

Original Article - Year 2015 - Volume 30 -
Reduction mammoplasties and mastopexies performed at HC-UNICAMP: comparative analysis between two techniques
Mamoplastias redutoras e mastopexias realizadas no HC-UNICAMP: análise comparativa entre duas técnicas
ABSTRACT
INTRODUCTION: Several reduction mammoplasty and mastopexy techniques are described in the literature, with the aim of reconstituting the upper pole, offering better projection, and providing adequate treatment for breast ptosis. However, particular attention should be devoted to the safety of the technique, with maintenance of vascularization, tissue innervation, and the capability of breastfeeding. Female patients operated on with the inferior pedicle flap technique were compared with those operated on with purse-string circular suturing.
METHODS: Eighty-five patients who had undergone reduction mammoplasty or mastopexy without implants, between January 2011 and December 2012 at Unicamp's Clinical Hospital, were evaluated. Thirty-one patients who only underwent reduction mammoplasty by Pitanguy's technique (without the use of flaps or circular sutures) were excluded. Of the remaining 54 patients, five were subsequently excluded for not attending medical appointments or failure to have postoperative ultrasonography. A group of 16 patients who had undergone circular suturing and a group of 33 operated on by the inferior pedicle technique were considered.
RESULTS: Demographic data were similar for both groups. A higher number of minor complications and unsatisfactory results were observed in the group that underwent the inferior pedicle technique, who also had a higher rate of relevant post-operative ultrasonography events.
CONCLUSION: The circular suturing technique resulted in a high satisfaction rate, lower number of complications, and longer lasting results than the inferior pedicle technique, during the period analyzed in this study.
Keywords: Reduction mammoplasty; Mastopexy; Breast reduction, Inferior pedicle flap; Continuous circular suture; Cosmetic surgery.
RESUMO
INTRODUÇÃO: Diferentes técnicas para mamoplastia redutora e mastopexia são descritas na literatura, visando a resultados que reconstituam o polo superior, ofereçam melhor projeção e proporcionem tratamento adequado para a ptose mamária. No entanto, devemos nos atentar para a segurança da técnica, com manutenção da vascularização, inervação dos tecidos e possibilidade de amamentação. Análise comparativa com pacientes operadas pela técnica com retalho de pedículo inferior e pacientes operadas pela técnica com sutura circular em bolsa.
MÉTODOS: Análise de 85 pacientes submetidas à mamoplastia redutora ou mastopexia sem implantes, entre janeiro de 2011 e dezembro de 2012, no Hospital de Clínicas da Unicamp. Foram excluídos 31 pacientes, as quais foram submetidas apenas à mamoplastia redutora pela técnica de Pitanguy (sem utilização de retalhos ou sutura circular). Dentre as 54 pacientes restantes, cinco foram posteriormente excluídas devido ao não comparecimento à consulta ou à não realização da ultrassonografia pós-operatória. Foram agrupadas 16 pacientes submetidas à sutura circular contínua e 33 pacientes operadas pela técnica de pedículo inferior.
RESULTADOS: Dados demográficos foram semelhantes nos dois grupos. Maior número de pequenas complicações e resultados insatisfatórios foi observado no grupo submetido à técnica de pedículo inferior, bem como maior índice de achados ultrassonográficos relevantes no pós-operatório.
CONCLUSÃO: A técnica de sutura circular contínua apresentou elevado índice de satisfação, menor número de complicações e resultados mais duradouros quando comparados com a técnica de pedículo inferior, durante o período analisado.
Palavras-chave: Mamoplastia redutora; Mastopexia, Redução de mamas; Retalho de pedículo inferior; Sutura circular contínua; Cirurgia estética.
Surgeons have been trying to optimize the results of reduction mammoplasty and mastopexy since the beginning of the twentieth century, which has led to the constant revision of surgical techniques and the development of new strategies aimed at the cosmetic improvement of postoperative results.
Extensive and varied literature is available on reduction mammoplasty with or without mammopexy. In 1961, Pitanguy improved Arié's technique1, creating a new technique2-5 that introduced the principle of previous individualized marking without predetermined molds; this enabled large tissue resections at a single session (keel-shaped, in the center of the breast), compared to that with Arié, who performed the surgery in two chronologically separated steps.
Since the work by Peixoto in 1979, surgeons became concerned about perfecting details, aiming at reduction in final scarring. Peixoto showed that it was possible to perform small skin resections, even with large-volume gland resections, and believed that cicatricial skin retraction would contribute to the final shape of the breast cone6,7, resulting in only vertical scarring. With time, it became apparent in some cases that breast ptosis occurred due to insufficient skin resection. Thus, several other technical strategies were developed, based on Peixoto's concepts, and avoiding the unpleasant scarring enlargements produced by some previous marking techniques.
The reconstitution of the superior mammary pole has merited the attention of several authors6,8-11, who employed flaps for that purpose. In our field, Ribeiro8 proposes an inferior dermoglandular pedicle flap, with vascular nutrition provided by internal mammary perforator vessels, mainly in the sixth intercostal space, for the reconstitution of the superior mammary pole, which is often emptied by other techniques. Nevertheless, failure to correctly perform these flaps may lead to vascularization problems and the formation of steatonecrosis nodules, which are difficult to distinguish from the breast's inherent changes and diseases.
The use of purse-string circular suturing or continuous circular suturing of the breast was described in 2003; this involved the aponeurosis of the pectoralis major muscle, to reduce the mammary base and project the nipple-areola complex (NAC) at the vortex of the mammary cone, with restoration of the superior pole, and without the use of flaps12,13.
The surgical indication for correction of ptosis and/or mammary hypertrophy must take into account the possible cosmetic outcome, the ease of the procedure, and the safety of the technique, without compromising vascularization, tissue innervation, and the capability of future breastfeeding. Moreover, procedures with lasting medium- and long-term results, as well as progressively smaller scarring to the size of an acceptable cosmetic standard, are valued.
OBJECTIVE
The goal of this work is to carry out a comparative analysis between patients operated on with the inferior pedicle flap technique and those operated on with the purse-string circular suturing technique on the aponeurosis of the pectoralis major muscle. Possible complications and unsatisfactory results were considered, with regard to scarring position and size, maintenance of the projection, and short- and long-term satisfaction rates.
METHODS
The medical records of 85 patients who underwent reduction mammoplasty or mastopexy without implants between January 2011 and December 2012 at Unicamp's Clinical Hospital were analyzed. Of these, 31 patients were excluded from the study, as they had only undergone reduction mammoplasty by Pitanguy's technique (without the use of flaps or circular sutures). The remaining 54 patients were scheduled for outpatient return visits, breast ultrasonography, photographic recording, and a postoperative satisfaction survey. All 54 patients had completed a minimum of one year postoperatively. Of these patients, five were subsequently excluded for not attending consultations or failure to have postoperative ultrasonography. Thus, this study included 49 patients, 16 of whom underwent continuous circular suturing, with 33 operated on by the inferior pedicle technique. All patients were evaluated by a single observer (Figure 1).
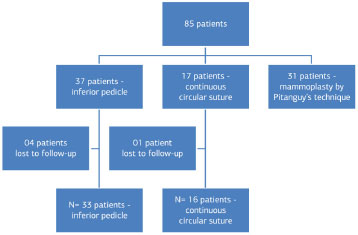
Figure 1. Diagram - Patient selection.
Preoperative marking and surgical technique
Inferior pedicle technique: With the patient in a sitting position, the areolae are marked with a 4 cm diameter areola cutter. A vertical line is then drawn from the sternal clavicle to the umbilical scar, and another from the midclavicular line to the superior areolar region. We mark point A, which corresponds to the projection of the inframammary fold on the breast's superior pole. A bi-digital maneuver is then used to mark points B and C, thereby enclosing the central region of the breast that will be de-epithelized. The previously marked points are connected to the inframammary fold with arched lines, which results in a marking similar to that previously published by Pitanguy2-5,14. The inferior pole of the breast is fully exposed, and the pedicle is marked at the mid-region of the inferior pole, with a width of 4 to 6 cm, and extending to 1 to 2 cm from the inferior edge of the areola. This previously enclosed area will also be de-epithelized and an incision will be made from the edge of the flap to the fascia of the major pectoralis muscle; this creates a glandular dermal fat flap, based on the perforating arteries and the branches of the internal mammary artery, and derived from the fourth, fifth, and sixth intercostal spaces. It is important for the flap to be at least 3 cm wide. After completion of the resection of excessive breast tissue, the pedicle is fixed close to the fascia with interrupted nylon 2-0 sutures. The breast is reassembled by joining points B and C at the midpoint of the flap base, with additional suturing in planes. This is also known as Ribeiro's technique.
Continuous circular suturing technique: Incisions are previously marked and are based on points A, B, C, and D, as established by Pitanguy; however, this sequential marking was advocated by Bueno et al.12, as described below.
The markings are made while the patient is sitting or standing, before the preanesthetic medication. There is an initial marking on the new inframammary fold, 2 to 3 cm cranial to the patient's natural fold, as well as a midvertical line from the sternal clavicle to the umbilicus. A third line is drawn from the midclavicular region to the nipple. Midpoint "B" is located on a line that originates in the fourth intercostal space towards the nipple. Its location can vary by 8 to 10 cm, depending on breast volume and the diameter of the thorax.
Point "C" is positioned laterally, and is defined by the clamping of the skin, lateral to the NAC, towards point "B". Point "D" is located on the extension of the midclavicular line, and 1.5 cm above the inframammary fold. Point "A", which is usually the first point marked in other techniques, appears in this technique as a consequence of the bi-digital clamping, rather than by the projection of the depth of the inframammary fold onto the midclavicular line. In this way, there is no fixed, predetermined distance from the sternal clavicle for positioning this point (Figures 2, 3, and 4).
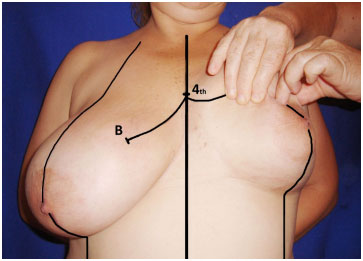
Figure 2. Marking - Continuous circular suture - Marking of points B and C.
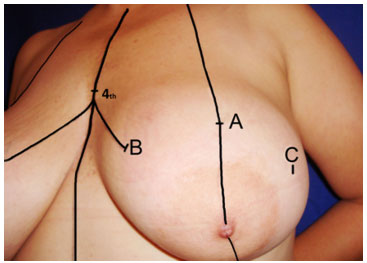
Figure 3. Marking - Continuous circular suture - Marking of point A on the midclavicular line, based on the bi-digital maneuver.
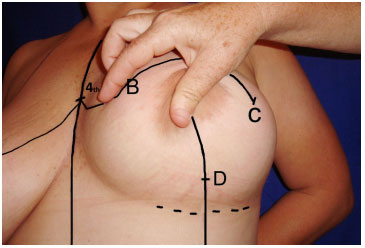
Figure 4. Marking - Continuous circular suture - Marking of point D on the midclavicular line, 2 cm above the original mammary fold.
Joining these four points forms a four-sided polygon or an ovoid surrounding the NAC. In the operating room, when the patient is in dorsal, horizontal decubitus, the markings are revised.
Surgery is performed with the patient's trunk elevated (30º to 40º) and without local infiltration. A tourniquet is applied to the base of the breast and the NAC is outlined with a 4 cm diameter areola cutter. This procedure is followed by de-epithelizing of the entire periareolar region and internal contouring, bordering the area outlined by points A, B, C, and D.
Incisions are performed within the de-epithelized region, and a superior pedicle flap, containing the NAC and about 3 cm thick, is outlined. While a tourniquet is kept on the breast, the wedge resection of the glandular and skin tissues of the inferior quadrants is performed. The tourniquet is then released and hemostasis of bleeding vessels is performed. Next, dissection is performed, on a supra-aponeurotic plane of the superomedial quadrant, towards the second intercostal space. Breast reassembly then follows, employing polyglactin 0 or monofilament nylon 2-0 suture; the continuous purse-string circular suture is initiated from the mid-region of the second intercostal space, close to the sternal manubrium, and proceeds with the circular suturing of the entire breast, back to the superomedial quadrant (Figure 5). Upon traction of the thread to complete the suture, the decrease of the breast's base and the resulting conical shape are noted. The finishing suture knot is performed; using the remaining suture thread, which has not been cut yet, another purse-string suture is made, passing again through the four quadrants, and completing the joining of the mammary tissue corresponding to the breast's lateral and mid pillars (Figure 6). Next, excess skin is excised, the glandular and skin pillars are closed along the vertical edges, and the NAC is repositioned, as in routine mammoplasties. Excess skin near the inframammary fold area is also excised with no special detail, in order to obtain an inverted T line of skin suture, and with the smaller branches at the level of the inframammary fold. No drains are employed (Figures 7 and 8). Porous adhesive tape covers all the suture lines, followed by a sterile dressing and postoperative surgical mesh.
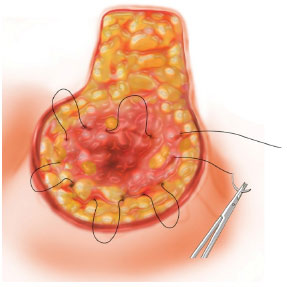
Figure 5. Scheme - Marking - Continuous circular suture (purse-string).
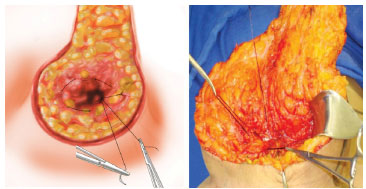
Figure 6. Intraoperative - Marking - Continuous circular suture (purse-string).

Figure 7. Continuous circular suture - Immediate postoperative.

Figure 8. Continuous circular suture - Immediate postoperative.
RESULTS
Forty-nine patients who underwent bilateral reduction mammoplasty or mastopexy at HC-Unicamp between January 2011 and December 2012 were included in the study. Sixteen of these patients underwent continuous circular suturing (group 1) and 33 were operated on with the inferior pedicle technique (group 2). All the patients were evaluated by a single observer.
The average age was 33.14 years (18-59) for group 1, and 31.96 (17-55) for group 2. Body mass index was similar for both groups, with an average of 25.71 kg/m2 (22.4-30.47) and 25.12 kg/m2 (19.37-29.41), respectively. Two patients from each group had previously undergone reduction gastroplasty. None of the study participants were smokers. Group 1 included one hypertensive patient, one with hypothyroidism, and one with asthma. In group 2, one patient was hypertensive, three had hypothyroidism, and one reported psoriasis. The follow-up period, from the date of surgery to when the questionnaire was filled in, ranged between 12 and 34 months.
For group 1, the average volume of tissue removed was 428.07 g for the right breast (range 13-910 g) and 370.71 g for the left breast (range 20-920 g). For group 2, a slightly lower amount of tissue was removed, with 272.58 g for the right breast (range 20-850 g) and 314.19 g for the left breast (range 25-620 g). General anesthesia was employed for all study patients and the first surgeon for all patients was a plastic surgery resident.
Three patients who underwent continuous circular suturing had Penrose drains, for two days each. Among five patients subjected to the inferior pedicle technique, three had Penrose drains (also for two days each), and two had Porto-Vac drains (one for two days and another for three days). There were no reported cases of hematoma requiring surgery in either group.
With regard to other complications and postoperative results, two cases of pseudoptosis were observed in group 2 patients, a feature that was not found in group 1. As a major complication, pulmonary thromboembolism was reported for one group 2 patient, who was admitted to a different unit, with good recovery. Additional complications were considered minor, although some required surgical repair procedures, as shown in the appended graph.
Some patients underwent additional surgery to improve the aesthetic outcome and/or possible resolution of minor complications, all of which included procedures performed under local anesthesia. Four group 1 patients underwent additional surgery. One of these received a total skin graft of the areola, one underwent axillary liposuction, and two were subjected to procedures to correct "ears" on the edge of breast base scarring. In group 2, 12 patients underwent additional surgery: one breast resuturing, four scar corrections (two of whom had undergone a previous triamcinolone infiltration for incisional keloids), three corrections of excess breast skin/tissue (ears) on the breast base, two axillary liposuctions, one symmastia correction, and one total skin graft of the areola.
None of the group 1 patients reported the presence of palpable nodules in either breast on the date when the questionnaire was filled in. Three group 2 patients reported palpable nodules, one of whom referred a "hardened" nodule with inverted "T" topography (point where the column and breast base sutures joined) on the left breast; another two reported painful palpable nodules on the superior pole of the left breast. Upon medical evaluation, five group 2 patients had palpable nodules. Two were mentioned above (nodule in the superior pole of the left breast, in agreement with the physical examination), one with palpable nodules in the superomedial quadrants of the breasts (bilaterally), one with palpable nodules in the superomedial quadrant of the right breast, and one with palpable nodules in the medial and lateral superior quadrants of the right breast (Figure 9).
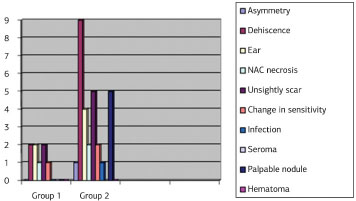
Figure 9. Graph - Postoperative complications.
Late (greater than one year) postoperative ultrasonography did not reveal significant alterations in any of the patients who underwent continuous circular suturing; only alterations due to surgical breast manipulation were found. Of the patients operated on with the inferior pedicle technique, four (hereafter named A, B, C, and D) had some significant ultrasonography finding:
Patient A underwent mammography, using the Breast Imaging-Reporting and Data System (BI-RADS) II classification; there was no mention of whether or not the lesion may have derived from suture material. For patients B and C, there was no report of localization (in quadrants) of surgical material and/or calcifications. For these patients, gynecological follow-up with routine mammography was recommended. For patient D, a mammogram and consultation with a breast specialist were advised (mammography with visualization of well-defined lesions in the right and left breasts, with BI-RADS II classification for the right, and BI-RADS III for the left).Patient A: Well-defined, 1.5-cm nodule in the superomedial quadrant of the left breast, which may have corresponded to a postoperative foreign body/granuloma reaction; clinical correlation and mammography were advised. Patient B: Presence of surgical material (suture?) on a supramuscular and glandular plane of the left breast, without lesions suggestive of malignancy. Patient C: Absence of pathologic microcalcifications, nodules, or asymmetry. Gross calcifications in the right breast. Diffuse distortion of the architecture bilaterally, secondary to a previous surgical procedure. Patient D: Approximate 1.4-cm granuloma in the superomedial quadrant of the right breast. Elliptical 1.8 cm density in the lateral quadrant of the left breast, which could correspond to a fibroadenoma.
DISCUSSION
Cosmetic surgery of the breasts imposes a great responsibility on plastic surgeons, given the social valuation of women's bodies in our society, breasts being closely linked to sexuality. Therefore, in a tropical country with an extensive shoreline, the quest for techniques and strategies that result in minimal scarring is great, and good results are even demanded by women with very large breasts. Most patients want their breasts to be firm, stable, conical-round shaped, with centered, anteriorly projected nipples, which is not always easy to achieve15.
The continuous circular suture technique allows a new approach to reduction mammoplasty and mastopexy procedures, when implants are not desired or necessary, as the suturing of the pectoral fascia and ensuing fibrosis reproduce, to a certain extent, the effects of the breast ligaments that were weakened by time, gravity, breast weight, and lactation. Besides, this technique tends to decrease the diameter of the base, re-positioning the glandular tissue and improving the projection of the breasts; in this way, less scarring is achieved, as excess marking and tissue removal occur after breast reassembly (Figures 10 to 15).

Figure 10. Preoperative Continuous circular suture - CSPO, 45 years-old.
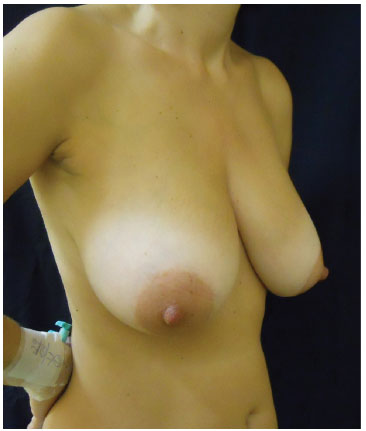
Figure 11. Preoperative Continuous circular suture - CSPO, 45 years old.
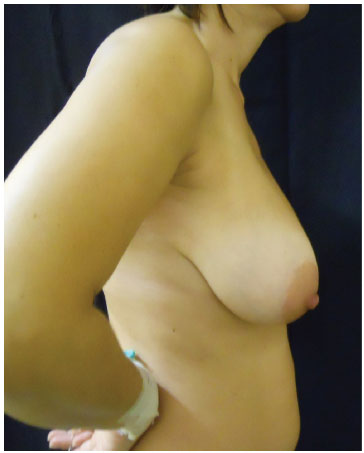
Figure 12. Preoperative Continuous circular suture - CSPO, 45 years-old.

Figure 13. Postoperative continuous circular suture (2 years) - CSPO, 47 years-old.

Figure 14. Postoperative continuous circular suture (2 years) - CSPO, 47 years-old.

Figure 15. Postoperative continuous circular suture (2 years) - CSPO, 47 years-old.
Conversely, to a varying extent, the inferior pedicle technique may lead to foci of steatonecrosis, in turn leading to calcifications, in addition to loss of projection, mainly in the superior poles, and ptosis of the breasts. This is likely due to the tilting movement of the breast over time, which empties the superior pole and often leaves the inferior pedicle flap apparent in its cranial portion, at approximately the level of the second intercostal space (Figures 16 to 22).
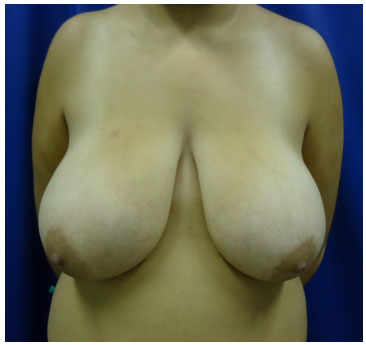
Figure 16. Preoperative inferior pedicle - AKR, 18 years-old.

Figure 17. Preoperative inferior pedicle - AKR, 18 years-old.

Figure 18. Preoperative inferior pedicle - AKR, 18 years-old.

Figure 19. Postoperative (1 year) reduction mammoplasty with inferior pedicle - AKR, 19 years-old.

Figure 20. Postoperative (1 year) reduction mammoplasty with inferior pedicle - AKR, 19 years-old.

Figure 21. Postoperative (1 year) reduction mammoplasty with inferior pedicle - AKR, 19 years-old.
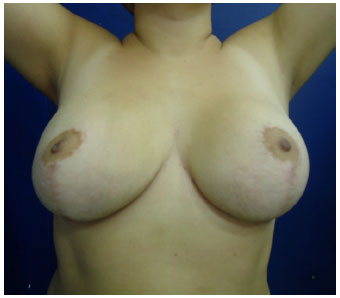
Figure 22. Postoperative (1 year) reduction mammoplasty with inferior pedicle - AKR, 19 years-old.
In this study, we observed no significant differences between the demographic data of the two groups: both the age average and ranges were similar; the weight average was slightly higher in the group that underwent continuous circular suturing, although the two groups presented very similar body mass indexes. As previously mentioned, a larger average amount of breast tissue was removed from group 1 patients, particularly for the right breast: 428.07 g vs. 272.58 g for group 2. Comorbidities were more prevalent in group 2, with 27.27% of the patients presenting some disease symptoms, compared with 18.75% in group 1.
Complication rates were similar to those reported in the literature3,8,11,16, with only 3% experiencing major complications (one case of pulmonary thromboembolism in group 2); if we take into account all the study patients (group1 + group2), the rate drops to approximately 2%. We noted a significant number of dehiscencewere reported, but no information on size was available for several of these; the questionnaires enabled us to clarify that most were small dehiscences, since only one of the group 2 patients underwent breast resuturing. An association was also found between the prevalence of unaesthetic scarring and patients with a record of suture dehiscences. A change in areolar sensitivity was reported by one group 1 patient (who underwent a total skin graft due to NAC necrosis), and by two group 2 patients, neither of whom had NAC necrosis; it is interesting to note that the patient who underwent a skin graft, in the latter group, reported no complications.
Contrary to literature reports, no seromas were reported by our patients; for group 1, this may be due to the decrease of dead space in the breast resulting from circular suturing. However, a possible bias in questionnaire answers cannot be excluded, as this was a retrospective study. Likewise, no bruising of the breasts was recorded and only a few instances of reabsorption ecchymosis were reported.
Only three of the five patients with palpable breast nodules had alterations in the ultrasonogram. The examination in the patient who reported a painful nodule in the superior pole of the left breast (confirmed upon medical examination) corresponds to Patient A. That of the patient with bilateral nodules in the superomedial quadrants corresponds to Patient C (the absence of findings on the left breast should be noted). Examination D corresponds to the patient who complained of a palpable nodule in the medial and lateral quadrants of the right breast; the left breast presented a lesion that was neither reported by the patient nor detected upon physical examination. No alterations were detected by ultrasonography, either in the patient who presented a hardened nodule with inverted "T" scarring (not considered a palpable nodule in the physical examination), or in the patient who reported a nodule in the superior pole of the left breast. Likewise, the ultrasonogram of the patient with nodules in the superomedial quadrant of the right breast presented alterations of breast architecture resulting from surgical intervention, which were not considered significant, as previously mentioned. Examination B refers to a patient who presented no complaints or alterations on physical examination. The low rate of ultrasonography findings raises questions about its accuracy as a means of evaluating postoperative breast alterations following reduction mammoplasty or mastopexy, in addition to being an operator-dependent exam. Magnetic resonance of the breasts is likely a more appropriate exam to detect possible steatonecrosis foci and granulomas in this type of patient; however, such an exam appears inappropriate as a screening method in our unit.
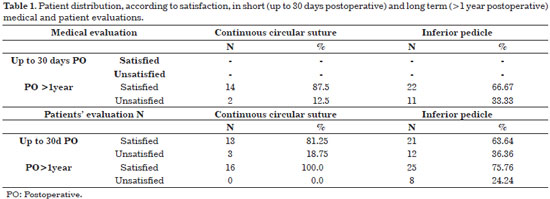
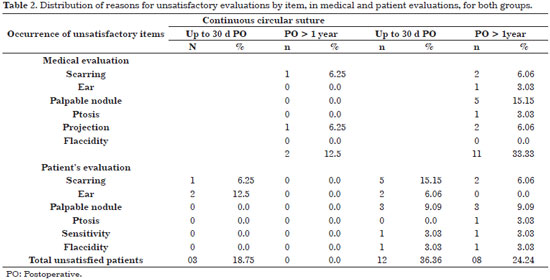
When analyzing patient satisfaction with either technique, the main consideration should be the rate of late postoperative satisfaction; many reasons for early postoperative lack of satisfaction were due to minor complications, which were resolved with simple approaches (correction of scarring, ears, etc.), as well as to poor recall in some patients. A 100% late postoperative satisfaction rate was found through binary answers (YES or NO) among patients subjected to continuous circular suturing. However, among patients subjected to the inferior pedicle technique, the rate was also acceptable, with approximately 75% reporting satisfaction (Table 1). Of the main complaints reported, scarring and the presence of palpable nodules were the most prevalent (Table 2).
When patients were analyzed long after undergoing continuous circular suturing, only one case of unaesthetic scarring (widened) was found, as well as one case of loss of breast projection, particularly in the superior pole, totaling 12.5% lack of satisfaction with the results. Of the patients operated on with the inferior pedicle technique, 11 reasons for partial lack of satisfaction were reported. However, these reasons were accounted for by only seven patients, with some reporting more than one reason. Thus, the rate of patients with an unsatisfactory outcome is 21.21%, not 33.3% , as shown in Table 2.
Upon comparing the physical examination and the pre- and postoperative photographs, we were unable to determine the reasons for the choice of one technique or the other; the study population was very heterogeneous, with various breast volumes, different degrees of ptosis, breast stability, and amount of striae, among other features, in addition to some cases of inadequate reporting. Therefore, it seems clear that firmer breasts, with good skin elasticity and less ptosis should present better results, regardless of the technique employed. No measurements of scar length, column height, and NAC positioning were performed, as no such preoperative measurements were taken in most cases, making comparison impossible. However, due to differential marking, patients operated on with the continuous circular suture technique were extremely satisfied with scar positioning and size, as well as with the shape and projection of the breasts.
CONCLUSION
This study shows that the continuous circular suturing technique resulted in good levels of satisfaction, with longer-lasting postoperative results throughout the period of the analysis, confirming the initial expectations (breasts with well-positioned scarring, decreased base, and good projection); however, satisfactory results were also obtained with the inferior pedicle technique. Thus, although we believe that neither of these techniques can be universally applied, the study is valuable for the knowledge gained regarding different strategies for optimizing results.
REFERENCES
1. Arié G. Nova técnica em mamaplastia. Rev Lat Amer Cir Plast. 1957;3(2):28-39.
2. Pitanguy I. Breast hypertrophy. In: Wallace AB, editor. Transactions of the second Congress of international Society of Plastic Surgeons; Edinburg. London: Livingstone; 1960.
3. Pitanguy I. [Mammaplasty. Study of 245 consecutive cases and presentation of a personal technic]. Rev Bras Cir. 1961;42:201-20. PMid:14486960.
4. Pitanguy I. Surgical treatment of breast hypertrophy. Br J Plast Surg. 1967;20(1):78-85. http://dx.doi.org/10.1016/S0007-1226(67)80009-2. PMid:5339723.
5. Pitanguy I. Mamaplastia. Rio de Janeiro: Guanabara Koogan; 1978.
6. Peixoto G. Reduction mammaplasty: a personal method. In: Ely JF, editor. Transactions of the Seventh International Congress of Plastic and Reconstructive Surgery; Rio de Janeiro. São Paulo: Cartgraf; 1979.
7. Peixoto G. The infra-areolar longitudinal incision in reduction mammoplasty. Aesthetic Plast Surg. 1985;9(1):1-5. http://dx.doi.org/10.1007/BF01570677. PMid:3993462.
8. Ribeiro L. Cirurgia plástica de mama. Rio de Janeiro: Medsi; 1989.
9. Graf R, Biggs TM, Steely RL. Breast shape: a technique for better upper pole fullness. Aesthetic Plast Surg. 2000;24(5):348-52. http://dx.doi.org/10.1007/s002660010057. PMid:11084696.
10. Hall-Findlay EJ. Pedicles in vertical breast reduction and mastopexy. Clin Plast Surg. 2002;29(3):379-91. http://dx.doi.org/10.1016/S0094-1298(02)00008-1. PMid:12365638.
11. Georgiade NG, Serafin D, Morris R, Georgiade G. Reduction mammoplasty utilizing an inferior pedicle nipple areolar flap. Ann Surg. 1979;3:211-8.
12. Bueno MAC, Cavazana WC, Baroudi R, Nunes PHF, Psillakis JM, Boin IFSF. Running circular suture technique for reduction mammaplasty and mastopexy. Aesthetic Plast Surg. 2012;36(6):1320-8. http://dx.doi.org/10.1007/s00266-012-9972-4. PMid:22955862.
13. Bueno MAC, Souto LRM. Mammaplasty: a new approach. Aesthetic Plast Surg. 2003;27(3):185-92. http://dx.doi.org/10.1007/s00266-003-0113-y. PMid:14534827.
14. McCulley SJ, Hudson DA. Short-scar breast reduction: why all the fuss? Plast Reconstr Surg. 2001;107(4):965-9. http://dx.doi.org/10.1097/00006534-200104010-00010. PMid:11252090.
15. Mey D, Greuse M, Azzam C. The evolution of mammaplasty. Eur J Plast Surg. 2005;28(3):213-7. http://dx.doi.org/10.1007/s00238-005-0744-0.
16. Graf R, Araujo L, Rippel R, Neto L, Pace D, Biggs T. Reduction mammaplasty and mastopexy using the vertical scar and thoracic wall flap technique. Aesthetic Plast Surg. 2003;27(1):6-12. http://dx.doi.org/10.1007/s00266-002-0111-5. PMid:12687296.
Universidade Estadual de Campinas - UNICAMP, Campinas, SP, Brazil
Institution: Study carried out at Hospital de Clínicas of the Universidade Estadual de Campinas, Campinas, SP, Brazil.
Corresponding author:
Ivana Leme de Calaes
Universidade Estadual de Campinas
Rua Egberto Ferreira de Arruda Camargo, 1200 - Parque da Hípica
Campinas, SP, Brazil Zip Code 13092-621
E-mail: ivanacalaes@yahoo.com.br
Article received: July 10, 2014.
Article accepted: January 25, 2015.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter