

Original Article - Year 2014 - Volume 29 -
Refinement of the Mustardé technique for the treatment of prominent ears
Refinamento da técnica de Mustardé para o tratamento das orelhas proeminentes
ABSTRACT
INTRODUCTION: Traditionally, multiple abnormalities can cause prominent ears, and specific techniques have been developed for the treatment of each abnormality. In this study, we tested a single approach aimed at achieving satisfactory outcomes.
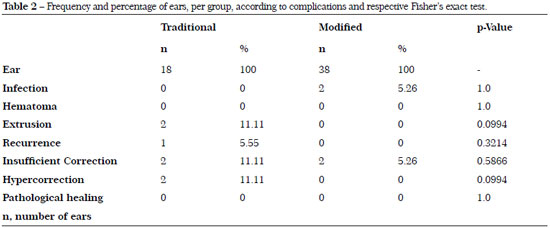
METHOD: Patients submitted to bilateral otoplasty, between June 2010 and December 2012, were retrospectively evaluated and divided into two groups: group 1 - patients submitted to the conventional Mustardé technique and group 2 - those who underwent the modified Mustardé technique. For comparison, we collected data relating to early and late complications, requirement for a new surgery, and degree of patient satisfaction. Statistical analysis was performed with Fisher's exact test.
RESULTS: Group 1 included nine patients treated with the conventional Mustardé technique. A case of suture extrusion (11.11%) was observed. Seven patients reported to be very satisfied, one satisfied, and one dissatisfied because of insufficient correction and a subsequent need for a second surgery. Group 2 included 19 patients submitted to the modified Mustardé technique, which involved three sutures in the middle third of the ear and the posterior rotation of the vertex of the antihelix. One case of bilateral infection (5.26%) was observed. Seventeen patients reported to be very satisfied, one satisfied, and another dissatisfied because of insufficient correction, thus needing to undergo a second surgery. No statistical difference was observed between the two groups.
CONCLUSION: The identification of the basic abnormality associated with prominent ears allows performing a single approach that is easy to learn and implement, in addition to providing good outcome (i.e., natural appearance) and a high degree of patient satisfaction.
Keywords: External ear/abnormalities; Plastic surgery; Results evaluation; Postoperative complications.
RESUMO
INTRODUÇÃO: Tradicionalmente, múltiplas anomalias podem causar as orelhas proeminentes e foram desenvolvidas técnicas específicas para o tratamento de cada deformidade. Neste trabalho, testou-se uma abordagem única para alcançar resultados favoráveis.
MÉTODO: Foram avaliados, retrospectivamente, os pacientes submetidos a otoplastia bilateral entre junho de 2010 e Dezembro de 2012, divididos em dois grupos: Grupo 1 - técnica convencional de Mustardé e Grupo 2 - Refinamento da técnica de Mustardé. Para comparação foram coletados os dados referentes às complicações precoces, tardias, à necessidade de reoperação e ao grau de satisfação do paciente. A análise estatística foi realizada através do teste exato de Fisher.
RESULTADOS: No Grupo 1 foram incluídos 9 pacientes tratados com a técnica tradicional de Mustardé. Houve um caso de extrusão de pontos (11,11%). Sete pacientes ficaram muito satisfeitos, um satisfeito e um insatisfeito por correção insuficiente, sendo reoperado. No Grupo 2 foram incluídos 19 pacientes submetidos a uma variação da técnica de Mustardé com 3 suturas no terço médio da orelha, rotacionando posteriormente o vértice da antélice. Houve um caso de infecção bilateral (5,26%). Dezessete pacientes ficaram muito satisfeitos, um satisfeito e outro insatisfeito por correção insuficiente, sendo reoperado. Não houve diferença estatística entre os grupos.
CONCLUSÃO: A identificação da alteração básica relacionada com orelhas proeminentes permite uma abordagem única, de fácil aprendizado e execução, com resultados de aparência natural e elevado grau de satisfação do paciente.
Palavras-chave: Orelha Externa / Anormalidades; Cirurgia Plástica; Avaliação resultados; Complicações pós-operatórias.
Although prominence of the ear is the most common congenital deformity in this organ1, there is no consensus in the literature about the definition of this condition. Several authors2 define prominent ear as the presence of a >2 cm distance between the helical edge and the point directly perpendicular to the mastoid. The prevalence of prominent ears is approximately 5%3; it and mainly affects the Caucasian population, with no sex preponderance and with a pattern of autosomal dominant genetic transmission of different degree of penetration4.
The ear measures 5-7 cm, reaching between 85% and 95% of its adult size from the age of 3 and 7 years, respectively2. The most appropriate age for the correction of fan-like ears is around 5 to 6 years, when the formation of the pavilion is almost complete. Correction of the abnormality during this preschool age will enable avoiding the psychological, emotional, and behavioral consequences of this abnormality on the child, e.g., being bullied by peers5.
As in other facial procedures, the ideal surgery is one that will result in a natural and long-lasting postoperative aesthetic appearance. Specifically in otoplasty surgeries, this consists in providing a graceful curvature to the helicoid and antihelical contours, and rendering them symmetrical to the opposite ear6. In 1968, McDowell specified the basic surgical goals in otoplasty7: 1) all traces of protrusion in the upper third of the ear must be corrected (a little protrusion remaining in the middle and lower third may be acceptable as long as the upper portion is properly corrected; the reverse is not acceptable); 2) frontally, the helix of both ears should be seen beyond the antihelix (at least in the upper half but preferably throughout the ear); 3) the helix must have a regular and smooth profile through all its extension; 4) the postauricular groove cannot be superficial or distorted; 5) the ear should not be too close to the skull, especially in boys (the posterior measure between the outer edge of the helix and the skin of the mastoid region should be 10-12 mm in the upper, 16-18 mm in the middle, and 20-22 mm in the lower third, respectively); 6) the position of both ears (i.e., the distance from the lateral edge to the head) should be very similar, with a difference of <3 mm at any height.
Traditionally, the abnormalities causing prominent ears include an undefined antihelix fold, conchal hypertrophy, increased concho-mastoid angle, and anterior lobe projection6. Since its first description by Dieffenbach in 1848, several techniques have been developed for the specific treatment of each abnormality8,9. Besides being possible, the combination of these techniques has the theoretical advantage of enabling the surgeon to perform an individualized approach for each patient1. The literature describes >200 otoplasty procedures4 whose possible combinations render the teaching and the comparison of the results extremely difficult between different treatment centers.
Influenced by the logical principle of Ockham's razor, attributed to the English Franciscan friar William of Ockham (XIV century), which states that the best explanation must consist in strictly necessary premises (i.e., eliminating secondary assumptions), or that simple approaches should be selected over complex procedures, we established the hypothesis that antihelix malformation is the basic premise for the formation of fan-like ears and that a single surgical strategy would allow achieving the same satisfactory outcome when compared with traditional treatment combinations.
Therefore, in this study, we tested a single approach with the aim to achieve good outcomes and patient satisfaction.
METHOD
We retrospectively evaluated all patients submitted to bilateral otoplasty, between June 2010 and December 2012, at the private clinic of the author, who gradually replaced conventional techniques with the modified Mustardé technique. The study followed the ethical principles of the Declaration of Helsinki. Six months after study inclusion, the medical records as well as the pre- and postoperative images of patients, monitored for a minimum of 6 months, were analyzed. Then, the patients were divided into two groups: group 1 - patients submitted to the conventional Mustardé technique and group 2 - those who underwent the modified Mustardé technique.
For comparison, we collected data on different complications (infection, hematoma, skin dehiscence, recurrence, asymmetry, and suture extrusion), the need for an additional procedure, and subjective analysis, based on the degree of patient satisfaction rated on a scale from 1 to 4 (1 - very dissatisfied, 4 - very satisfied).
In group 1 patients, the Mustardé technique was carried out through an incision in the postauricular groove, detachment of the skin flap in the direction of the helix, generation of four to five posterior sutures to shape the new antihelix along the upper two-third of the ear, and resection of the excess skin spindle.
In group 2 patients, the Mustardé technique8 was modified by using three "U" sutures with 3-0 colorless nylon, to define the transition of the antihelix from the middle and lower third, until it shifts between the middle and upper third of the ear (Figure 1A). Through a linear incision of approximately 4 cm in the posterior projection of the antihelix (Figure 1B), we were able to detach the skin enough to demarcate the cartilage. Then, with a 21G needle, we transfixed the cartilage from an anterior to a posterior direction (Figure 1C), staining with methylene blue the locations where the "U" sutures would have been placed (Figure 1D and E). We then found the support for the two lower points, which were approximately 3 mm closer to the conchal cartilage when compared with the traditional technique. Our aim was to bend it and posteriorly rotate its upper edge, thus contributing to a better definition of the antihelix and, at the same time, decreasing the conchal size (Figure 1F). Colorless nylon sutures were left progressively looser in the cranial direction (Figure 2A). Mustardé sutures were not used in the upper third of the ear. The posterior skin was sutured, without tension (Figure 2B), with 5-0 hidden black nylon thread, in the posterior antihelix groove (Figure 2C). Between the first and second ear, fan correction can be seen (Figure 2D). Figure 2E shows the symmetry between the ears at the end of the surgery. The patients were instructed to wear an elastic band over the ears for a month, and the sutures were removed after 2 weeks.
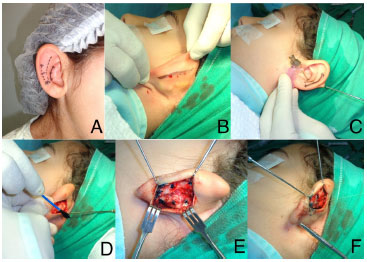
Figure 1. (A and B) Preoperative marking in the modified Mustardé technique. (C-F) Technical marking and preparation for the shaping sutures.

Figure 2. Shaping aspect (A) and posterior suture (B and C). Final unilateral (D) and bilateral (E) aspect of the surgery performed with the modified Mustardé technique.
Both groups did not present any difference concerning ear deformities at clinical examination.
The statistical analysis between the groups in terms of rate of complications, reoperation, and degree of patient satisfaction was done by applying Fisher's exact test, with the aim of verifying the association between two categorical variables. The statistical analysis was conducted with the GraphPad Prism® 5.0 software, with the level of significance set at p<0.05.
RESULTS
Thirty-five patients were included in the study.
Group 1 included nine patients, for a total of 18 ears operated. The patients were aged between 6 and 52 years (average, 21.5 years) and submitted to the conventional Mustardé technique. One patient (11.11%) presented bilateral extrusion of Mustardé sutures, and one (3.12%) patient was reoperated for unilateral recurrence (Figure 3). Seven patients (77.77%) reported being very satisfied; one patient (11.11%) was satisfied but was not willing to undergo reoperation (Figure 4); and one patient (11.11%) was dissatisfied and considered the correction inadequate, and was therefore reoperated after 6 months.

Figure 3. Patient from group 1 (traditional treatment) with unilateral recurrence (center); reoperation was performed after 6 months (right).

Figure 4. Patient from group 1 (traditional treatment) who reported satisfaction about the hypercorrection of the upper antihelix; however, this patient was not willing to undergo reoperation and thus was lost to follow-up.
Group 2 included 19 patients, for a total of 38 ears operated. The patients were aged between 6 and 62 years (average, 25.4 years). One case (5.26%) of bilateral infection was observed and clinically treated, whereas no cases of suture extrusion were detected (Table 1). Seventeen patients (89.47%) reported to be very satisfied (Figure 5 and 6); one patient (5.26%) was satisfied; and another patient (5.26%) was dissatisfied (desiring the upper third of the ear to be closer to the pavilions) and was therefore reoperated after 6 months (Table 1).
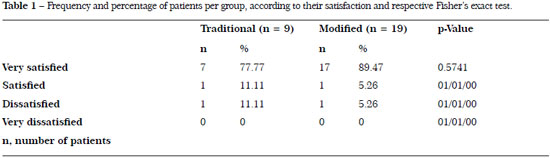

Figure 5. Patient from group 2 (modified treatment) with a high degree of satisfaction.

Figure 6. Patient from group 2 (modified treatment) with a high degree of satisfaction.
No complications such as hematomas, ear deformities, hypertrophic or keloid scar, suture dehiscence, or skin necrosis were observed in both groups (Table 2).
No statistically significant difference was observed for any of the variables compared between the groups.
DISCUSSION
Otoplasty is one of the plastic surgeries most commonly performed in children10. The modern techniques of this surgery can be divided into three categories according to the cartilage procedure: scraping11, 12, incision5, 13, and shaping with posterior sutures8,9.
Scraping techniques can lead to irregularities subsequent hematoma, infection, and even to cartilage destruction. In addition, these procedures result in a variable and asymmetric convex curvature on the side of the ear where scraping was applied14. Because of this risk, we avoided previous scraping of the antihelix, according to the technique proposed by Stenstroem11, even if this could facilitate the posterior rotation of the transition point between the concha and the antihelix, which was not evidenced, as we have performed rotation in even more hardened cartilages of adult patients. As there was no previous access, formation of any type of visible scar on the anterior face of the ear was avoided.
Techniques that completely disrupt the continuity of the cartilage, during the incision, promote the formation of a new antihelix through micro-incisions in the anterior face of the cartilage13, or a flap production in a cartilaginous island that remains adhered to the previous skin5. There is no randomized trial comparing incision techniques with scraping or posterior sutures; however, an incidence of complications similar to that of other techniques has been reported5.
Shaping procedures with posterior sutures seem safer because the integrity of the perichondrium is maintained and prior dissection of the skin is not required, thus resulting in the best aesthetic outcome with fewer complications15. Despite the high incidence of suture extrusion, reported in up to 19%16, the number of cases that needed to be re-approached was zero in group 2, probably owing to the minimum dissection of the skin for the production of the Mustardé sutures. The recurrence rate (one ear in group 1 [1.78%]) was lower than the rate reported in the literature (up to 6.6%17), probably because of the use of a thicker thread (3-0 colorless nylon).
Despite the existence of different repair procedures, there is no validated tool to measure the outcomes. Some studies used visual scales of comparison18; others used rates of recurrence and complications to compare the different methods in otoplasty4. McDowell proposed the use of objective measures with regard to the protrusion and symmetry between ears7. However, currently, the treatment is focused on the subjective evaluation of the patient and the surgeon, as well as of the improvement observed after the surgical treatment, as objective measures do not reflect the patient's view about the outcome19.
Driessen et al.20, looking for a definition for the diagnosis, reached the conclusion that otoplasty should focus on the upper protrusion of the auricle, as it plays a predominant role in the perception of the prominence7. This may explain the satisfaction of our patients, although none were subjected to procedures that involve the lobe, except its medialization, owing to the posterior rotation of the middle portion of the antihelix. However, we believe that excessive treatment of the upper portion of the antihelix should be avoided (Figure 7) to avoid sutures in the upper third for its definition. This allows a more natural aspect, with the progressive removal of the antihelix in the cranial direction10 (Figure 8).

Figure 7. Patient from group 1 (traditional treatment) with hypercorrection of the antihelix in the upper third.

Figure 8. Aesthetically pleasing ear showing the progressive loss of definition of the antihelix in the cranial direction.
As we avoided conchal resection, we had no case of "telephone ear deformity" with a relative prominence of the upper and lower third, or skin redundancy on the anterior face of the ear concha. On the other hand, our approach on the middle third of the antihelix prevented the occurrence of "reverse telephone ear deformity" due to conchal prominence.
Unlike the conventional Mustardé technique, our incision was posterior to the new antihelix, without resection of postauricular skin. This prevented an exaggerated approximation of the ear in relation to the skull, the attenuation of the postauricular groove, and the formation of keloid or hypertrophic scars due to suture tension. Moreover, no skin redundancy was observed on the posterior face of the ear (Figure 9).

Figure 9. Postoperative image at 6 months after the modified technique, showing a hidden scar in the posthelical groove, without skin redundancy.
We did not use Furnas sutures to anchor the concha to the mastoid, as we believe them to be unnecessary for this treatment. We also avoided narrowing the external auditory canal due to the sliding of the concha in the previous direction in relation to the mastoid3.
Of the four basic changes related to fan-like ears (lack of definition of the antihelix fold, conchal hypertrophy, increase of the concho-mastoid angle, and anterior projection of the lobe), several authors have pointed out the underdevelopment of the antihelix and the hyperdevelopment of the concha as the most common4, 6. We believe that these two changes are related to each other, as the absence of folds in the cartilage that would form the antihelix causes a laterolateral increase of conchal dimensions and provides a feeling of hypertrophy (Figure 10), as confirmed in our series. On the basis of these premises, we changed the approach of the conventional Mustardé technique and applied sutures to define the antihelix, anchoring it closer to the base of the concha, in order to rotate the new antihelix more and reduce the hypertrophy related to the concha.

Figure 10. Apparent conchal hypertrophy that was manually corrected by folding the antihelix in the posterior direction.
The strategy to shape the antihelix was developed from the technique described by Mustardé8, as we believe that this technique is easier to implement and has a low morbidity. However, when performing the suture, there are still risks of height and width asymmetry, subsequent formation of the antihelixes between the ears, possible rupture of the suture, and subsequent recurrence. A technical limitation that prevents a more natural result is also present. This is due to the impossibility to redo the folds inherent to normal antihelixes (Figure 8), as, conceptually, the "U" sutures only obtuse folds in the cartilage. Therefore, we believe that further studies on the aesthetic conformation of the antihelix are necessary to establish the optimal parameters for this shaping. We also hope that in vivo strategies and the clinical application of less invasive modeling measures, such as laser, radiofrequency, enzymatic digestion, and electromechanical manipulation, would allow making this already safe procedure even safer, and provide long-lasting results.
CONCLUSION
By establishing the lack of definition of the antihelix as the basic aspect related to prominent ears, we were able to restrict the surgical options to a single approach that is easy to learn and implement. This technique provided a good outcome (i.e., natural appearance) and a high degree of patient satisfaction. However, further studies with random location and objective parameters of evaluation are necessary to confirm our results.
REFERENCES
1. Ungarelli LF. Eficácia do retalho adipofascial retroauricular em otoplastia. Rev Bras Cir Plást. 2012;27:249-59.
2. Adamson JE, Horton CE, Crawford HH. The growth pattern of the external ear. Plast Reconstr Surg. 1965;36(4):466-70.
3. Speranzini MF, R. Otoplastia. In: Mélega JM, Mendes FH. Ed. Cirurgia Plástica - Os Princípios e a Atualidade. Rio de Janeiro: Guanabara Koogan; 2011. p. 1072-83.
4. Limandjaja GC, Breugem CC, Mink van der Molen AB, Kon M. Complications of otoplasty: a literature review. JPRAS. 2009;62(1):19-27.
5. Maricevich P, Gontijo AN, Duprat R, Freitas F, Pitanguy I. Island technique for prominent ears: an update of the Ivo Pitanguy clinic experience. Aesthet Surg J. 2011;31(6):623-33.
6. Adamson PA, Litner JA. Otoplasty technique. Facial Plast Surg Clin North Am. 2006;14(2):79-87.
7. McDowell AJ. Goals in otoplasty for protruding ears. Plast Reconstr Surg. 1968;41(1):17-27.
8. Mustarde JC. The treatment of prominent ears by buried mattress sutures: a ten-year survey. Plast Reconstr Surg. 1967;39(4):382-6.
9. Furnas DW. Correction of prominent ears by conchamastoid sutures. Plast Reconstr Surg. 1968;42(3):189-93.
10. Klockars T, Makitie A, Rautio J. Aesthetics of the auricle and its implications for otoplasty and auricular reconstruction. Int J Pediatr Otorhinolaryngol. 2012;76(9):1347-50.
11. Stenstroem SJ. A "natural" technique for correction of congenitally prominent ears. Plast Reconstr Surg. 1963;32:509-18.
12. Chongchet V. A method of antihelix reconstruction. Br J Plast Surg. 1963;16:268-72.
13. Ribeiro JA, da Silva GS. Finesse in otoplasty in four steps. Aesthet Plast Surg. 2012;36(4):846-52.
14. Jeffery SL. Complications following correction of prominent ears: an audit review of 122 cases. Br J Plast Surg. 1999;52(7):588-90.
15. Mandal A, Bahia H, Ahmad T, Stewart KJ. Comparison of cartilage scoring and cartilage sparing otoplasty - a study of 203 cases. JPRAS. 2006;59(11):1170-6.
16. Spira M. Otoplasty: what I do now - a 30-year perspective. Plast Reconstr Surg. 1999;104(3):834-40.
17. Aki F, Sakae E, Cruz DP, Kamakura L, Ferreira MC. Complications of otoplasty: review of 508 cases. Rev Soc Bras Cir Plast. 2006;21(3):140-4.
18. Schaverien MV, Al-Busaidi S, Stewart KJ. Long-term results of posterior suturing with postauricular fascial flap otoplasty. JPRAS. 2010;63(9):1447-51.
19. Mashhadi S, Butler DP. A strategy for assessing otoplasty outcome intra-operatively. JPRAS. 2012;65(7):984-5.
20. Driessen JP, Borgstein JA, Vuyk HD. Defining the protruding ear. J Craniofacial Surg. 2011;22(6):2102-8.
1. Professor of Plastic Surgery at the Federal University of Goiás (UFG); PhD in Surgery from FMRP-USP; Titular Member of BSPS - Professor of Plastic Surgery (UFG) and Plastic Surgeon at the Master Hospital - Goiania/GO
2. Postdoctoral Student at FMRP-USP; Postdoctoral Training and PhD in Surgery from FMRP-USP; Titular Member of BSPS - Assistant Physician of the Plastic Surgery course of FMRP-USP
Institution: Master Hospitals of Plastic Surgery - Goiás/Rondônia.
Corresponding author:
Rodrigo Gouvea Rosique
Rua 1123, 232 - Marista
Goiânia, GO, Brazil Zip code: 74175-070
Email: rodrigo@rosique.com.br
Article submitted: November 18, 2013.
Article accepted: December 13, 2014.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter