

Original Article - Year 2015 - Volume 30 -
Giant lipomas: a 14-case series
Lipomas gigantes: série de 14 casos
ABSTRACT
INTRODUCTION: Lipomas are the most common benign mesenchymal tumors worldwide. To be considered giant, they must be at least 10 cm in one of its dimensions or weigh at least 1,000 g. The objective of this study is to analyze a series of cases of giant lipomas seen in our practice.
METHOD: We conducted a retrospective analysis of the medical and anatomopathological records of patients diagnosed with lipomas who underwent surgery between January 2003 and January 2010.
RESULTS: We evaluated 14 patients with a mean age of 52.3 years (range, 33-72 years) and a mean evolution time until treatment of 4.4 years (range, 6 months to 20 years); 64% of cases presented no symptoms. All patients underwent surgical tumor resection. The average weight of the pieces was 3.8 kg (range, 512 g to 22 kg), while the average length of the longest axis was 27.5 cm (range, 15-66 cm). Postoperative complications were observed in 42% of cases.
CONCLUSION: We observed prolonged periods of evolution until treatment, even in cases of large-volume lesions. Open surgical excision should be considered the treatment of choice for these tumors.
Keywords: Lipoma surgery; Neoplasms; Adipose tissue surgery.
RESUMO
INTRODUÇÃO: Os lipomas são os tumores mesenquimais benignos mais frequentes na população. Para ser considerado gigante, deve apresentar pelo menos 10 cm em uma de suas dimensões ou pesar ao menos 1.000g. O objetivo do trabalho é analisar uma série de casos de lipomas gigantes atendidos em nosso serviço.
MÉTODO: Análise retrospectiva de prontuários e registros anatomopatológicos dos diagnósticos de lipomas submetidos a tratamento cirúrgico no período de janeiro 2003 a janeiro 2010.
RESULTADOS: Foram avaliados 14 pacientes, com média de idade de 52,3 anos (33-72) e tempo médio de evolução até o tratamento de 4,4 anos (seis meses - 20 anos); 64% dos casos não apresentavam sintomas. Todos os pacientes foram submetidos à ressecção cirúrgica da neoplasia. O peso médio das peças foi de 3,8 kg (512 g - 22 kg) e o tamanho médio no maior eixo foi de 27,5 cm (15-66 cm). Foram observadas complicações pós-operatórias em 42% dos casos.
CONCLUSÃO: Observamos períodos prolongados de evolução até o tratamento, mesmo em casos com lesões de grande volume. A exérese cirúrgica aberta deve ser considerada o tratamento de eleição para estes tumores.
Palavras-chave: Lipoma/cirurgia; Neoplasias; Tecido adiposo/cirurgia.
Lipomas are the most common benign mesenchymal tumors worldwide and have an estimated incidence of 10% and prevalence of 2.1 per 1,0001,2. They are commonly present in subdermal and subcutaneous locations and can occur in any region of the body, including the viscera and cavities3-5.
Most lipomas have small dimensions (rarely >10 cm) and weigh a few grams6. According to Sanchez et al.4, for a lipoma to be considered a giant one, it must be at least 10 cm long in one of its dimensions or weigh at least 1,000 g. Although the vast majority do not cause symptoms, depending on their location and proximity to other structures, lipomas can cause functional limitations due to size and excessive weight, lymphedema, pain, or nerve compression7.
OBJECTIVE
This work aimed to analyze a series of cases of giant lipomas that were surgically treated at our institution.
METHOD
A retrospective analysis of medical records and anatomopathology tests of all cases of lipomas that were surgically treated between January 2003 and January 2010 was conducted. Lipomas with at least one dimension > 10 cm were included. Among these, we studied those weighing >500 g with a subdermal or subcutaneous location.
Cases of syndromes associated with lipomatosis were excluded, as were lipomas of intracavitary or visceral location and infiltrative variants (intra- and intermuscular).
RESULTS
A total of 2,101 cases of lipomas confirmed by anatomopathology were treated surgically. Of these, 147 had at least one dimension > 10 cm. Twenty-one cases of lipomas > 500 g were identified, seven of which were excluded due to incomplete data in the medical record. Thus, a total of 14 cases were analyzed.
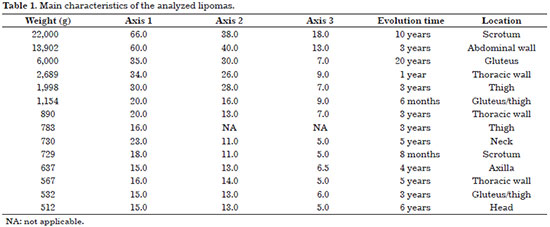
The average patient age was 52.3 years (range, 33-72 years). There was a predominance of male patients (64%; n = 9). The average time from the injury onset to treatment was 4.4 years (range, 6 months to 20 years) (Table 1).
The majority of patients had no symptoms (64%). Of the five symptomatic patients, two had pain, two had skin ulcerations, and one had lower limb lymphedema (secondary to the location of the lipoma in the scrotum). All of these patients showed symptom improvement after surgical treatment.
The preoperative diagnosis was predominantly clinical, and imaging studies were indicated in seven cases: ultrasonography in four, computed tomography (CT) in one, and magnetic resonance imaging (MRI) in two. The body weights of four patients (>120 kg) was a limiting factor for the performance of CT and MRI. All test results were suggestive of lipoma.
Incisional biopsies were performed in four cases. In one case, a biopsy showed features suggestive of liposarcoma, which was discarded after a detailed study of the surgical specimen was performed.
All patients underwent open surgical resection. No aspiration technique was employed in any case. The average weight of the resected tumors was 3.8 kg (range, 512 g to 22 kg). The average length of the longest axis was 27.5 cm (range, 15-66 cm) (Table 1).
In 10 cases, resection of excess skin was required prior to proper closing of the bloody area. In all cases, aspiration drainage was used in a closed system for an average of 2 days.
Anatomopathological examination showed common lipomas in 13 cases and fibrolipoma in one case.
During the postoperative period, six patients (42%) had complications. Paresthesia was observed in two patients but improved after a few weeks. Two patients required skin grafts, one due to a residual bloody area after skin flap ischemia and one due to infection and wound necrosis. There was one reported case of lower limb varicose veins after thigh lipoma resection. Pulmonary complications not directly related to the surgical area occurred in a patient with severe chronic obstructive pulmonary disease.
The patients were followed up and reviewed at regular intervals with a minimum of 24 months of follow-up after tumor resection without evidence of late complications or signs of recurrence.
DISCUSSION
Giant lipomas are rare. They usually evolve over long periods of time, tending to be insidious and progressive, with intervals of up to 10-15 years4,7-9. The largest skin lipoma, reported by Brandler in 1894, weighed 22.7 kg and was located in the scapular region of a 26-year-old man4,8. In this series, we report the case of a 22-kg lipoma in the scrotum of a 58-year-old man with a 10-year evolution period (Figure 1A and B, Figure 2A and B, Figure 3).

Figure 1. Front (A) and side (B) views of a 58-year-old man with a 22-kg giant scrotal lipoma that evolved over 10 years.

Figure 2. Intra- (A) and postoperative (B) views of removal of the giant scrotal lipoma, scrotal and penile reconstruction (arrow), and dissected and isolated pedicle.
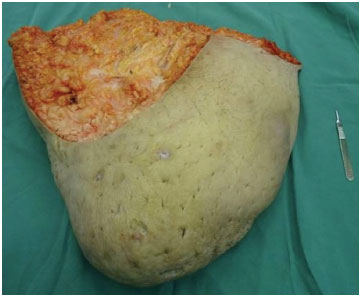
Figure 3. Photograph of a piece of the resected 22-kg giant scrotal lipomahypoattenuating
In this series, we chose to include only cases of lipomas >500 g with the aim of analyzing the most significant samples in relation to the associated symptoms as well as difficulties in preoperative diagnosis and complications. Lipomas are twice as common in women, probably due to their greater accumulation of adipose tissue10,11. In our series, however, there was a male predominance (64% of cases). Lipomas are typically unique tumors, multi-lobulated and pseudoencapsulated, that are composed of mature adipocytes. They usually present as mobile and asymptomatic lesions with a fibro-elastic consistency. Apart from the typical subcutaneous location, they may also be present in the subfascial plane and as rare infiltrative variants (intra- and intermuscular). The viscera and cavities can also be affected5,7,8,12-15.
The fat contained within lipomas usually increases as body weight increases but does not decrease even in times of starvation or cachexia7,8,14. The commonly reported evolution time is not reliable since most of the giant lipomas are asymptomatic in the initial period4,10. When present, the symptoms result from compression of the neighboring structures, size, and/or excessive weight7, as seen in three of the cases in this series. Skin ulcers, the most common secondary changes in giant4 lipomas, occurred in two cases in this series.
On imaging, lipomas have characteristic features. On ultrasonography, they present as hyperechoic lesions (relative to the musculature) with echogenic lines corresponding to the septa. On CT, they are hypoattenuating lesions (-50 to -150 HU) and are not impregnated by contrast (Figure 4). On MRI, the signal is similar to that of conventional fat with hyperintensity on T1-weighted and hypointensity on T2-weighted imaging, and their margins adjacent to normal tissues are clearly defined. They appear as homogeneous lesions with thin and uniform septa and have a >75% fat composition5,7,12,14,15.
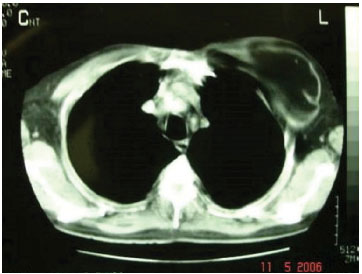
Figure 4. Computed tomography image of a giant lipoma within the thoracic wall (sub-pectoral).
According to Terzioglu et al.7 and Phalen et al.10, there is no way to definitely differentiate lipomas from liposarcomas using imaging studies only. However, other authors believe that this differentiation can be accomplished in most cases16-18. The greatest difficulty in differentiation occurs in cases of well-differentiated liposarcoma.
On radiography, calcified areas that are highlighted secondary to fat necrosis are present in 10-15% of malignant lesions but rarely in benign lesions; however, this is a nonspecific finding17,18. On MRI, liposarcomas have irregular septa and thick non- adipose-associated tissue with a small proportion of fat within the tumor (<75%) compared to nodular and associated globular17,18 lesions. According to Kransdorf et al.17, lesions with one dimension >10 cm are 14 times more likely to be malignant.
Suspicious lesions may require an incisional biopsy or fine-needle aspiration, but the latter is often inconclusive for these cases7,12,13,15 (Figures 5A and B). Malignancy is very rare in cutaneous lipomas, and its possibility is even questioned by some authors. This hypothesis should be considered in lesions showing rapid growth, high volume, and the presence of symptoms or ulceration4,5,7,16-18. In our series, the incisional biopsy results of one of the patients were suggestive of liposarcoma, but malignancy was excluded after excision of the lesion.

Figure 5. Lateral (A) and posterior (B) photographs of a 54-year-old man with a 730-g giant cervical lipoma that evolved over 5 years. *Incisional biopsy scar.
There are reports of using the aspiration technique (using conventional liposuction cannulas) for these tumors4,8,9,11, but the risk of recurrence or incomplete removal of the lesion as well as a high incidence of seroma and hematoma are possible. With this type of treatment, a precise histological diagnosis is impossible. Thus, surgical excision is the modality of choice for treatment, generally with dissection facilitated by the presence of a pseudocapsule4,5,7-9 involving the lesion (Figures 6A and B, Figure7).

Figure 6. Pre- (A) and postoperative (B) photographs of a 48-year-old man with a 512-g giant lipoma of the scalp (subgaleal) that evolved over 6 years.
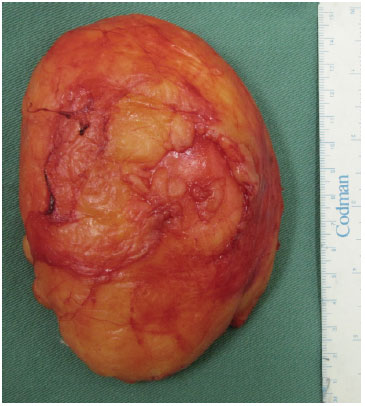
Figure 7. Surgical piece from the resected 512-g giant lipoma of the scalp (subgaleal).
None of the patients presented with tumor recurrence, but this may have been influenced by the limited postoperative follow-up in some cases.
CONCLUSION
In the present study, we observed similar characteristics to data found in the literature regarding the evolution time, presence of symptoms, and incidence of complications. Similar difficulties regarding the differential diagnosis of liposarcoma were also observed. This is the largest case series of giant lipomas in the literature and includes the second largest case ever reported.
REFERENCES
1. Mescon H. Lipoma in clinical dermatology. Clin Dermatol. 1991;4:1-2.
2. Rydholm A, Berg NO. Size, site and clinical incidence of lipoma. Factors in the differential diagnosis of lipoma and sarcoma. Acta Orthop Scand. 1983;54(6):929-34. http://dx.doi.org/10.3109/17453678308992936. PMid:6670522.
3. Harrington AC, Adnot J, Chesser RS. Infiltrating lipomas of the upper extremities. J Dermatol Surg Oncol. 1990;16(9):834-7. http://dx.doi.org/10.1111/j.1524-4725.1990.tb01569.x. PMid:2398202.
4. Sanchez MR, Golomb FM, Moy JA, Potozkin JR. Giant lipoma: case report and review of the literature. J Am Acad Dermatol. 1993;28(2 Pt 1):266-8. http://dx.doi.org/10.1016/S0190-9622(08)81151-6. PMid:8432930.
5. Hakim E, Kolander Y, Meller Y, Moses M, Sagi A. Gigantic lipomas. Plast Reconstr Surg. 1994;94(2):369-71. http://dx.doi.org/10.1097/00006534-199408000-00025. PMid:8041830.
6. Shmookler BM, Enzinger FM. Pleomorphic lipoma: a benign tumor simulating liposarcoma. A clinicopathologic analysis of 48 cases. Cancer. 1981;47(1):126-33. http://dx.doi.org/10.1002/1097-0142(19810101)47:1<126::AID-CNCR2820470121>3.0.CO;2-K. PMid:7459800.
7. Terzioglu A, Tuncali D, Yuksel A, Bingul F, Aslan G. Giant lipomas: a series of 12 consecutive cases and a giant liposarcoma of the thigh. Dermatol Surg. 2004;30(3):463-7. PMid:15008886.
8. Silistreli OK, Durmuş EU, Ulusal BG, Oztan Y, Görgü M. What should be the treatment modality in giant cutaneous lipomas? Review of the literature and report of 4 cases. Br J Plast Surg. 2005;58(3):394-8. http://dx.doi.org/10.1016/j.bjps.2004.09.005. PMid:15780237.
9. Mello DF, Helene A JR. Lipoma subgaleal gigante: relato de caso. Rev Bras Cir Craniomaxilofac. 2010;13(3):180-2.
10. Phalen GS, Kendrick JI, Rodriguez JM. Lipomas of the upper extremity: a series of fifteen tumors in the hand and wrist and six tumors causing nerve compression. Am J Surg. 1971;121(3):298-306. http://dx.doi.org/10.1016/0002-9610(71)90208-X. PMid:4322966.
11. Dolsky RC, Asken Nguyan S. Surgical removal of lipomas by liposuction surgery. Am J Cosmet Surg. 1986;3:3.
12. Haas AF, Fromer ES, Bricca GM. Spindle cell lipoma of the scalp: a case report and review. Dermatol Surg. 1999;25(1):68-71. http://dx.doi.org/10.1046/j.1524-4725.1999.08038.x. PMid:9935099.
13. Mordjikian E, Leão E. Lipoma gigante de coxa: Relato de caso. Rev Soc Bras Cir Plast. 2001;16(3):23-8.
14. D'Alessandro GS, Nunes TR, Lajner A, Beirigo MF, Porto O, Pinto WS. Lipoma intermuscular gigante: Relato de caso. Rev Bras Cir Plast. 2008;23(3):226-8.
15. El-Monem MH, Gaafar AH, Magdy EA. Lipomas of the head and neck: presentation variability and diagnostic work-up. J Laryngol Otol. 2006;120(1):47-55. http://dx.doi.org/10.1017/S0022215105004597. PMid:16359147.
16. Jones AP, Lewis CJ, Dildey P, Hide G, Ragbir M. Lipoma or liposarcoma? A cautionary case report. J Plast Reconstr Aesthet Surg. 2012;65(1):e11-4. http://dx.doi.org/10.1016/j.bjps.2011.08.004. PMid:21865105.
17. Kransdorf MJ, Bancroft LW, Peterson JJ, Murphey MD, Foster WC, Temple HT. Imaging of fatty tumors: distinction of lipoma and well-differentiated liposarcoma. Radiology. 2002;224(1):99-104. http://dx.doi.org/10.1148/radiol.2241011113. PMid:12091667.
18. Peterson JJ, Kransdorf MJ, Bancroft LW, O'Connor MI. Malignant fatty tumors: classification, clinical course, imaging appearance and treatment. Skeletal Radiol. 2003;32(9):493-503. http://dx.doi.org/10.1007/s00256-003-0647-8. PMid:12802520.
Irmandade da Santa Casa de Misericórdia de São Paulo, São Paulo, SP, Brazil
Institution: Study carried out at Irmandade da Santa Casa de Misericórdia de São Paulo - ISCMSP, São Paulo, SP, Brazil.
Corresponding author:
Daniel Francisco Mello
Irmandade da Santa Casa de Misericórdia de São Paulo
Rua Mato Grosso, 128, Conj. 72 - Higienópolis
São Paulo, SP, Brazil Zip Code 01239-040
E-mail: mello.plastica@gmail.com
Article received: March 27, 2014.
Article accepted: December 13, 2014.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter