

Ideas and Innovation - Year 2015 - Volume 30 -
Excision of eyelid eccrine hidrocystomas via lower blepharoplasty incision
Abordagem de hidrocistomas palpebrais écrinos por incisão de blefaroplastia inferior
ABSTRACT
INTRODUCTION: Eccrine eyelid hidrocystoma is a rare cystic lesion, usually small and not exceeding 10 mm in diameter. Its treatment is usually by simple excision and biopsy. The rate of local recurrence is high.
METHODS: A patient presented with multiple bilateral hidrocystomas, several larger than 10 mm. Under local anesthesia, an infraciliary incision traditionally used for lower blepharoplasty was performed, and hidrocystomas with intact capsules were withdrawn.
RESULTS: The patient had excellent esthetic results, with no recurrence for more than six months after the procedure.
CONCLUSION: The infraciliary lower blepharoplasty incision is a promising technique for excising hidrocystomas larger than 10 mm. More studies should be conducted to confirm the good esthetic and functional outcomes of this technique.
Keywords: Hidrocystoma; Blepharoplasty; Relapse.
RESUMO
INTRODUÇÃO: O hidrocistoma palpebral écrino corresponde a lesão cística rara, usualmente de pequenas dimensões, não ultrapassando o diâmetro de 10 mm. Sua abordagem usualmente é por excisão simples e biópsia. É alto o índice de recidiva local.
MÉTODOS: Paciente com múltiplos hidrocistomas bilaterais, vários maiores que 10 mm. Sob anestesia local, foi realizada incisão infraciliar tradicionalmente usada para blefaroplastia inferior e retirada dos hidrocistomas com cápsula íntegra.
RESULTADOS: Paciente com excelentes resultados estéticos e sem recidivas até o presente momento, mais de seis meses após o procedimento.
CONCLUSÃO: A incisão infraciliar de blefaroplastia inferior é uma técnica promissora para exérese de hidrocistomas maiores que 10 mm. Mais estudos devem ser realizados para confirmação do bom resultado estético-funcional desta técnica.
Palavras-chave: Hidrocistoma; Blefaroplastia; Recidiva.
Eyelid hidrocystoma (EH) is a palpebral lesion of ectodermal origin, which mainly affects females from the fourth decade of life. It is not yet clear whether these are benign neoplasms of skin appendages or pseudoneoplastic cystic lesions1. They present as single or multiple, fluid-containing cysts, brownish in color in most cases, which can affect lower and/or upper eyelids and can be unilateral or bilateral.
The two histological types of EH, eccrine and apocrine hidrocystomas, can be differentiated by clinical examination. The first is located under the skin of the eyelid, and the second is close to the eyelashes. There is still debate about which is the more prevalent histologic type. According to a study by Schellini et al.1, of the EHs studied, almost 83% were apocrine, and only 7%, eccrine. The same study showed that EH has a prevalence of 0.07% among all eyelid lesions biopsied1.
According to the literature, there are several possible approaches to the treatment of EHs, such as excision and suturing, cauterization, and puncture and drainage. However, the major obstacle common to all these procedures is the high recurrence rate of the lesions. Here, we report on surgical excision of the lesions via a lower blepharoplasty incision.
OBJECTIVE
To present an infraciliary incision approach, as yet not described in the literature, for the treatment of eccrine EH.
METHOD
Patient GPP, a 68 year-old female, presented with bilateral large cystic lesions in the upper and lower eyelids. The first lesion had appeared four years previously in the left infraciliary region, and had a cystic appearance; the lesion was cauterized at another institute about two years previously. Bilateral local recurrence and subsequent emergence of multiple similar lesions in the upper and lower periorbital regions was observed. The patient reported pruritus in this region, but had no pain, climate-dependent lesion changes, or any change in visual acuity. There was no other treatment after the first intervention. The patient was healthy, with a history of facial hyperhidrosis, and had a 50-year-old sister with a similar single lesion on the right eyelid.
Examination revealed multiple periorbital cystic lesions, with diameters ranging from 3 to 12 mm; these were painless on palpation and consistent with a clinical diagnosis of hidrocystoma (Figure 1).
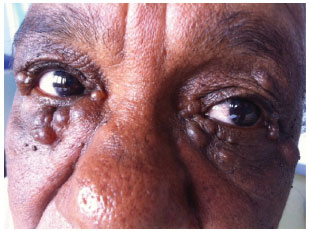
Figure 1. Preoperative photograph - Patient with large bilateral hidrocystomas.
Under local anesthesia using 2% lidocaine with epinephrine, an infraciliary transcutaneous incision was performed, following the line of the tarsus; there was immediate access to multiple cysts, which were just below the dermis, making the dissection extremely delicate. Most of the cysts were resected with an intact capsule, in order to remove the entire complex and decrease the chances of relapse. After excision of the cyst, a small ellipse of redundant skin, approximately 2 mm in width, was removed. The fat pockets were not resected. For the lesions of the upper eyelids, we opted for simple excision, with incision of the skin above the cyst. Skin suturing was performed with simple mononylon 5.0, which was removed on the fifth postoperative day. The pathological examination confirmed the diagnosis of eccrine hidrocystoma (Figures 2, 3, and 4).
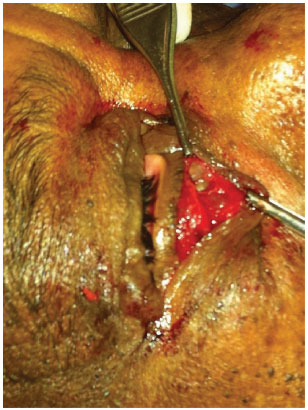
Figure 2. Start of the operation - An infraciliary incision is made under local anesthesia.
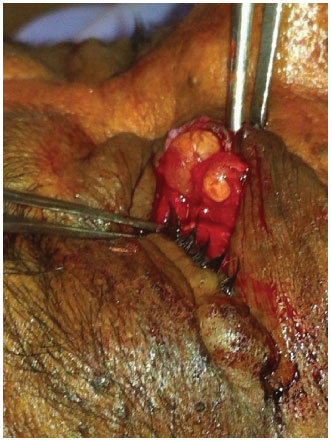
Figure 3. Careful dissection of the lesions - The already exposed, large lesions had an intact capsule.
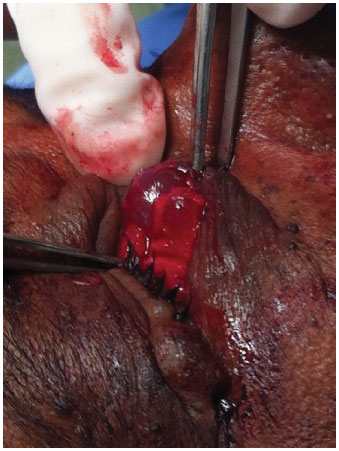
Figure 4. Extraction of the lesions - The lesions had an intact capsule.
RESULTS
A satisfactory esthetic result was obtained. At the most recent assessment, six months after surgery, the patient has had no recurrences or complications associated with the type of incision performed.
DISCUSSION
The technique used in this case has not yet been described in the literature on eccrine HPs. The only reference found concerned recurrent apocrine hidrocystoma associated with genetic syndromes2,3. The current approach proved to be useful in avoiding rupture of the lesions as far as possible; since the visual field was large, there was greater ease in identifying all lesions.
In addition, a single incision just below the eyelashes, with minimum resection of the excess eyelid skin, made it possible to leave only a virtually imperceptible scar; the patient was very satisfied with the result (Figure 5).
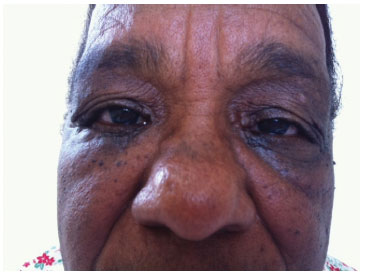
Figure 5. Postoperative photograph - The patient, six months after the procedure, had no signs of recurrence of the resected lesions.
The eccrine EH originates in the sweat gland; it is a rare cystic condition, presenting as vesicles, usually on the skin of the face and of the lower eyelid. In turn, the apocrine EH is caused by obstruction of the apocrine secretory ducts of the Glands of Moll, located in the eyelid margin. It presents as a translucent, rounded, small and painless vesicle, 1 to 3 mm in diameter1.
Clinical differentiation of these two entities is difficult, but possible. The predominant localization of an apocrine EH is next to the eyelashes and the lacrimal duct, while the eccrine EH is located under the eyelid skin1.
Histologically, the differentiation becomes simpler due to the lack of secretion by decapitation (loss of apical cytoplasm of cells of the apocrine glands) in the case of eccrine HPs. These manifest as ductal retention cysts, with only one partially collapsed cystic cavity in the dermis. Sometimes they have a brown secretion due to lipofuscin from the cells. There are no papillary projections, and they are delimited by one or two layers of cuboidal epithelial cells. A feature of apocrine hidrocystoma in the dermis is the presence of several large cystic spaces with papillary projections, coated by two layers of secretory cells. The inner cells are columnar and have eosinophilic cytoplasm4.
The etiology of eccrine EH is still questionable, but Robinson5, the first to report such a lesion, emphasized the influence of a warm climate as a predisposing factor, because droplets of sweat would accumulate more often in the glands5.
In accordance with the typical definition of eccrine EH, according to a retrospective study by Singh et al.6, hidrocystomas larger than 10 mm are very rare6.
Small and multiple lesions can be treated with CO2 laser ablation, curettage, and by chemical ablation using trichloroacetic acid or botulinum toxin. Due to the association with hyperhidrosis, anticholinergic drugs have been proposed to be effective. Treatment with topical atropine sulfate, glycopyrrolate 0.5% in aqueous solution, and oral anticholinergic agents7,8 has been reported. These treatments have been effective for multiple and small lesions; the effect on larger cysts is not known9.
The pattern in the present case differs greatly, since the hidrocystomas were bilateral, large, and confluent, and several were larger than 10 mm in the upper and lower eyelids. The patient still had small lesions in the medial edge of the upper left eyelid that were not resected during the same operation, due to the duration of surgery and prolonged discomfort expressed by the patient during the procedure.
Despite the advantages of this technique, the difficulty in dissection of cysts in relation to the dermis should be pointed out. The cysts were strongly adherent to the dermis, and the dissection was extremely delicate, in order to avoid rupture of the capsule. Due to the predictable retraction of the skin during the postoperative period, the resection of surplus skin was very judicious, with prevention of ectropion and other complications being the aim.
This aspect made the block excision much more complex; a simple juxtalesional incision was virtually impossible due to the large number and size of the lesions.
Despite the characteristic aspect of hidrocystomas, histopathological examination is always recommended, because it allows the identification of clinically similar malignant lesions.
EH remains a rarely found lesion in medical practice, and there is no consensus regarding the best management approach. It is always important to the pathological examination to confirm the benign nature of the resected lesions.
CONCLUSION
The infraciliary incision is an appropriate and promising technique for excision of hidrocystomas larger than 10 mm, and its use should be encouraged. More studies should be conducted to confirm the excellent results of this technique.
REFERENCES
1. Schellini SA, Pinto APC, Castilho CN, Achilles AB, Padovani CR, Marques MEA. Hidrocistoma écrino e apócrino na pálpebra - Casuística na Faculdade de Medicina de Botucatu - São Paulo. An Bras Dermatol. 2001;76(3):283-8.
2. Mallaiah U, Dickinson J. Photo essay: bilateral multiple eyelid apocrine hidrocystomas and ectodermal dysplasia. Arch Ophthalmol. 2001;119(12):1866-7. http://dx.doi.org/10.1001/archopht.119.12.1866. PMid:11735807.
3. Henderer JD, Tanenbaum M. Excision of multiple eyelid apocrine hidrocystomas via an en-bloc lower eyelid blepharoplasty incision. Ophthalmic Surg Lasers. 2000;31(2):157-61. PMid:10743931.
4. Alessi E, Gianotti R, Coggi A. Multiple apocrine hidrocystomas of the eyelids. Br J Dermatol. 1997;137(4):642-5. http://dx.doi.org/10.1111/j.1365-2133.1997.tb03803.x. PMid:9390347.
5. Robinson AR. Hidrocystoma. J Cutan Genitourin Dis. 1893;11:293-303.
6. Singh AD, McCloskey L, Parsons MA, Slater DN. Eccrine hidrocystoma of the eyelid. Eye. 2005;19(1):77-9. http://dx.doi.org/10.1038/sj.eye.6701404. PMid:15205675.
7. Vashi N, Mandal R. Giant multi-loculated apocrine hidrocystomas. Dermatol Online J. 2010;16(11):16. PMid:21163167.
8. Saucedo GMG, Jiménez JCM, Puya RJ, Bujaldon AR. Topical glycopyrrolate: a successful treatment for craniofacial hyperhidrosis and eccrinehidrocystomas. Dermatol Ther. 2010;23(1):94-7. http://dx.doi.org/10.1111/j.1529-8019.2009.01296.x.
9. Shimizu A, Tamura A, Ishikawa O. Multiple apocrine hidrocystomas of the eyelids treated with trichloroacetic acid. Eur J Dermatol. 2009;19(4):398-9. PMid:19467969.
Hospital das Clínicas, Universidade Federal de Minas Gerais (UFMG), Belo Horizonte, MG, Brazil
Institution: Study carried out at Hospital das Clínicas, Universidade Federal de Minas Gerais, Belo Horizonte, MG, Brazil.
Corresponding author:
Thaís Gomes Casali
Hospital das Clínicas, Universidade Federal de Minas Gerais
Rua Buenos Aires, 213, Complemento 312 - Sion
Belo Horizonte, MG, Brazil Zip Code 30315-570
E-mail: casalithais@hotmail.com
Article received: August 1, 2013.
Article accepted: January 6, 2014.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter