

Original Article - Year 2015 - Volume 30 -
Star nymphoplasty: a surgical technique for labia minora hypertrophy
Ninfoplastia em estrela: técnica para redução dos pequenos lábios vulvares
ABSTRACT
INTRODUCTION: In recent years, women have been frequently consulting the plastic surgeon concerning the shape and dimensions of the labia minora and other surrounding structures, not only for aesthetic but also functional reasons, e.g., dyspareunia. The authors present a technique for the aesthetic and functional treatment of the external female genitalia, the vulva, with the purpose of correcting hypertrophy of the labia minora (nymphs), without changing their form.
METHOD: This technique consists in the incision in the shape of a star leading to a shortening of nymphs both anteroposteriorly and craniocaudally. This is a 15-year retrospective study, with clinical and surgical follow-up of 64 female patients with an age range between 14 and 58 years, all submitted to star nymphoplasty, the technique proposed in this study.
RESULTS: The results were obtained from the patients operated from January 1996 to December 2011, at the Hospital da Lagoa and at Interclínica-Centroplástica, Jardim Botânico, Rio de Janeiro, RJ. A high rate of patient satisfaction with the size and aesthetic shape of the genitalia was achieved. There was a low rate of complications and remaining complaints.
CONCLUSION: This surgical procedure is done with the objective of reshaping the tissue structure of the hypertrophic labia minora. From a technical point of view, it can be considered as a simple and effective functional and aesthetic treatment of the female genitalia.
Keywords: Nymphoplasty; Labiaplasty; Star incision; Intimate surgery; Hypertrophy of the labia minora.
RESUMO
INTRODUÇÃO: O cirurgião plástico tem sido consultado com frequência, nos últimos anos, sobre a forma e as dimensões dos pequenos lábios vulvares e outras estruturas circunvizinhas, não só pela questão estética, mas também pela funcional, da dispareunia. Os autores apresentam uma técnica de tratamento estético e funcional da genitália externa feminina, a vulva, com o intuito de corrigir a hipertrofia dos pequenos lábios (ninfas), sem alterar-lhes a forma.
MÉTODO: A técnica consiste na abordagem do pequeno lábio vulvar, com uma incisão em forma de estrela, produzindo um encurtamento das ninfas tanto ântero-posteriormente como crânio-caudalmente. O estudo é de tipo retrospectivo de um período de 15 anos, com seguimento clínico e cirúrgico de 64 pacientes de sexo feminino, com uma faixa etária entre 14 e 58 anos, todas submetidas à ninfoplastia em estrela, técnica proposta neste estudo.
RESULTADOS: Os resultados foram obtidos da ficha dos pacientes operados no período compreendido entre janeiro de 1996 e dezembro de 2011, no Hospital da Lagoa e na Interclínica-Centroplástica, Jardim Botânico, Rio de Janeiro-RJ. Alto índice de satisfação das pacientes com o tamanho e o formato estético da genitália. Houve uma baixa taxa de complicações e queixas residuais.
CONCLUSÃO: Este ato cirúrgico é feito com o objetivo de remanejar a estrutura tecidual hipertrófica dos pequenos lábios vulvares. De um ponto de vista técnico, pode-se considerar como um procedimento simples e eficaz no tratamento tanto funcional como estético da genitália feminina.
Palavras-chave: Ninfoplastia; Labioplastia; Incisão em estrela; Cirurgia íntima; Hipertrofia de pequenos lábios.
Nymphoplasty or Labiaplasty is a simple and rapid procedure that consists in the surgical and aesthetic approaches for the female genitalia. This type of procedure is aimed at achieving a more suitable and aesthetic form of the labia minora.
The enhancement and modeling of the asymmetry of the labia minora, as well as the redundant tissue of the vulva, are the main objectives of the proposed technique1,2.
Currently, cosmetic vaginal surgery has gained wide acceptance and development; it has become a popular and openly disclosed procedure because of the benefits and excellent results obtained with a well-refined technique.
Widely reported in the media as "genital rejuvenation," the procedure encompasses various aspects, from the functional and structural alteration to the enhancement of the aesthetic appearance of the female genitalia. This approach involves a series of procedures of a surgical nature3. Some of the most common procedures associated with nymphoplasty are reduction of the clitoral hood, vulvoplasty, vaginoplasty, perineoplasty, and hymenoplasty.
From a technical standpoint, intimate surgery attempts to improve the external appearance of the genitalia. In addition, the change in the external configuration of the area4 also brings satisfaction to women, positively improving their self-esteem related to intimate aspects such as the exploration of sexuality resulting from sexual freedom, as well as the appreciation of the forms and aesthetic concepts of beauty5.
OBJECTIVES
In the present study, we aimed to present our experience of cases treated with the proposed surgical technique.
The main objective of this study is to present our experience in the surgical treatment of labia minora hypertrophy.
METHODS
This is an observational, retrospective study in a consecutive series of 64 patients treated at the Hospital da Lagoa and Interclínica-Centroplástica in Rio de Janeiro, who underwent surgery consisting in the star-shaped excision of the hypertrophic labia minora, from 1996 to 2011, with a clinical follow-up of 2-5 years. The data were obtained through analysis and review of medical records of patients submitted to the proposed surgical procedure. In the review of medical records, data were analyzed in relation to certain factors such as the primary complaint, age, postoperative complaints, and complications associated with the procedure. Among the main complaints of the patients were the unaesthetic appearance of the genitalia, difficulty in using intimate apparel and tight-fitting clothing, interference in sexual intercourse (dyspareunia), and infectious processes as a result of impaired intimate hygiene (Figure 1). Notably, the complaints were similar to those found in the literature6,7.
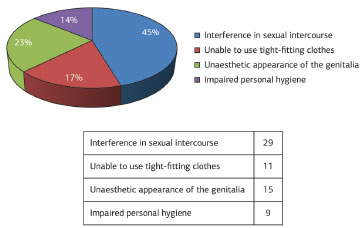
Figure 1. Complaints/reasons for surgery.
Anatomy
The nymphs are bilateral vulval folds, projected in the craniocaudal direction, approximately 30-35 mm in length and 10-15 mm in thickness, have a double tegumentary layer of nonkeratinized squamous epithelium separated by connective tissue, and sensitive to stimuli8.
The blood supply of this structure derives from internal pudendal arteries and veins. The innervation of the nymphs is mainly of the somatosensory type (S2-S4), from branches of the internal pudendal nerve.
A considerable asymmetry is often found in a population of otherwise healthy women. Nevertheless, a woman may or may not be aware of having this condition (Figures 2 and 3).

Figure 2. Identification of redundant tissue. Preoperative aspect of the labia minora.
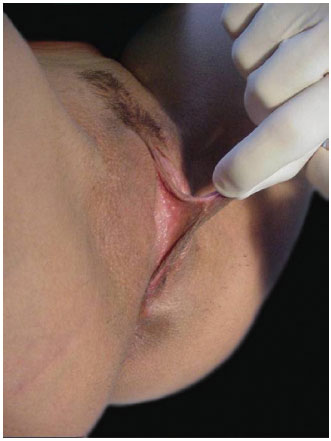
Figure 3. Identification of redundant tissue. Preoperative aspect of the labia minora.
Surgical technique
The patients were operated in a surgical center, in the lithotomy position, under sedation with local anesthesia.
A group of six patients underwent epidural anesthesia, according to the need for surgical procedures, such as abdominal dermolipectomy and liposuction.
The procedure begins with the application of an ointment containing 2% lidocaine in the vulvar mucosa. The area of the star-shaped resection is drawn on the hypertrophic labia minora (portion projected to the outside, beyond the limit of the labia majora), generally equivalent to the central area of the structure9-13. The infundibular areas and the area near the clitoral hood should not be touched (Figures 4A and B).
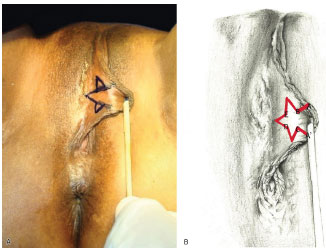
Figure 4. (A) Star-shaped marking of the external face of the labia minora. (B) Star-shaped marking of the area to be resected.
An anesthetic solution with 2% xylocaine and 1:100,000 IU epinephrine is infiltrated in the marked lines. The incision is made to the total thickness of the nymph, sectioning the three layers. This resection should be uniform and parallel to the imaginary border of the vaginal opening and, at the same time, on a parallel line exceeding by 1 cm the limit of the labia majora1,2, aided by the placement of two Gillies hooks. The incision of the mucosa is followed by strict homeostasis.
The suture is performed with the aid of straight tweezers at the extreme points of the labial structure (A and A'). Subsequently, a suture is made at points uniting B, C, D, and E (Figure 5). This suture should be made in single plane with absorbable Catgut 4.0, with continuous sutures both in the external and internal mucosal layers (Figures 6 and 7). The dressing comprises Nebacetin® topical ointment, padded gauze, and absorbent compress.
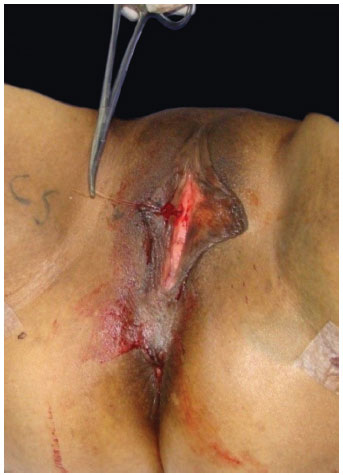
Figure 5. Surgery. The suture was performed with the aid of straight tweezers, at points uniting A and A'.

Figure 6. Immediate postoperative period.
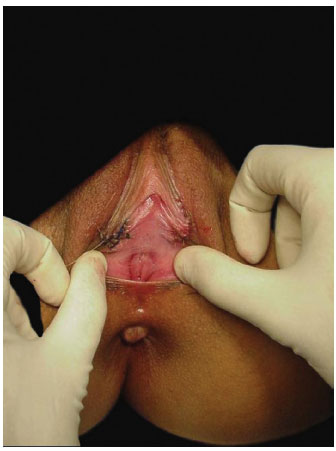
Figure 7. Immediate postoperative period.
RESULTS
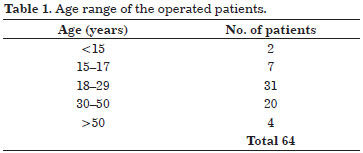
We evaluated 64 female patients with complaints of hypertrophy of the vulval labia minora. The most frequent complaint was interference with sexual intercourse, reported in 45% of the cases studied. The age of the study population ranged from 14 to 58 years, and the star-shaped surgical resection was most frequently performed in those at their third decade of life -this is the age group with the highest demand for our proposed procedure (Table 1).
The postoperative complaints were mainly pain and local edema, which regressed spontaneously in at most 5 days. Concerning postoperative complications, we experienced two cases of intramural hematoma on the fifth postoperative day. The first case involved a patient who had intense physical activity and lack of rest, and the hematoma was resolved clinically with local heat and antibiotic therapy. On the other hand, the second case of hematoma needed surgical reintervention. In the cases operated, no complications such as suture dehiscence, infection, or changes in sensitivity were reported. There was no incident involving the scar or complications due to scar retraction.
A clinical follow-up of 2-5 years postoperatively was carried out, with improvement of prior complaints and few residual complaints, in some cases related to sexual performance and dyspareunia (Figures 8 and 9).
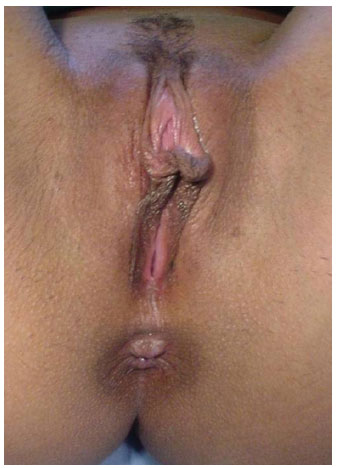
Figure 8. Pre-surgery. Hypertrophy of the labia minora.

Figure 9. Late postoperative period.
In the postoperative period, as a protocol and institutional conduct, antibiotic prophylaxis was indicated for 72 h, use of anti-inflammatory for 5 days, analgesia if necessary, and, as standard recommendation, daily hygiene and sexual abstinence for 30 days.
DISCUSSION
With the entry of women into the labor market, becoming an economically active partner of the population and with the fall of rules and sexual taboos, women have been increasingly concerned about their health and beauty. The size of the female sexual organ has been a major concern not only for aesthetic reasons but also because of the functional problem of dyspareunia. Notably, in recent years, women of all ages have consulted the plastic surgeon about this problem.
Nevertheless, what is considered, by some, as a defect of the vulva may simply be a normal or acceptable situation for others. However, from a subjective perspective, the size of the labia minora cannot be measured; when an enlargement is considered a disease, it can always be surgically corrected for aesthetic, functional, or emotional reasons when expressed as a complaint14.
The causes of hypertrophy of the labia minora differ and are, to some extent, complex; they may be related to genetic factors or associated with the influence of hormones during pregnancy and puberty, as already reported in the literature. The indiscriminate use of anabolic steroids may lead to an increase in the size of the labia minora and clitoris. Lately, perceived conflicts of sexual identity have been reported, due to the descriptions of observers, sexual partners, or others4,5.
Despite the availability of several techniques already described in the literature, the optimal treatment is still undetermined. For the reconstruction of the labia minora, amputation with a linear incision and wedge resection, as described by Alter, are still by far the most frequently used labioplasty techniques15. However, both techniques have limited results; moreover, simple amputation is not always well accepted by patients, because of scarring and changes in sensitivity.
Concerning the technique and refinements, the benefits of using absorbable sutures are seldom discussed. In the present work, as already described, chromic catgut was used for the synthesis of vulvar tissue, because it is a cheap suture with rapid absorption, thereby relieving the discomfort of the patient with less time for suture absorption. Other authors have reported the use of monocryl because this suture is easy to handle, has good resistance, and has low inflammatory reaction and absorption time necessary for proper healing.
The surgical intervention associated with liposuction and application of autologous grafting fat could be used to achieve an aesthetic appearance of the external structure of the female genitalia.
Concerning the reason for the consultation, our survey identified the main complaint as being difficulty in sexual intercourse as a result of the enlargement of the labia minora. This alteration may cause emotional and psychological issues, in turn leading to conflicts in intimate relationships.
Research has demonstrated that, in many cases, aesthetic issues are the significant and fundamental reason motivating the patient to visit a plastic surgeon for this type of complaint, differing somewhat from the finding in our experience16.
Surgery in a woman's intimate zone is designed to solve functional or aesthetic concerns that can prevent the normal development of women in society.
CONCLUSION
Star nymphoplasty is a technique that is easy to implement, is safe, and has a low rate of complications. It is has been shown to be a reproducible procedure leading to patients' satisfaction about the correction of hypertrophy of the labia minora, and producing a closer to normal genital appearance. It can therefore eliminate the social, functional, and aesthetic discomfort associated with the deformity.
REFERENCES
1. Tepper OM, Wulkan M, Matarasso A. Labioplasty: anatomy, etiology, and a new surgical approach. Aesthet Surg J. 2011;31(5):511-8. http://dx.doi.org/10.1177/1090820X11411578. PMid:21719863.
2. Triana L, Robledo AM. Refreshing labioplasty techniques for plastic surgeons. Aesthetic Plast Surg. 2012;36(5):1078-86. http://dx.doi.org/10.1007/s00266-012-9916-z. PMid:22718365.
3. Ellsworth WA, Rizvi M, Lypka M, Gaon M, Smith B, Cohen B, et al. Techniques for labia minora reduction: an algorithmic approach. Aesthetic Plast Surg. 2010;34(1):105-10. http://dx.doi.org/10.1007/s00266-009-9454-5. PMid:20043154.
4. Munhoz AM, Filassi JR, Ricci MD, Aldrighi C, Correia LD, Aldrighi JM, et al. Aesthetic labia minora reduction with inferior wedge resection and superior pedicle flap reconstruction. Plast Reconstr Surg. 2006;118(5):1237-47. http://dx.doi.org/10.1097/01.prs.0000237003.24294.04. PMid:17016196.
5. Choi HY, Kim KT. A new method for aesthetic reduction of labia minora (the deepithelialized reduction of labioplasty). Plast Reconstr Surg. 2000;105(1):419-22, discussion 423-4. http://dx.doi.org/10.1097/00006534-200001000-00067. PMid:10627011.
6. Alter GJ, Alter GJ. A new technique for aesthetic labia minora reduction. Ann Plast Surg. 1998;40(3):287-90. http://dx.doi.org/10.1097/00000637-199803000-00016. PMid:9523614.
7. Rouzier R, Louis-Sylvestre C, Paniel BJ, Haddad B. Hypertrophy of labia minora: experience with 163 reductions. Am J Obstet Gynecol. 2000;182(1 Pt 1):35-40. http://dx.doi.org/10.1016/S0002-9378(00)70488-1. PMid:10649154.
8. Franco T. Princípios de cirurgia plástica. São Paulo: Atheneu; 2002. p. 869-874.
9. Daher M. Ninfoplastia. In: XXXIX Congresso de Cirurgia Plástica Curso Internacional Avançado; 2002 Nov 23; Salvador, Bahia.
10. Daher M. Ninfoplastia com incisão em estrela. In: 44º Congresso Brasileiro de Cirurgia Plastica; 2007 Nov; Curitiba, Brazil.
11. Daher M. Ninfoplastia com incisão em estrela: uma nova abordagem. In: 2º Congresso do DESC; 2008 Fev; São Paulo, Brazil.
12. Muñiz AR. Ninfoplasty: a new approach? Aesthet Surg J. 2014;34(2):332. http://dx.doi.org/10.1177/1090820X13519102. PMid:24497621.
13. Matarasso A, Tepper OM, Wulkan M. Response to "ninfoplasty: a new approach?". Aesthet Surg J. 2014;34(2):333. http://dx.doi.org/10.1177/1090820X13519104. PMid:24497622.
14. Kruk-Jeromin J, Zieliński T. [Hypertrophy of labia minora: pathomorphology and surgical treatment]. Ginekol Pol. 2010;81(4):298-302. PMid:20476604.
15. Alter GJ. Aesthetic labia minora and clitoral hood reduction using extended central wedge resection. Plast Reconstr Surg. 2008;122(6):1780-9. http://dx.doi.org/10.1097/PRS.0b013e31818a9b25. PMid:19050531.
16. Goodman MP. Female genital cosmetic and plastic surgery: a review. J Sex Med. 2011;8(6):1813-25. http://dx.doi.org/10.1111/j.1743-6109.2011.02254.x. PMid:21492397.
1. Interclínica - Centroplástica, Rio de Janeiro, RJ, Brazil
2. Serviço de Cirurgia Plástica e Reparadora do Hospital São Lucas, Pontifícia Universidade Católica do Rio Grande do Sul, Porto Alegre, RS, Brazil
3. Serviço de Cirurgia Plástica do Professor Ivo Pitanguy, Rio de Janeiro, RJ, Brazil
4. Clínica Consultório Dra. Karina Vanzan, Rio de Janeiro, RJ, Brazil
5. Clínica Dr. Guilherme Monteiro Cirurgião Plástico, São Luís, MA, Brazil
6. Clínica Dr. Jair Maciel, Rio de Janeiro, RJ, Brazil
7. Clínica Dr. Isaac Moura Cirurgia Plástica, Belém, PA, Brazil
Institution: Study performed at the Interclínica - Centroplástica Rio de Janeiro, Rio de Janeiro, RJ, Brazil.
Corresponding author:
Marcelo Daher
Interclínica - Centroplástica
Rua Jardim Botânico, 164 - Jardim Botânico
Rio de Janeiro, RJ, Brazil Zip Code 22461-000
E-mail: marcelodaher@centroplastica.com.br
Article received: May 29, 2014.
Article accepted: February 8, 2015.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter