

Original Article - Year 2014 - Volume 29 -
Treatment of malar mounds and festoons
Tratamento da bolsa malar e festoons
ABSTRACT
INTRODUCTION: Changes to the malar region are, in many cases, difficult to resolve. The ageing process causes great variation and deformity of this region. Therefore, the aim of this study was to describe a simple and less aggressive surgical procedure that has demonstrated good results and quick recovery.
METHOD: A canoe-shaped or elliptical-shaped line is drawn bordering the malar mound or the skin fold. The skin is incised down to the subcutaneous plane. The excess skin is removed and a suture is then performed immediately.
RESULT: The patients undergoing this direct surgical method showed a favorable postoperative course, and the scars were not very visible.
CONCLUSION: This direct procedure provides a favorable result and quick recovery. Indications depend on surgical judgment, age of the patient, and degree of skin flaccidity.
Keywords: Eyelid; Blepharoplasty; Festoon; Malar mound.
RESUMO
INTRODUÇÃO: A alteração da região do malar, em muitos casos, é de difícil solução. O envelhecimento traz grande variação de deformidade na região. Neste sentido o objetivo do trabalho foi apresentar que procedimentos cirúrgicos com simplicidade e pouca agressividade têm demonstrado um bom resultado e rápida recuperação.
MÉTODO: Desenha-se uma figura em forma de canoa ou elíptica margeando a bolsa malar ou da dobra de pele. Em seguida realiza-se a incisão até o plano do subcutâneo. Retira-se a pele e logo após realiza-se a sutura.
RESULTADO: Os pacientes operados pelo método direto evoluíram de maneira convincente e com cicatrizes muito pouco visíveis.
CONCLUSÃO: é uma maneira direta e que traz resultado bastante favorável e rápida recuperação. A indicação esta relacionada ao bom senso do cirurgião, a idade do paciente e a flacidez existente.
Palavras-chave: Pálpebra; Blefaroplastia; Festoon; Bolsa malar.
The malar region is, aesthetically, an area subjected to a range of anatomical changes due to ageing. These alterations are very easy to identify since they are located in a visible region.
There are three alterations related to ageing that a surgeon may approach with precision. Ageing impacts facial appearance, and in the malar region, these alterations are characterized and classified as palpebral bags, malar mounds, and skin folds (festoons) (Figure 1).

Figure 1. Example.
Anatomical identification of these alterations is needed to achieve a satisfactory treatment outcome.
OBJECTIVE
In this paper, we describe a direct and simple procedure; however, much perspicacity and good judgment is required to choose the appropriate treatment method and achieve efficient results.
This study aimed to treat malar mounds and festoons.
METHOD
Among the available surgical techniques, we selected a direct technique based on a canoe-shaped incision for five patients aged 60 to 75 years.
Anesthesia was performed with 1% xylocaine infiltration, with or without vasoconstrictors depending on the case, with sedation monitored by an anesthesiologist.
A canoe-shaped or elliptical-shaped line was marked in the most prominent area of the malar region (Figures 2 and 3). The skin was incised down to the subcutaneous plane. The lower insertion of the malar ligament, which is usually located in this area, was removed. Then, hemostasis was performed and continuous sutures were performed in layers using 5.0 absorbable monofilament material.

Figure 2. Preoperative marking with canoe-shaped incision lines.
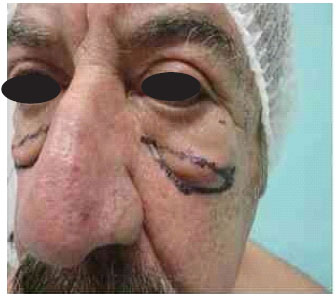
Figure 3. Preoperative marking with a canoe-shaped incision line, bordering the festoon.
RESULT
The direct approach with the canoe-shaped incision was shown to be a practical, simple, and quick technique to perform.
Patients who underwent surgery showed a favorable postoperative course. The resulting scar was visible during the first few days, and over the course of time, the scar became practically imperceptible (Figures 4, 5, and 6).

Figure 4. After 6 postoperative months.
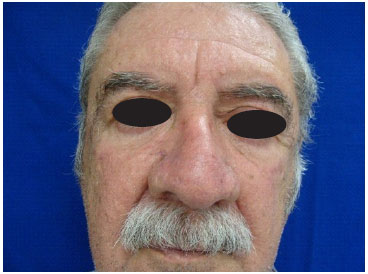
Figure 5. After 1 year postoperatively.
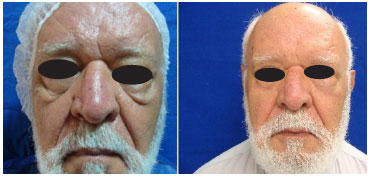
Figure 6. Preoperative image and after 6 postoperative months.
The complication of a large reddish edema was observed in one patient. Antibiotic therapy and spontaneous drainage resolved the edema and infection (Figure 7).
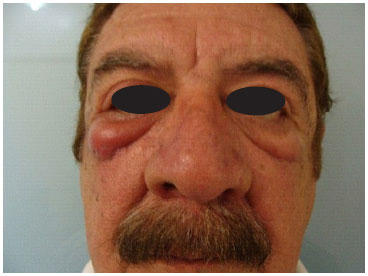
Figure 7. Postoperative complication (infection) that resolved with spontaneous drainage and antibiotic therapy.
DISCUSSION
Each anatomical alteration requires a specific treatment technique.
The classical blepharoplasty techniques aim to improve and correct the function, form, and aesthetic aspect of eyelids. Certainly, these are among the most performed procedures in plastic surgery. Generally, these procedures provide good results, but despite being apparently simple to perform, a great and diverse potential for the occurrence of complications remains, and it is not always possible to correct all the abnormalities of the region1,2,3.
The anatomy of the malar mounds, which are also referred to as malar pads, has already been described. The main factor contributing to this condition is increasing laxity of the malar ligament. The malar ligament originates in the upper part of the orbital rim periosteum and inserts itself inside the skin at 2.5 to 3cm below the level of the lateral canthus, which allows the accumulation of fluid above the level of its insertion in the skin. This structure acts as a relatively impermeable fibrous membrane, and is responsible for the accumulation of liquid in the region4.
The malar mounds may become aggravated due to chronic eyelid swelling, which over time becomes a festoon5. This condition develops due to orbicularis muscle attenuation, with occurrence of laxity in the bonding system between muscle and deep fascia, forming skin folds6.
Several techniques and methods to treat malar mounds and festoons have been described in the literature. Malar pads or mounds have posed difficulties to plastic surgeons when conducting the corrections. The current surgical approaches used to improve this characteristic of facial aging are the following: blepharoplasties, vertical suspension of the face, rhytidoplasties, CO2 laser, lipoaspiration, and direct skin incision. All the above-mentioned techniques have advantages and disadvantages with regard to outcomes. The lower blepharoplasties are generally unsatisfactory, even in cases where the extended flap of the orbicularis muscle is used, being more appropriate for the correction of lower baggy eyelids7. When the festoon is large, static vertical suspensions cannot completely correct skin laxity8. Lipoaspiration of the region is used to conceal the malar edema and small mounds of the malar9. Usually, this is indicated in young patients. Photothermolysis via CO2 laser is another method of treatment that can be used, which promotes an effective modification of the skin10. This method should only be used when surgically indicated; to use this type of incision in a young person is not recommended, since the scar resulting from this procedure will undoubtedly be visible.
CONCLUSION
The above-mentioned approach with a canoe-shaped incision is very promising. It is a simple technique that does not require special care, and has a satisfactory outcome, and the scar gradually becomes imperceptible. This technique is indicated for patients with increased laxity in the region, particularly patients above the 60 years of age who have the skin alterations described above.
REFERENCES
1. Jaimovich CA, Medeiros R. Blefaroplastia convencional. In: Mélega JM, ed.Cirurgia Plástica: fundamentos e arte. Cirurgia estética. Rio de Janeiro: Medsi; 2003. p.105-16.
2. Lessa S. Blefaroplastia não convencional. In: Mélega JM, ed. Cirurgia Plástica: fundamentos e arte. Rio de Janeiro: Medsi;2003 p.123-117.
3. Farrapeira AB. Abordagem segmentar do terço médio da face. Triângulo na região geniana: ponto de sutura dermogorduroso. Rev Bras Cir Plats. 2009;24(4):497-503.
4. Pessa JE,Garza JR. The malar septum the anatomic basis of malar mounds and malar edema. Aesthet Surg J.1997;17:11-17.
5. Hoenig JF, Knutti D, Fuente A. Vertical Subperiosteal Mid-face-lifts for Treatment of Malar Festoons. Aesth Plast Sur.2011;35:522-529.
6. Furnas DW. Festoons of orbicularis muscle as a cause of baggy eyelids. Plast Reconstr Surg.1978;61:540-546.
7. Sherrel JA,Walden JL,Freund RM. Blefaroplastia In:Castro CC. Ritidoplastia Arte e Ciência. Rio de Janeiro; Di Livros;2007. P 235.
8. Chang YC. Reposicionamento do terço médio da face na cirurgia da face: uma técnica simples de suspensão e fixação. Rev Bras Cirur Plas. 2008;23(2):71-74.
9. Rosenberg GJ. Correction of saddlebag deformity of the lower eyelids by superficial suction lipectomia.Plast Reconstr Surg.1995;96:1061.
10. Lessa S, Sebastiá R, Flores E. Estudo Histológico das Mudanças Estruturais da Pele Fina Palpebral após a fototermólise Seletiva com Laser de CO2.Rev Bras Cirur Plast. 199914(2):7-20.
Full Member of the Brazilian Society for Plastic Surgery - Director of the Institute for Specialized Surgery Ltda
Institution: Institute for Specialized Surgery Ltda. (ICEL), Israel Pinheiro Institute.
Corresponding author:
Adilson Branco Farrapeira
SHIS QI 26 - Conj. 3 - Casa 20 - Lago Sul
Brasília, DF, Brazil Zip code: 71670- 030
E-mail: abfarrapeira@ig.com.br
Article submitted: October 1, 2013.
Article accepted: January 25, 2015.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter