

Original Article - Year 2015 - Volume 30 -
Liposuction-related complications and death: survey conducted by the BSPS commission on liposuction
Intercorrências e óbitos em lipoaspiração: pesquisa realizada pela comissão de lipoaspiração da SBCP
ABSTRACT
INTRODUCTION: Liposuction is a surgical procedure that was developed approximately 30 years ago by Fournier, Illouz, and others. In 2011, a total of 211,108 liposuction procedures were performed in Brazil versus 325,332 in the United States. Over the years, liposuction performed with the tumescent technique has had a good safety profile. It is also performed by other specialists, including dermatologists, and has been described as an outpatient procedure in public institutions in Brazil. The scarcity of data on the subject has led the Brazilian Society of Plastic Surgery (BSPS) to create a commission composed of 10 full members with the aim of investigating the factors involved in severe liposuction-related complications and death in Brazil.
METHODS: An online questionnaire was created using an anonymous link on the BSPS website. The questionnaire was sent to the registered email addresses of 4,441 associate and full members of the BSPS. The first question was about the occurrence of liposuction-related complications. The respondents could only continue to answer the questionnaire if the answer to this question was "yes." In addition to the questionnaire, the BSPS sent letters to the official state and federal institutions in which the case or complication/death-related records and/or deaths as a consequence of liposuction were expected to exist. The significance of the association between death and the various factors was determined using the chi-square test. The significant variables were included in Poisson Regression Models. The significance level was set at 5%. The data were analyzed using STATA software version 10.0.
RESULTS: Thromboembolic events, combined surgical procedures, and the facilities where the procedure was performed were risk factors involved in liposuction-related mortality.
CONCLUSION: The implementation of programs that aim to standardize liposuction procedures may effectively reduce liposuction-related mortality rates. This study aimed to make a positive educational impact on the development of future safe liposuction protocols.
Keywords: Liposuction; Lipoplasty; Mortality rate; Complications; Survey.
RESUMO
INTRODUÇÃO: A lipoaspiração, procedimento cirúrgico com cerca de 30 anos desde sua sistematização por Fournier, Illouz e outros, atingiu, em 2011, o total de 211.108 cirurgias realizadas no Brasil e 325.332, nos Estados Unidos. Ao longo dos anos, foi reputado como procedimento seguro, baseado em conceitos da técnica tumescente. Realizado também por outras especialidades, já foi descrito como método ambulatorial, inclusive em instituições públicas no Brasil, por dermatologistas. Motivada por essa lacuna de dados, a Sociedade Brasileira de Cirurgia Plástica criou uma comissão composta por dez membros titulares, com o objetivo de realizar uma pesquisa para reconhecer a presença de possíveis fatores envolvidos nas intercorrências graves e nos óbitos, após uma cirurgia de lipoaspiração no Brasil.
MÉTODOS: Foi elaborado um questionário on-line através de um link anônimo e disponível para consulta, no site da SBCP. O questionário foi enviado, através dos e-mails de cadastro, para 4.441 membros associados e titulares da SBCP. A primeira questão indagava sobre a ocorrência de intercorrências em lipoaspiração. Somente a resposta positiva era então direcionada ao restante do questionário. Além do questionário, foram enviadas cartas pela SBCP às instituições oficiais estaduais e federais, nas quais prováveis registros de processos ou cadastro de fatos relacionados a intercorrências e/ou óbitos após lipoaspiração poderiam existir. A significância da associação entre óbito e os diversos fatores foi medida com aplicação do teste qui-quadrado. As variáveis significantes foram incluídas em Modelos de Regressão de Poisson. Foi considerado o nível de significância de 5%. Os dados foram analisados com auxílio do programa STATA versão 10.0.
RESULTADOS: Fenômenos tromboembólicos, associação de cirurgias e o local de realização da cirurgia demostraram ser fatores de risco envolvidos na mortalidade de lipoaspiração.
CONCLUSÃO: Programas visando à normatização na realização das lipoaspirações podem ser eficazes na diminuição da mortalidade em lipoaspiração. Acreditamos que este artigo pode promover um impacto positivo educacional e, futuramente, gerar protocolos de segurança em lipoaspiração.
Palavras-chave: Lipoaspiração; Lipoplastia; Taxa de mortalidade; Complicações; Pesquisa.
Liposuction is a surgical procedure that was developed approximately 30 years ago by Fournier, Illouz, and others1. In 2011, a total of 211,108 procedures were performed in Brazil2, while 325,332 were performed in the United States3.
Liposuction performed using the tumescent technique has had a good safety profile4. It is also performed by other specialtists5, including dermatologists, and has been described as an outpatient procedure in public institutions in Brazil6.
Reports of adverse outcomes by the media have raised concerns about whether they are more important than what the studies conducted by plastic surgeons suggest7. In the late 1990s in the USA, the liposuction-related mortality rate was higher than that associated with car accidents8. Literature reviews of severe complications and deaths demonstrated that liposuction is not an innocuous procedure and that its surgical risks require further study9. Pulmonologists have warned about the danger of fat embolism syndrome, a condition that is difficult to diagnose and for which the treatment differs from that of pulmonary embolism10 in Brazil11,12 and worldwide13. Cases of injury to the abdominal viscera14,15 and ureter16, blindness, necrosis, and severe infection17 are some of the severe complications described in the literature.
The scarcity of data on the subject has led the Brazilian Society of Plastic Surgery (BSPS) to create a commission of 10 full members with the aim of researching the factors involved in severe complications and deaths related to liposuction procedures performed in Brazil.
METHODS
The Liposuction Commission was created in March 2012 with the aim of investigating the factors involved in severe complications and fatal outcomes related to liposuction procedures performed in Brazil.
An online questionnaire was developed using an anonymous link on the BSPS website. The questionnaire was sent to the registered e-mail addresses of 4,441 associate and full members of the BSPS. A letter to explain the objectives of the research and to ensure anonymity of the answers preceded the questions.
Three weeks later, the same link was resent to ask more colleagues to participate in the study.
The first question was about the occurrence of complications in liposuction. The respondents could only continue to answer the questionnaire if the answer to this question was "yes."
In addition to the questionnaire, the BSPS sent letters to the official state and federal institutions where case records or records of liposection-related complications and/or deaths were expected to exist. These letters were sent to all of the State Councils of Medicine, the Federal Council of Medicine, all of the Medical Examiners, and all the Institutes of Forensic Medicine in Brazil. The letters stated the purpose of the study and requested, on a confidential basis, information about the number of deaths that occurred over the last 5 years and their causes.
The significance of the association between death and the various factors was determined using the chi-square test. The significant variables were included in Poisson Regression Models. The significance level was set at 5%. The data were analyzed using the STATA software version 10.0.
RESULTS
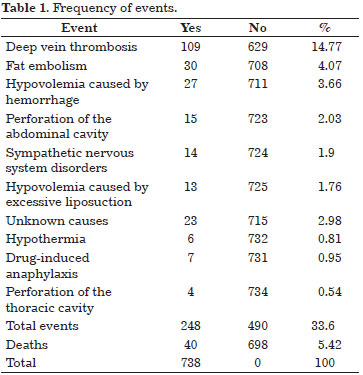
Of the 4,441 plastic surgeons who were approached by the BSPS, 738 (16.61%) returned the questionnaire. Of the 738 participants, 490 (66.39%) did not report complications, whereas 248 (33.60%) did. Of the 738 cases, 40 (5.4%) resulted in death intra- or postoperatively (Table 1).
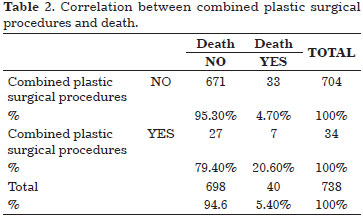
The number of deaths in combined surgical procedures was four times higher than that in separate procedures. The association between combined plastic surgery procedures and death was highly significant (p<0.0001) (Table 2).
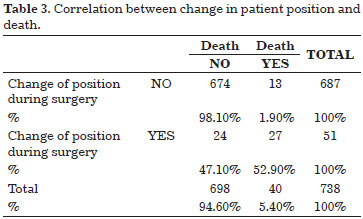
Changing the patient's position during the procedure (ventral to dorsal or dorsal to ventral and/or lateral) was not reported in most cases, and the mortality rate in this group was 1.9%. However, of the 51 cases in which the patient was repositioned during the procedure, more than half (52.9%) had complications with a fatal outcome. This difference was highly significant (p<0.001) (Table 3).
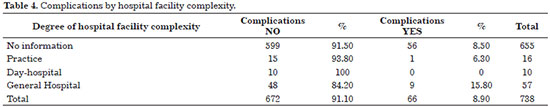
Although comparison of the facilities (general hospitals, day-hospitals, and practices) demonstrated that complications occurred more often in practices and day-hospitals, the large number of answers left blank for this question requires cautious interpretation (Table 4).
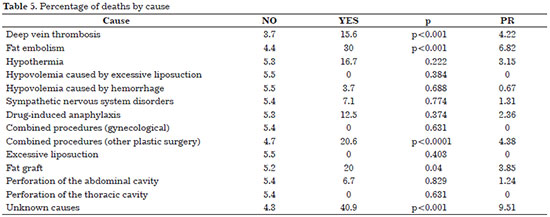
The main reported complications were deep vein thrombosis and fat embolism. The prevalence ratio (PR) determined the proportion of deaths in the presence of one factor relative to the proportion of deaths in the absence of this same factor. The PR showed a higher percentage of deaths related to unknown causes, fat embolism, combined surgical procedures, and deep vein thrombosis (Table 5).
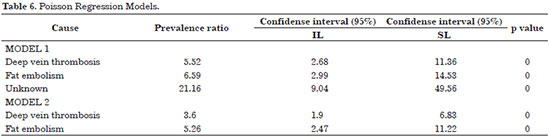
Table 6 shows the results of the two regression models whose factors are significantly associated with death. In model 1, the proportion of deaths was 452% higher among individuals who had deep vein thrombosis, 559% higher among those who had fat embolism, and more than 20 times higher among cases related to unknown causes. This variable was removed from model 2 because the classification ("I do not know the cause") may hide a variety of factors that may confound the effect of the association between the other factors and death. In this model, the proportion of deaths was 260% higher among individuals who had deep vein thrombosis and 426% higher among those with fat embolism.
DISCUSSION
The number of severe complications associated with liposuction, including death, is alarming and calls for the urgent quantification and examination of their causes. In this sense, several studies have indicated some factors that may be increase the risk of liposection-related death from liposuction18.
Grazer & Jong7 in 2000 and Hughes19 in 2001 published data obtained through questionnaires. Lehnhardt et al.14 compiled autopsy data from studies that used questionnaires, while Rao et al.8 obtained autopsy data from studies that did not use questionnaires. The participation of plastic surgeons (BSPS members) in the present survey was lower (16.6%) than those in the other surveys (Grazer, 76.4%; Hughes, 53%; and Lehnhardt, 65%), although the answers were sent by regular mail or fax in some of those surveys.
The difficulty obtaining medical records and data on fatal outcomes in plastic surgery procedures was notorious, an issue that is also discussed in Lehnhardt's article. There were very few answers to the letters sent to the institutional bodies, and some were duplicated; in addition, they did not indicate the training of the queried physician. Therefore, these answers were not included in the study.
The analysis comparing the data relative to the factors that were common to the four studies7,8,14,19 showed that thromboembolic events and fat embolism in combined surgical procedures were significant.
Hughes19 investigated thromboembolism and fat embolism in cases of nonfatal complications from liposuction. Thromboembolic events and fat embolism were preponderant in all of the analyses performed in this study (14.8% and 4.1%, respectively), which is in line with the results obtained by Rao8 (one of five deaths), Grazer7 (23.1% and 8.5%), and Lehnhardt14 (11.1%).
In Lehnhardt's study, which had 2,275 respondents, there were 72 major complications, including 23 deaths, with a predominance of cases of severe infection (37.5%), abdominal cavity perforation (9.72%), and hemorrhage from excessive liposuction (9.72%). The percentage of complications in combined procedures was 13.8%, while the percentage of outpatients was 55%.
Grazer reported 95 deaths among 496,245 cases, i.e., 19.1 in 100,000, and percentages of perforation, infection, and hemorrhage of 14.6%, 5.4%, and 4.6%, respectively. In Grazer's study, 77.7% of the deaths occurred in an outpatient environment. Hughes reported 1 death in 47,415 cases and that concomitant abdominoplasty or other procedures increased the mortality rate.
The present research revealed rates of 33.6% for complications and 5.4% for death. Therefore, considering the total number of liposuction procedures performed in Brazil during 2011 (211,108) and the total number of deaths in the survey, there were 18.9 deaths for every 100,000 performed liposuction procedures.
Morbidity rates were higher when the procedures were performed outside the hospital environment; however, this observation should be interpreted with caution because of the high number of answers left blank.
The present study does not provide statistically relevant data relative to the anesthetic technique in liposuction procedures or the role it may have in the occurrence of complications. Fatal outcomes were more frequent in liposuction procedures combined with other plastic surgery procedures, a result that is similar to those obtained in most studies.
Although changing the patient's position had a highly significant impact in the present survey, this result cannot be compared with data from the other studies.
The fact that unknown causes are referred to in all the studies shows that some factors may not have been adequately diagnosed.
Adequate documentation of procedures and the participation of plastic surgeons in scientific research should be encouraged to increase the knowledge about liposection-related complications and deaths. The statistical data obtained in this type of study serve as educational tools that can be used by plastic surgeons to minimize the incidence of liposection-related major complications and deaths. The BSPS should promote programs that encourage the participation of its members in research. Despite the limitations of the presented data, this study furthers our knowledge of liposuction-related mortality.
The high incidence of deep vein thrombosis observed in this survey indicates that prophylactic measures to avoid the condition (pneumatic compression of the lower limbs, low molecular weight heparin, and early walking) should be considered during the planning of liposuction procedures. Adequate patient and facility selection according to the available hospital resources should be considered the major safety parameters in the planning of liposuction procedures.
CONCLUSIONS
Thromboembolic events, combined procedures, and the facilities where the procedure is performed were shown to be risk factors involved in liposuction-related mortality. Programs aiming to standardize liposuction procedures may effectively reduce liposuction-related mortality. This study aimed to make a positive educational impact on the development of future safe liposuction protocols.
ACKNOWLEDGMENTS
Francisco José Fontenele Bezerra, M.D;
Marcus Vinicius Alfano Moscozo, M.D;
Péricles Serafim Filho, M.D;
Luiz Humberto Garcia De Souza, M.D;
Arnaldo Miró, M.D;
José Hermano Marinho Junior, M.D;
Ronildo Stork, M.D;
Sergio Augusto Da Conceição, M.D;
Fabio Coutinho Ferreira, M.D.
REFERENCES
1. Ahern RW. The history of liposuction. Semin Cutan Med Surg. 2009;28(4):208-11. http://dx.doi.org/10.1016/j.sder.2009.10.001.
2. Sociedade Brasileira de Cirurgia Plástica - SBCP. Cirurgias realizadas em 2011. São Paulo; 2012 [cited 2013 May 25]. Available from: http://www2.cirurgiaplastica.org.br/wp-content/uploads/2012/11/sbcp_isaps.pdf.
3. American Society for Aesthetic Plastic Surgery - ASAPS. 15th Annual Cosmetic Surgery National Data Bank Statistics. 2012. Plastic Surgery Statistic Report [cited 2013 Oct 3]. Available from: http://www.surgery.org/sites/default/files/ASAPS-2011-Stats.pdf.
4. Klein JA. Tumescent technique for local anesthesia improves safety in large-volume liposuction. Plast Reconstr Surg. 1993;92(6):1085-98. http://dx.doi.org/10.1097/00006534-199311000-00014. PMid:8234507.
5. Coleman WP 3RD, Glogau RG, Klein JA, Moy RL, Narins RS, Chuang TY, et al. Guidelines of care for liposuction. J Am Acad Dermatol. 2001;45(3):438-47. http://dx.doi.org/10.1067/mjd.2001.117045. PMid:11511843.
6. Utiyama Y, Di Chiacchio N, Yokomizo V, Benemond TM, Metelmann U. Retrospective study of 288 liposuctions carried out at the dermatology service of the " Hospital do Servidor Público Municipal de São Paulo. An Bras Dermatol. 2003;78(4):435-42. http://dx.doi.org/10.1590/S0365-05962003000400005.
7. Grazer FM, Jong RH. Fatal outcomes from liposuction: census survey of cosmetic surgeons. Plast Reconstr Surg. 2000;105(1):436-46. http://dx.doi.org/10.1097/00006534-200001000-00070. PMid:10627013.
8. Rao RB, Ely SF, Hoffman RS. Deaths related to liposuction. N Engl J Med. 1999;340(19):1471-5. http://dx.doi.org/10.1056/NEJM199905133401904. PMid:10320385.
9. Franco FF, Basso RCF, Tincani JA, Kharmandayan P. Complicações em lipoaspiração clássica para fins estéticos. Rev Bras Cir Plást. 2012;27(1):135-40. http://dx.doi.org/10.1590/S1983-51752012000100023.
10. Costa NA, Mendes DM, Toufen C, Arrunátegui G, Caruso P, Carvalho CRR. Síndrome da angústia respiratória do adulto por embolia gordurosa no período pós- operatório de lipoaspiração e lipoenxertia. J Bras Pneumol. 2008;34(8):622-5. http://dx.doi.org/10.1590/S1806-37132008000800013. PMid:18797748.
11. Folador JC, Bier GE, Camargo RF, Sperandio M. Síndrome de embolia gordurosa: relato de caso associado a lipoaspiração. J Pneumol. 1999;25(2):114-7.
12. Ross RM, Johnson GW. Fat embolism after liposuction. Chest. 1988;93(6):1294-5. http://dx.doi.org/10.1378/chest.93.6.1294. PMid:3371109.
13. Uemura K, Kikuchi Y, Shintani-Ishida K, Nakajima M, Yoshida K. A fatal case of post-operative pulmonary thromboembolism with cosmetic liposuction. J Clin Forensic Med. 2006;13(1):41-3. http://dx.doi.org/10.1016/j.jcfm.2005.05.011. PMid:16311062.
14. Lehnhardt M, Homann HH, Daigeler A, Hauser J, Palka P, Steinau HU. Major and lethal complications of liposuction: a review of 72 cases in Germany between 1998 and 2002. Plast Reconstr Surg. 2008;121(6):396e-403e. http://dx.doi.org/10.1097/PRS.0b013e318170817a. PMid:18520866.
15. Di Candia M, Malata CM. Aesthetic and functional abdominal wall reconstruction after multiple bowel perforations secondary to liposuction. Aesthetic Plast Surg. 2011;35(2):274-7. http://dx.doi.org/10.1007/s00266-010-9591-x. PMid:21046103.
16. Kattapuram TM, Avery LL. Ureteral tear at the ureteropelvic junction: a complication of liposuction. Emerg Radiol. 2010;17(1):79-82. http://dx.doi.org/10.1007/s10140-009-0797-7. PMid:19259711.
17. Sherman JE, Fanzio PM, White H, Leifer D. Blindness and necrotizing fasciitis after liposuction and fat transfer. Plast Reconstr Surg. 2010;126(4):1358-63. http://dx.doi.org/10.1097/PRS.0b013e3181ea4576. PMid:20885259.
18. Teimourian B, Adham MN. A national survey of complications associated with suction lipectomy: what we did then and what we do now. Plast Reconstr Surg. 2000;105(5):1881-4. http://dx.doi.org/10.1097/00006534-200004050-00043. PMid:10809120.
19. Hughes CE 3RD. Reduction of lipoplasty risks and mortality: an ASAPS survey. Aesthet Surg J. 2001;21(2):120-7. http://dx.doi.org/10.1067/maj.2001.115166. PMid:19331882.
1. Hospital Universitário Pedro Ernesto, Universidade do Estado do Rio de Janeiro (UERJ), Rio de Janeiro, RJ, Brazil
2. Hospital Pedro Ernesto, Rio de Janeiro, RJ, Brazil
3. Universidade Federal de Juiz de Fora (UFJF), Juiz de Fora, MG, Brazil
Institution: Study conducted by the Comissão de Lipoaspiração 2012/2013 of the Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil.
Corresponding author:
Antonia Marcia Branco Cupello
Universidade do Estado do Rio de Janeiro
Avenida das Américas, 4200 - Bloco 9 - Sala 224 - Barra da Tijuca
Rio de Janeiro, RJ, Brazil Zip Code 22640-102
E-mail: contato@antoniacupello.com.br
Article received: July 1, 2014.
Article accepted: August 31, 2014.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter