

Special Article - Year 2014 - Volume 29 -
Dysmorphophobia: to be seen through someone else's eyes
Dismorfofobia: o olhar do outro
ABSTRACT
The modern modus vivendi has promoted a growing discontentment in regard to self body image, and imagining a perfect body leads to a desire in an individual that is not always compatible with reality. With no limits in transfiguration, the body is modeled based on the dream of a perfect body structure, which is most times unattainable and requires numerous proposed surgical procedures. Therefore, it is of utmost importance for plastic surgeons to become aware of Body Dysmorphic Disorder (BDD), or dysmorphophobia. This is a disorder that is prevalent in both sexes, in which self visual appearance is distorted. It is also characterized by an excessive concern over a tiny physical imperfection or delusive physical imperfections. The diagnosis can remain unnoticed due to lack of knowledge, misdiagnosis, or concern only over body alterations, which may lead to personal damage, legal claims, and also risk of prolonging the disorder.
Keywords: Dysmorphophobia; Body dysmorphic disorder; Plastic surgery; Body image; Somatoform disorders.
RESUMO
O modus vivendi moderno tem produzido cada vez mais um crescente descontentamento em relação à anatomia corporal e a imaginação a respeito do corpo perfeito desperta um desejo no indivíduo nem sempre condizente com sua realidade. Sem limitação para as transfigurações, o corpo é modelado com base no sonho de uma estrutura corporal perfeita, na maioria das vezes, inalcançável, com os inúmeros procedimentos cirúrgicos propostos. Assim, é fundamental que os cirurgiões plásticos conheçam o Transtorno Dismórfico Corporal (TDC) ou dismorfofobia, desordem esta prevalente em ambos os sexos, em que a visão da aparência é deturpada, caracterizada pela inquietação excessiva de uma imperfeição física minúscula ou por imperfeições corporais ilusórias. O diagnóstico pode passar despercebido pelo não conhecimento, pelo subdiagnóstico ou pela preocupação apenas com a alteração corporal, o que pode trazer prejuízos pessoais, demandas jurídicas e até ajudar a manter o distúrbio.
Palavras-chave: Dismorfofobia; Transtorno dismórfico corporal; Cirurgia plástica; Imagem corporal; Transtornos somatoformes.
Body image concerns used to be a predominantly female issue; however, in recent years, men have also become concerned with their body images. Discontentment with physical image is the main reason for most psychiatric disorders and is especially important for plastic surgeons to consider. Dysmorphophobia, or Body Dysmorphic Disorder (BDD)1, exposes the surgeon to a pathology that is little known, understudied, and so far under-diagnosed.
With the economic improvements occurring in Brazil and worldwide, plastic surgery, which was previously seen as being restricted to just some individuals, became available to members of the population who did not previously have access to such a service, resulting in aesthetic and functional improvements. Most plastic surgeons have decreased their holistic view of the patient and have started to worry more about specific forms or distortions, rather than the "whole" view. This fact, in addition to the manifestations of a patient with BDD, comprises a perfect combination for failure of surgery and the beginning of a series of dissatisfactions experienced by both patient and surgeon.
Dysmorphophobia is a Greek word meaning ugliness, especially in the face, which was used for the first time a hundred years ago by Morselli1; however, the first reference to this concept appeared in Herodotus's Histories, in the myth of the "The Ugly Girl from Sparta," who was taken every day by her family to the temple to free herself from her lack of beauty and attractiveness.
There are many different names used to describe it, such as beauty disease, body image distortion syndrome, aesthetic hyper valorization, globalization of beauty, and standardization of forms; however, this condition is best described as a somatoform disorder, characterized by excessive concern over repairing a defect. Most of the time, this defect is either imaginary or trivial in its physical characteristics, but it is capable of creating emotional stress that can lead to the damaging of social, professional, and/or affective interactions. However, in 1987, a mere century after being first described, dysmorphophobia classified as an atypical somatoform disorder and was entered into the Diagnostic and Statistical Manual of Mental Disorders (DSM-III-R), currently in its fourth edition. In Brazil, the first reference to this disease appeared in a work published in 1976 by Pitanguy et al., which raised the importance of psychological and psychiatric issues in plastic surgery.
In 2009 alone, more than 600 thousand aesthetic surgeries were performed in Brazil, which makes us wonder what percentage of this sample could represent BDD. Has this disorder been under-diagnosed and overlooked?
OBJECTIVE
The objective of this work is to present, through a bibliographic review and personal evaluations, some relevant information to help the plastic surgeon in regard to dysmorphophobia, its diagnosis, its treatment, and the clinical management of patients carrying this mental alteration, since these cases are increasingly present in the plastic surgery practice.
BODY DYSMORPHIC DISORDER AS DISEASE
This pathology, despite not being much investigated, was described more than a century ago, with several cases being reported, attesting to the potential problems associated with continuous plastic surgeries. Even if it is used in different ways, this term comprises excessive concern over a small or delusive defect in regard to body image; i.e., a feeling of ugliness perceived by the patient2,3.
According to Fontenelle2, body dysmorphic disorder is described by Phillips as "a new name given to an old syndrome." Torres et al.4,5 note that the BDD definition is based on the distortion of perception manifested as anxiety, obsession, or overvalued or excessive thoughts in regard to body form or to some specific parts of the body6,7. It is multicausal in origin and includes biological, genetic, psychological, and even cultural and/or environmental factors that combine in a way that is still unclear. It equally affects men and women, despite the fact that women naturally show a higher concern with their body image compared to men, which is the reason why women search for plastic surgery, and demand better results, more frequently. In men, the disease can present itself as vigorexy, which corresponds to the muscle dysmorphia disorder, or "academy syndrome," concern with hair loss, dental changes, and even with biotype. Its peak is manifested in adolescence. It shows a floating trend, progressive worsening throughout the years in cases in which treatment has not been established.
Some studies have evaluated dysmorphophobic patients in samples from the general population, indicating an incidence of 1 to 7%, in Germany, and 2 to 4% in the USA8-11. Among plastic surgery patients, studies revealed that the incidence varies between 7 and 8% in the USA12,13, and 6.3 to 9.1%, in Europe13-15. In Brazil, it is believed that the numbers are similar to the worldwide incidence; however, there is no way to measure such data.
Hodgkinson16 stated that individuals dissatisfied with plastic surgery results may show body dysmorphic disorder. Overall, studies with individuals who have great concerns over their body images and who searched for aesthetical, dental, and plastic surgery treatments to improve them showed rates of 3 to 15%17-19. Sarwer et al.13 analyzed one hundred individuals who were subjected to aesthetical surgery and identified dysmorphophobia in 7%, a higher percentage than that reported by Andreasen & Bardach, which was 2% among the same type of population20. Warnick9 reported that previous evidence indicated that dysmorphophobia is regularly diagnosed with equal incidence among both sexes. Additionally, studies by Connolly & Gipson and Hay found the same rates between the two sexes2,5,11,21,22.
The first signs usually occur in the beginning of adolescence and extend until approximately the age of 20 years, because it is during this period that several body development problems occur6,14,18,21. In dysmorphophobia, the individual demonstrates exaggerated concern over a small physical abnormality, which causes great suffering at a clinical level and damage to social and professional interactions, and to other important areas of the patient's life, leading to relevant morbidity22,23.
Many of these individuals live isolated at home for many years, many progress with significant social and professional losses, and most of them seek surgical or aesthetical treatment, without psychological support, which clearly results in failure24-26. Often, patients with dysmorphophobia seek and find surgical treatment or a doctor with the aim of correcting their fictitious defects; however, they continue to treat their body, or parts of their bodies, with discrimination. Therefore, treatment may result in an increase of body image obsession or may promote new concerns, which may then result in many unsuccessful surgeries that leave these individuals dissatisfied.
The suffering BDD may cause has been well documented in the literature. It can result in social and marital problems that completely disassemble the life of an individual, and it can even lead to thoughts of suicide. This may occur as a result of the time spent by some individuals on their afflictions, which is time spent disregarding other areas of their lives.
DIAGNOSIS
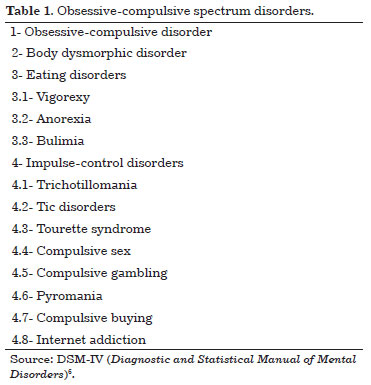
The wish for a perfect body image does not imply that one suffers from a mental disease, but it increases the possibilities that these disorders may occur and should, therefore, be regarded as a disease. The Diagnostic and Statistical Manual of Mental Disorders IV (DSMV-IV) describes the disease as belonging to the obsessive-compulsive spectrum, like bulimia and anorexia, and stipulates relevant diagnostic criteria (Table 1). In some cases, the diagnosis is difficult if the disease manifests itself along with other mental disorders7.
Deformity, which is insignificant to other individuals, is apprehended by the patient as devastating and causes stress, anxiety, and apprehension, which leads the patient to incessantly, and unwisely, seek physical perfection and harmony1,5,11,19. It also causes apprehension, displeasure, exaggeration in the perception of the deformity, significant degeneration in social and occupational performance, and anguish.
The diagnosis is based on a clinical consultation, since many of these patients will show anxiety, perfectionism, low self-esteem, and introversion, and their complaints may change over time. It may be associated with other diseases, such as anxiety-depressive disorder and phobias (panic syndrome), with suicidal ideation being present in up to 80% of the patients. The most serious cases may lead to progressive functional incapacity and social isolation.
Usually, the complaints are based on illusory or minimal defects in the head or face, such as acne, swelling, scars, wrinkles, excessive hair, lack of hair, disproportionate or lack of face symmetry, and form and/or size of the nose, eyes, mouth, eyebrows, ears, teeth, chin, mandible, and cheek. However, any part of the body may be cause for distress, such as the genitals, abdomen, buttocks, hips, and shoulders, and this can also comprise a group of various body parts26-28,.
Some common behaviors are frequently observed in these patients, such as comparing the defected part with that of others; looking at the defect repeatedly in the mirror or reflective surfaces, despite generally avoiding looking at it in order to decrease discomfort and concern; thinking about it often throughout the day and letting those thoughts dominate their lives; not taking pictures of themselves; using clothes, hats, and excessive makeup to disguise the imperfection; using their hands or posture to hide the defect; performing elaborate rituals to take care of their appearance; excessively searching for information about the "defected" part of the body; seeking surgery or medical treatment in spite of contrary recommendations; looking for confirmation in regards to the defect or trying to convince others that it is abnormal; avoiding social events in which the imperfection may be noted; experiencing social phobia due to the defect; feeling social isolation; and showing introversion and low self-esteem. In severe dysmorphophobia cases, the patients may quit school, jobs, or even avoid leaving the house altogether23,24,29-31. Some indicators of dysmorphophobia are as follows: feelings of discomfort when in public, excessive concern and negative evaluations of one's appearance, tendency to overrate appearance when determining self-worth, avoiding social circumstances and physical contact with others, and excessive alteration of appearance through clothes and cosmetics6,25-27,30.
According to the DSM-IV, the criteria required to diagnose dysmorphophobia are as follows: (a) concern with imaginary body image defects or excessive concern over a small physical defect (b) significant disruption or damage in social or occupational functioning or in other important areas due to the excessive concern; and (c) the inability to attribute the concern to another mental disorder, such as anorexia nervosa6.
Patients with a dysmorphophobia profile are usually shy, susceptible to rejection, socially impatient, and perfectionistic. Most of them have problems with depression, and these are frequently manifested through intense anguish or feelings of inferiority, as exhibited by very severe eating disorders.
In addition, these patients can perform an adequate self-evaluation, under a doctor's request, by excluding what disturbs them the most. If they excessively overrate a small defect, their confidence may be destroyed. Even in the presence of a large amount of evidence against the perceived imperfection, the patient completely believes in its existence and cannot stop worrying, although these worries are groundless13,15,31-33.
According to Bárbara Machado34, patients may assume one of the four temperament forms described by Ferreira35. Such a personality type indicates the direction of post-surgery recovery and expectation levels regarding treatment. Thus, the following personalities may be seen among dysmorphophobic patients:
- Choleric patients are determined, dominant, impulsive, and tend to take charge of the situation. If the input by the doctor contradicts their expectations, they argue against it. If the doctor insists, they may not even follow indications and may end up searching for another professional who will support their ideas. In these situations, to eliminate challenges, conducting the dialogue in a way so that the patient feels stimulated and thinks in a different way and observes new aspects related to him and to his deformity may be a good approach, although this would require additional free time or even more consultations.Obviously, it is difficult to find patients that manifest only one of the four above described temperaments; nevertheless, there is always the predominance of one, and knowing how to deal with the patient greatly increases the chances of success35. The dysmorphophobic patient may assume any of the four temperaments. This will differ according to personality. However, there are some questions that can be asked to a patient suspected of having dysmorphophobia during consultations:
- Phlegmatic patients are calm observers, passive, deductive, and usually accepting of the input given to them by the doctor. They think in a methodical and careful way, seek new data that will allow them to better evaluate the situation, and may also require more time to digest everything they hear. It is important to make available to them all data and information that they might require.
- Melancholic patients are sensitive, emotional and intuitive. They generally develop a small number of relationships, however deep. Special care should be given when informing them, in particular when the information given may generate some sort of fear or anxiety, since they tend to become depressed. They need to be assured that the doctor is someone they can count on, who will offer them all the possible resources to deal with the situation.
- Sanguine patients are labile, seductive, attractive, and of easy and numerous relationships; however, they tend to be shallow. They will probably easily accept the arguments and directions given by the doctor, which does not mean they are completely convinced by what the doctor said. They may not correctly follow all the instructions, claiming forgetfulness and lack of time or excessive activities, among other excuses. If the doctor identifies the predominance of this temperament in a patient, it is important not to criticize, but to see to it, in a calm and firm way, that the patient gains self-awareness and follows instructions33,35.
1- Was any "problem" or alteration identified? Can the surgeon treat the patient?Based on the replies obtained, the plastic surgeon may infer the type of patient when approaching him/her, but it should be noted that the diagnosis may often be overlooked if the doctor focuses only on the body change of the patient, giving no emphasis to adequate clinical and psychological examinations, since approximately 10% of plastic surgery patients show some level of dysmorphophobia. Although it has been described in different ways in the literature, such a topic remains unclear to numerous medical colleagues who do not diagnose these patients and subject them to surgical procedures that, in addition to not bringing benefits, do not solve the problems pointed out by the patients.
2- Is the patient manageable? Would the doctor like to have the patient in his office?
3- In case of complications, will the patient cooperate?
4- Does the patient understand the margin of error associated with the procedure?
HOW TO TREAT DYSMORPHIC PATIENTS
Besides having been reported more than one hundred years ago, and being the cause of much suffering, dysmorphophobia is believed to be adequately treated in only 10% of all cases17,18. Usually, treatment consists of a combination of antidepressant drugs, which help in decreasing depression symptoms, and psychotherapy, which increases safety and confidence. Applied together, these methods help the patient dominate their obsessions and anxiety, which are related to body image21,22. With the aid of antidepressant drugs, the patients are able to decrease their concerns, their feelings of discomfort, and behavioral rituals, and improvements in social and occupational behavior are observed. Although the defect is still noted, because it never stops being a defect, in a general way it will cause less discomfort1,13,17,18,31.
In cognitive-behavioral therapy, the methods applied include self-monitoring thoughts; checking the time spent in front of the mirror; trying to change thoughts about body image, if in a social situation; and preventing and avoiding compulsive behaviors25,31,35. The surgery does not bring benefits to this group of patients and is contraindicated, since due to the image distortion, even the most beautiful result will still not meet their expectations, which are, in fact, unsurpassable.
CONCLUSIONS
Dysmorphophobia, or body dysmorphic disorder, was described for the first time in 1886 as being a "subjective feeling of ugliness or physical defect in which patients feel that they are being observed by a third party, although their appearance is considered within normal limits."4 Thus, the body is a cause of much suffering, being rejected and considered worthless without passion and, as a result, submitted to unnecessary extreme procedures or isolation and neglect. Usually, this condition is not diagnosed because doctors do not adequately research patients' complaints or because they tend to worry with only somatic alterations.
The dysmorphic patient lives in constant stress because he cannot control the disturbances associated with his negative body image, which he believes he possesses, even when he is assured that all is well and the defect is insignificant, minimal, or nonexistent. It is a concern that damages his comprehension or body recognition. These disturbances distort the image that the patient has of himself, leading him to be obsessed with a perfect body image and transforming small imperfections into real monstrosities, which causes much suffering and social, occupational, and familiar isolation. With the aim of changing their appearances, patients with dysmorphophobia seek treatment from diverse professionals, including plastic surgeons; subsequently, after being dissatisfied with the results, they undergo new procedures for the same complaint or for a different part of the body that becomes then the new focus of attention14,16,18,21.
It is of the utmost importance that health services professionals know how to recognize the symptoms of dysmorphophobia and thoroughly investigate the disturbances presented by the patients before any procedures are administered. It is essential to underline that the plastic surgeon may have some difficulties in identifying dysmorphophobia, and since dysmorphic patients create delusional expectations of the aesthetic procedures - and generally are not satisfied with them - they may hold the doctor responsible for it, which can lead to legal claims.
A plastic surgeon uninformed in respect to dysmorphophobia may cause personal damage or even help to prolong the disorder of the patient over time, while the procedures are being performed. This professional will be faced with a psychologically altered patient who, in the post-operative phase, is dissatisfied, returns frequently to the doctor's office showing baseless complaints, and even proposes the need for new surgical procedures as a form of "mitigating" his dissatisfaction with the recently performed procedure.
Surgery is formally contraindicated for these patients, since, besides not being in agreement concerning their expectations, the disorder may worsen, which can result in legal claims, or verbal, or even physical, aggression. The treatment is based on specialized monitoring by a psychiatrist and psychologist, and drugs are prescribed in order to help treat anxiety and obsession.
REFERENCES
1. Pavan C, Simonato P, Marini M, Mazzoleni F, Pavan L, Vindigni V. Psychopathologic aspects of body dysmorphic disorder: a literature review. Aesthetic Plast Surg. 2008;32(3):473-84. http://dx.doi.org/10.1007/s00266-008-9113-2. PMid:18224271
2. Fontenelle LF. Actualizacion y Revision del Trastorno Dismorfico Corporal. Trabajos Distinguidos. Salud Ment. 2004;7(6):67-71.
3. Dufresne RG, Phillips KA, Vittorio CC, Wilkel CS. A screening questionnaire for body dysmorphic disorder in a cosmetic dermatologic surgery practice. Dermatol Surg. 2001;27(5):457-62. PMid:11359494.
4. Morselli E. Dysmorphophobia and taphephobia: two hitherto undescribed forms of Insanity with fixed ideas. Hist Psychiatry. 2001;12(45):107-14. http://dx.doi.org/10.1177/0957154X0101204506.
5. Torres AR, Ferrão YA, Miguel EC. Transtorno dismórfico corporal: uma expressão alternativa do transtorno obsessivocompulsivo? Rev Brasileira de Psiquiatria. 2005;27(2):95-6.
6. AMERICAN PSYCHIATRIC ASSOCIATION - APA. Diagnostic and Statistical Manual of Mental Disorders DSM-IV-TR. 4. ed. Washington: American Psychiatric Association; 2002.
7. ORGANIZAÇÃO MUNDIAL DA SAÚDE - OMS. Classificação Estatística Internacional de Doenças e Problemas Relacionados a Saúde. 10. rev. São Paulo: Edusp; 2007.
8. Koran LM, Abujaoude E, Large MD, Serpe RT. The prevalence of body dysmorphic disorder in the United States adult population. CNS Spectr. 2008;13(4):316-22. PMid:18408651.
9. Warwick HMC. Transtornos somatoformes y factícios. In: Caballo VE, Buella Casal G, Carrobles C, orgs. Manual de Psicopatologia y transtornos Psiquiátricos. Madrid: Siglo Ventiuno Editores de España; 1996. p. 404-64.
10. Ruffolo JS, Phillips KA, Menard W, Fay C, Weisberg RB. Comorbidity of body dysmorphic disorder and eating disorders: severity of psychopathology and body image disturbance. Int J Eat Disord. 2006;39(1):11-9. http://dx.doi.org/10.1002/eat.20219. PMid:16254870
11. Rief W, Buhlmann U, Wilhelm S, Borkenhagen A, Brähler E. The prevalence of body dysmorphic disorder: a populationbased survey. Psychol Med. 2006;36(6):877-85. http://dx.doi.org/10.1017/S0033291706007264. PMid:16515733
12. Javaras KN, Pope HG Jr, Lalonde JK, Roberts JL, Nillni YI, Laird NM, et al. Co-occurrence of binge eating disorder with psychiatric and medical disorders. J Clin Psychiatry. 2008;69(2):266-73. http://dx.doi.org/10.4088/JCP.v69n0213. PMid:18348600
13. Sarwer DB, Crerand CE. Body dysmorphic disorder and appearance enhancing medical treatments. Body Image. 2008;5(1):50-8. http://dx.doi.org/10.1016/j.bodyim.2007.08.003. PMid:18255365
14. Aouizerate B, Pujol H, Grabot D, Faytout M, Suire K, Braud C, et al. Body dysmorphic disorder in a sample of cosmetic surgery applicants. Eur Psychiatry. 2003;18(7):365-8. http://dx.doi.org/10.1016/j.eurpsy.2003.02.001. PMid:14643566
15. Altamura C, Paluello MM, Mundo E, Medda S, Mannu P. Clinical and subclinical body dysmorphic disorder. Eur Arch Psychiatry Clin Neurosci. 2001;251(3):105-8. http://dx.doi.org/10.1007/s004060170042. PMid:11697569
16. Hodgkinson DJ. Identifying the body-dysmorphic patient in aesthetic surgery. Aesthetic Plast Surg. 2005;29(6):503-9. http://dx.doi.org/10.1007/s00266-005-5033-6. PMid:16328637
17. Phillips KA, McElroy SL. Insight, overvalued ideation, and delusional thinking in body dysmorphic disorder: theoretical and treatment implications. J Nerv Ment Dis. 1993;181(11):699-702. http://dx.doi.org/10.1097/00005053-199311000-00009. PMid:8228952
18. Phillips KA, Albertini RS, Siniscalchi JM, Khan A, Robinson M. Effectiveness of pharmacotherapy for body dysmorphic disorder: a chart-review study. J Clin Psychiatry. 2001;62(9):721-7. http://dx.doi.org/10.4088/JCP.v62n0910. PMid:11681769
19. Phillips KA. The presentation of body dysmorphic disorder in medical settings. Prim psychiatry. 2006;13(7):51-9. PMid:17183412.
20. Bienvenu OJ, Samuels JF, Riddle MA, Hoehn-Saric R, Liang KY, Cullen BA, et al. The relationship of obsessive-compulsive disorder to possible spectrum disorders: results from a family study. Biol Psychiatry. 2000;48(4):287-93. http://dx.doi.org/10.1016/S0006-3223(00)00831-3. PMid:10960159
21. Kittler JE, Menard W, Phillips KA. Weight concerns in individuals with body dysmorphic disorder. Eat Behav. 2007;8(1):115-20. http://dx.doi.org/10.1016/j.eatbeh.2006.02.006. PMid:17174859
22. Neziroglu F, Cash TF. Body dysmorphic disorder: causes, characteristics, and clinical treatments. Body Image. 2008;5(1):1-2. http://dx.doi.org/10.1016/j.bodyim.2008.03.001. PMid:18358798
23. Veale D. Advances in a cognitive behavioural model of body dysmorphic disorder. Body Image. 2004;1(1):113-25. http://dx.doi.org/10.1016/S1740-1445(03)00009-3. PMid:18089145
24. Buhlmann U, Reese HE, Renaud S, Wilhelm S. Clinical considerations for the treatment of body dysmorphic disorder with cognitive-behavioral therapy. Body Image. 2008;5(1):39-49. http://dx.doi.org/10.1016/j.bodyim.2007.12.002. PMid:18313372
25. Wolf J. Mirror mirror off the wall: a personal experience of intertwined obsessive/compulsive spectrum disorders: body dysmorphic disorder and trichotillomania. New York: New Harbinger Publications; 2003.
26. Assunção SSM. Dismorfia muscular. Rev Bras Psiquiatr. 2002;24(Suppl 3):80-4. http://dx.doi.org/10.1590/S1516-44462002000700018.
27. Phillips KA, Dufresne RG. Body dysmorphic disorder. A guide for dermatologists and cosmetic surgeons. Am J Clin Dermatol. 2000;1(4):235-43. http://dx.doi.org/10.2165/00128071-200001040-00005. PMid:11702368
28. Castle DJ, Phillips KA, Dufresne RG Jr. Body dysmorphic disorder and cosmetic dermatology: more than skin deep. J Cosmet Dermatol. 2004;3(2):99-103. http://dx.doi.org/10.1111/j.1473-2130.2004.00105.x. PMid:17147563
29. Grant JE, Phillips KA. Recognizing and treating body dysmorphic disorder. Ann Clin Psychiatry. 2005;17(4):205-10. http://dx.doi.org/10.1080/10401230500295313. PMid:16402752
30. Cotterill JA. Body dysmorphic disorder. Dermatol Clin. 1996;14(3):457-64. http://dx.doi.org/10.1016/S0733-8635(05)70373-9. PMid:8818555
31. Crerand CE, Phillips KA, Menard W, Fay C. Nonpsychiatric medical treatment of body dysmorphic disorder. Psychosomatics. 2005;46(6):549-55. http://dx.doi.org/10.1176/appi.psy.46.6.549. PMid:16288134
32. Marks I, Mishan J. Dysmorphophobic avoidance with disturbed bodily perception. A pilot study of exposure therapy. Br J Psychiatry. 1988;152(5):674-8. http://dx.doi.org/10.1192/bjp.152.5.674. PMid:3167444
33. Ramos KP, Amaral VLAR. Transtorno dismórfico corporal: escala para profissionais da área da saúde. Intellectus. 2008;4(5):1-27.
34. Machado BHB. Captação e fidelização do paciente ao cirurgião plástico: manual de boas práticas em cirurgia plástica. 1. ed. Rio de Janeiro: Editora DOC; 2012.
35. Caprara A, Franco ALS. A relação paciente-médico: para uma humanização da prática médica. Cad Saúde Pública. 1999;15(3):647-54.
1. Postgraduate Specialist, Lecturer at the Study and Research Center for Plastic Surgery, Mater Dei Hospital, Belo Horizonte, MG, Brazil
2. Resident of the Study and Research Center for Plastic Surgery, Mater Dei Hospital, Belo Horizonte, MG, Brazil
3. Resident of the Study and Research Center for Plastic Surgery, Mater Dei Hospital, Belo Horizonte, MG, Brazil
4. Second-year student of the Law course at the State University of Ponta Grossa (UEPG), Ponta Grossa, PR, Brazil
Institution: Work performed at the Mater Dei Hospital, Belo Horizonte, MG, Brazil.
Corresponding author:
Jorge Antônio de Menezes
Centro de Estudos e Pesquisas na Área de Cirurgia Pástica do Hospital Mater Dei
Rua Aimorés, 2480, sala 801 - Santo Agostinho
Belo Horizonte, MG, Brasil CEP 30140-072
E-mail: jorgeamenezes@uol.com.br
Article received: February 13, 2013.
Article accepted: March 10, 2013.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter