

Ideas and Innovation - Year 2015 - Volume 30 -
Duoscapular flap: a new option in shoulder reconstructive surgery
Retalho Duoescapular: uma nova opção na cirurgia reparadora do ombro
ABSTRACT
INTRODUCTION: Shoulder cutaneous fibrosarcoma is an unusual pathology that requires extensive resections. The scapula is a source of flaps widely used in this region.
METHOD: A longitudinal and prospective study was carried out in a patient with protuberans cutaneous fibrosarcoma on the right shoulder who underwent resection followed by local reconstruction with a Duoscapular Flap (a combination of scapular and parascapular flaps).
RESULTS: The patient had no postoperative complications, as systemic and local complications as well as functional limitations were not observed.
CONCLUSION: Duoscapular Flap placement is a novel procedure and a relevant choice for the reconstruction of extensive wounds exposing noble structures in the shoulder. It allows the primary closure of the donor area without increasing the morbidity of the procedure.
Keywords: Duoscapular; Scapular; Parascapular; Cutaneous fibrosarcoma; Shoulder; Flap.
RESUMO
INTRODUÇÃO: O Dermatofibrossarcoma do Ombro é patologia incomum e seu tratamento demanda extensas ressecções. O sistema escapular é fonte de retalhos bastante utilizados nesta região.
MÉTODO: Realizado estudo longitudinal, prospectivo, através da condução de um caso de Dermatofibrossarcoma Protuberans em ombro direito, submetido a ressecção e reconstrução local com Retalho Duoescapular, obtido através da associação dos retalhos escapular e paraescapular.
RESULTADOS: Paciente evoluiu sem intercorrências no pós-operatório, não sendo observadas complicações sistêmicas e locais, e limitações funcionais.
CONCLUSÃO: O Retalho Duoescapular é nova e relevante opção para reconstrução de feridas extensas, com exposição de estruturas nobres no ombro. Permite fechamento primário da área doadora, sem acrescentar morbidade ao procedimento.
Palavras-chave: Duoescapular; Escapular; Paraescapular; Dermatofibrossarcoma; Ombro; Retalho.
The shoulder is a common region for cancer development, and skin grafting is widely used. The involvement of this region in cutaneous fibrosarcoma protuberans is rare, and its treatment is based on extensive resections that require great skill of the plastic surgeon in the reconstruction of this area. Scapular fasciocutaneous flaps are good options for the skin coverage of this region1. We describe an innovative application of scapular flaps, i.e., the Duoscapular Flap derived from the combination of scapular and parascapular flaps, for the treatment of cutaneous fibrosarcoma of the shoulder.
METHODS
The study material was based on the monitoring and management of this case. This is a longitudinal and prospective study. The patient was informed of the details of the procedure and signed an informed consent form. There is no conflict of interest.
Case description
The patient is a 46-year-old woman with brunette skin and without comorbidities. She has a history of nodular lesions on the right shoulder 20 years ago. Biopsies performed in the period evaluated revealed a cutaneous fibrosarcoma that evolved 2 years ago with a fibrous nodule formation on the previous surgical site, with slow and gradual growth, progressive pain, and aggravated by episodes of bleeding and drainage of necrotic material. A new biopsy confirmed the diagnosis of protuberans cutaneous fibrosarcoma.
The patient was referred to the Plastic Surgery Service of the Hospital das Clínicas of UFMG. At that time, the patient presented a large nodular, fibrous, pedunculated, and ulcerated lesion in the posterior region of right shoulder, measuring 10 × 9 × 9 cm and apparently not adhered to the deep planes. There was a large amount of drainage of necrotic material and blood (Figure 1).

Figure 1. Cutaneous fibrosarcoma. Notice the central necrotic degeneration and pedunculated aspect.
Computed tomography of the chest (Figure 2) revealed a cutaneous nodule in the posterior region of the right shoulder, without the involvement of muscle and bone planes. There were no enlarged lymph nodes and distant metastases.
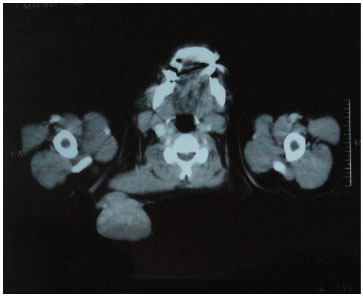
Figure 2. Computed tomography of the chest. The injury was not adhered to the deep planes.
We opted to remove the lesion with margins of 4 cm (Figure 3), and the entire mass (14 × 14 × 12 cm) containing subcutaneous tissue, trapezius muscle, and scapular periosteum was excised. No macroscopic evidence of residual lesion was seen.

Figure 3. Intraoperative wound.
The Duoscapular Flap was used for local reconstruction. This is produced by the combination of scapular and parascapular flaps to create a bilobed flap that provides adequate skin coverage for the lesion (Figure 4), in addition to the immediate closure of the donor area with minimal morbidity and no sequelae.
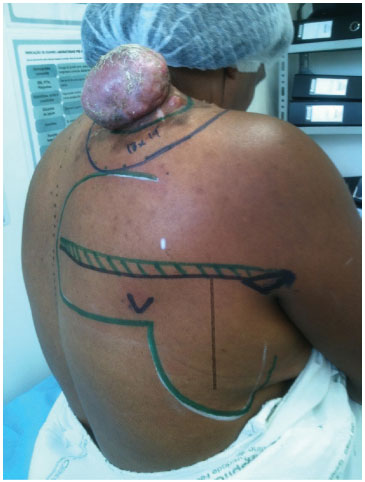
Figure 4. Marking the safety margins and the scapular flap associated with the parascapular flap.
The procedure begins with the identification of the "triangular space," the origin of scapular vessels. From this point, a horizontal line is drawn toward the spine, this being the medial limit and the axis of the scapular flap.
The lateral border of the scapula serves as a reference for marking a downward vertical line with up to 25-cm length, representing the descending branch of the circumflex artery of the scapula supplying the parascapular flap (Figure 5).
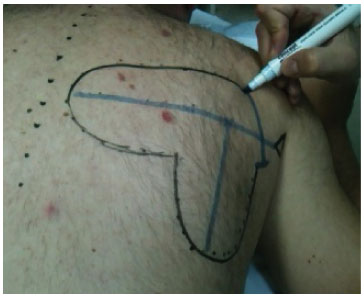
Figure 5. Marking the flap axes. Notice the triangular space.
Special attention should be given to the point of origin of the descending branch of the left circumflex artery of the scapula, which should be centered to serve as the axis for the descending portion of the flap.
The detachment begins by the wound, in the subfascial plane, releasing the flap completely until the wound closes without any degree of tension and with a perfect edge coaptation (Figure 6).

Figure 6. Detachment in the subfascial plane.
After the hemostatic revision, suture by planes was carried out with absorbable Vicryl 2.0 and 3.0, followed by Mononylon 3.0 for the cutaneous synthesis. Vacuum suction drains are positioned and then removed according to the drain (Figure 7).

Figure 7. Final aspect of the flap.
RESULTS
The patient had a positive postoperative course. She did not present any complication and was discharged on the third day of hospitalization. The anatomopathological examination led to the diagnosis of protuberans cutaneous fibrosarcoma, with free surgical margins. The patient was transferred to the Department of Clinical Oncology, where she was submitted to adjuvant therapy through radiation therapy. At present, she is under clinical follow-up and does not present signs of recurrence (Figure 8).

Figure 8. Postoperative day 40.
DISCUSSION
Protuberans cutaneous fibrosarcoma is a rare malignant neoplasm derived from dermal dendrocytes; it is highly recurrent2. It preferentially develops on the trunk and proximal region of the limbs. Usually, it tends to be initially confused with a hypertrophic or keloid scar3.
The treatment is based on its excision, with wide surgical margins (3-5 cm), removing the deep fascia or the first entire structure found3. Surgical excision is performed with 2.5 cm free margins in 95% of cases2.
The scapular fasciocutaneous flap is B type, with the vascular pedicle based on the circumflex vessels of the scapula. It is located in the posterior portion of the trunk between the armpit and the posterior midline, centered on the infraspinatus region of the scapula4.
Its size is up to 20 × 7 cm and can be vertically or horizontally oriented. It presents a constant and reliable anatomy of the vascular pedicle, easy surgical dissection, and the possibility of primary closure of the donor area4.
Its pedicle originates in the so-called triangular space (Figure 9) between the subscapularis and teres minor muscles superiorly, the teres major inferiorly, and the triceps laterally4.
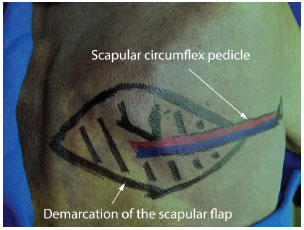
Figure 9. Scapular flap.
The cutaneous branches between the third and the fifth intercostal spaces are responsible for its innervation5.
The parascapular flap was described by Nassif et al. in 1982, who detected the continuous presence of a descending branch derived from the scapular circumflex artery6. This pedicle, responsible for flap irrigation, presents a vertical path, originating near the lateral margin of the scapula7.
It can extend inferiorly by up to 25 cm, with an average width of 7 cm (Figure 10). It is a B-type fasciocutaneous flap as described by Cormack and Lamberty7.
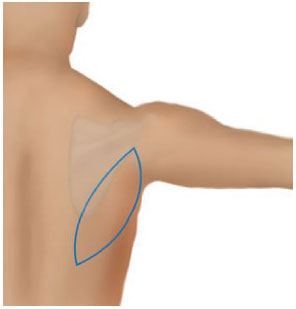
Figure 10. Parascapular flap.
Because of its shape, there are no nervous branches specific to this flap1.
Both flaps are indicated for reconstructions of defects in the shoulder, elbow, armpit, and lateral region of the chest wall. They are also used as microsurgical flaps1.
The thoracodorsal artery perforator flaps are interesting alternatives and widely used in shoulder reconstructions1,8. However, they present dermis and subcutaneous tissue that are thinner than the scapular flap, and higher emergency pedicle variation; they are located laterally, hindering the flap rotation toward the shoulder5.
Owing to the great depth and scapular bone exposure in the resulting lesion, we decided to use a fasciocutaneous flap. Muscle flaps were spared and used in case of a possible relapse.
By using the flap, we aimed for an adequate reconstruction of the injured area and immediate closure of the donor area, with minimal complications and sequelae.
The association of the irrigation principle of scapular and parascapular flaps allowed making a bilobed flap that is robust and has great vitality. The bilobed form allows making a large flap with an adequate lesion coverage that favors the primary closure of the donor area. There were no dehiscence, ischemia, infection, and functional limitations.
CONCLUSION
Protuberans cutaneous fibrosarcoma of the shoulder is a rare malignancy that is locally infiltrative and highly recurrent. It needs aggressive treatment based on extensive resections, which then require complex reconstructions.
The Duoscapular Flap proved to be reliable and effective in covering wide and deep lesions on the shoulder. It allowed the primary closure of the donor area, with better aesthetic results than grafting, and without causing morbidity and functional disability to the patient.
This flap is a new and relevant choice for the reconstruction of large wounds exposing noble structures of the shoulder.
REFERENCES
1. Chang J, Neligan PC. Plastic surgery. 3rd ed. Elsevier Health Sciences; 2012. (Hand and Upper Limb, vol. 6).
2. Mélega JM. Cirurgia plástica fundamentos e arte. Rio de Janeiro: Medsi; 2004.
3. Fleury LFF JR, Sanches JA JR. Sarcomas cutâneos primários. An Bras Dermatol. 2006;81(3):207-21. http://dx.doi.org/10.1590/S0365-05962006000300002.
4. Sevin K. Review of the free scapular flap: a versatile flap for most osteocutaneous tissue defects. Eur J Plast Surg. 2001;24(6):282-8. http://dx.doi.org/10.1007/s002380100296.
5. Ishida LH. Estudo anatômico comparativo entre o retalho escapular e o retalho perfurante da artéria toracodorsal [dissertação]. São Paulo: Faculdade de Medicina da USP; 2006.
6. Nassif TMMD, Vidal L, Bovet JLMD, Baudet J. The parascapular flap: a new cutaneous microsurgical free flap. Plast Reconstr Surg. 1982;69(4):591-600. http://dx.doi.org/10.1097/00006534-198204000-00001. PMid:7071197.
7. Klinkenberg M, Fischer S, Kremer T, Hernekamp F, Lehnhardt M, Daigeler A. Comparison of anterolateral thigh, lateral arm, and parascapular free flaps with regard to donor-site morbidity and aesthetic and functional outcomes. Plast Reconstr Surg. 2013;131(2):293-302. http://dx.doi.org/10.1097/PRS.0b013e31827786bc. PMid:23357991.
8. Thomas BP, Geddes CR, Tang M, Williams J, Morris SF. The vascular basis of the thoracodorsal artery perforator flap. Plast Reconstr Surg. 2005;116(3):818-22. http://dx.doi.org/10.1097/01.prs.0000176253.42394.7c. PMid:16141821.
1. Hospital das Clínicas, Universidade Federal de Minas Gerais (UFMG), Belo Horizonte, MG, Brazil
2. Universidade Federal de Minas Gerais (UFMG), Belo Horizonte, MG, Brazil
Institution: Study carried out at Hospital das Clínicas of Universidade Federal de Minas Gerais, Belo Horizonte, MG, Brazil.
Corresponding author:
Diogo Petroni Caiado Fleury
Universidade Federal de Minas Gerais
Av. Professor Alfredo Balena, 110 - Santa Efigênia
Belo Horizonte, MG, Brazil Zip Code 30130-100
E-mail: diogocaiadomed@gmail.com
Article received: March 3, 2013
Article accepted: September 18, 2013


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter