

Reviw Article - Year 2015 - Volume 30 -
Alterations of the myofunctional orofacial system in the Parry-Romberg syndrome: a critical literature review
Alterações do sistema miofuncional orofacial na síndrome de Parry-Romberg: revisão crítica da literatura
ABSTRACT
INTRODUCTION This qualitative literature review analyzed international scientific publications on possible orofacial myofunctional alterations in patients with Parry-Romberg syndrome by using PubMed.
METHODS: The survey was conducted in English, between 2002 and 2012, and was limited to human beings of any age. Publications without full access, duplicated by overlapping keywords, literature reviews, letters to the editor, and those not directly related to the research topic were excluded.
RESULTS: We identified 719 studies, of which 21 were within the established criteria. Based on the selected studies, patients with Parry-Romberg syndrome may show changes in soft and hard tissues such as atrophy of the sternocleidomastoid, masseter, and pterygoid muscles; atrophy in the cheek region and depression of the nasolabial fold; deviation of the lips and nose; unilateral tongue atrophy; atrophy of the mouth angle; progressive resorption of the maxilla and mandible bone; atrophy of the zygomatic arch and frontal bone, and facial asymmetry; atrophic root development or pathological resorption of permanent tooth numbers; and jaw reduction and delayed eruption of the upper and lower teeth.
CONCLUSION: Despite the growing interest in the diagnosis and symptomatic description of individuals with Parry-Romberg syndrome, publications that address functional and interdisciplinary treatments are scarce. Therefore, specific studies aimed at improving the quality of life of these patients are needed.
Keywords: Facial hemiatrophy; Stomatognathic system; Face; Facial bones; Tissue.
RESUMO
INTRODUÇÃO Esta revisão qualitativa da literatura analisou publicações científicas internacionais sobre possíveis alterações miofuncionais orofaciais em pacientes acometidos pela Síndrome de Parry-Romberg, por meio da base de dados PubMed.
MÉTODOS: O levantamento realizado limitou-se a seres humanos, de qualquer faixa etária, no idioma inglês, entre os anos 2002 e 2012. As publicações sem acesso completo, repetidas por sobreposição das palavras-chave, revisões de literatura, cartas ao editor e as não relacionadas diretamente ao tema foram excluídas.
RESULTADOS: Foram identificados 719 estudos, sendo 21 dentro dos critérios estabelecidos. Com base nos estudos selecionados, pacientes acometidos pela Síndrome de Parry-Romberg podem apresentar alterações dos tecidos mole e duro, tais como atrofia dos músculos esternocleidomastoideo, masseter e pterigoideos; atrofia na região da bochecha e depressão da prega nasolabial; desvio dos lábios e nariz; atrofia unilateral da língua; atrofia do ângulo da boca; reabsorção progressiva do osso da maxila e da mandíbula; atrofia do arco zigomático, do osso frontal e assimetria facial; desenvolvimento atrófico das raízes ou reabsorção patológica dos números de dentes permanentes; redução da mandíbula e erupção atrasada dos dentes superiores e inferiores.
CONCLUSÃO: Apesar do crescente interesse pelo diagnóstico e pela descrição sintomatológica de indivíduos com Síndrome de Parry-Romberg, a escassez de publicações que abordem tratamentos funcionais e interdisciplinares é evidente. Verifica-se a necessidade da realização de estudos mais específicos que visem à melhoria da qualidade de vida desses pacientes.
Palavras-chave: Hemiatrofia facial; Sistema estomatognático; Face; Ossos faciais; Tecido conjuntivo.
The Parry-Romberg syndrome, also known as progressive facial hemiatrophy1-16, is usually unilateral4-6,9,15-17, affecting the skin1-3,5,7,8,10-18, muscles1-3,5,7-13,16-18, fat6,9,11,18, cartilages2,6,10, and bones1-3,5,6,8-18.
Among the possible etiological causes, the most common are local facial trauma2,5,6,9,19; endocrine disorders5,6,9; autoimmunity2,5,9,10,19,20; heredity, hyperactivity, or underactivity of the sympathetic nervous system2,5,6,9,19,20; trigeminal nerve abnormality9,19; and viral infections2,5,6,9,19.
Atrophy appears in the first 20 years of life1,2,4-6,9,10,12,13,16,17,21, progressing from 2 to 10 years1,2,9 and stabilizing thereafter1,2,5,9,10. It is more common in women4,5,9.
The main symptoms associated with the pathology described in the literature are neurological changes2,11-13,17,18 such as migraines2,16-18, epilepsy2,11-13,17,18, and facial pain2,16,18, in addition to ocular complaints2,11,18 and hair loss2,11. Generally, patients take medical help regarding aesthetic complaints5 and neurological symptoms.
The most important characteristics of the syndrome are facial asymmetry6,21, which may extend from the chin to the forehead21, mouth and nose deviation to the affected side6, and unilateral teeth exposure when the lips are engaged5,6,18. When the forehead is affected, linear scleroderma can be diagnosed, and the sign in this facial region is called en coup de sabre2,11,18,21.
Treatment is multidisciplinary, involving physicians, dentists, speech therapists, and psychologists5. Surgical procedures are indicated when the disease reaches a steady status3. In addition, patients who develop facial atrophy may need counseling5.
No specific studies in the literature in the field of speech therapy discuss muscular and functional alterations of the Orofacial Myofunctional System in patients with the syndrome. Thus, before beginning clinical research on this condition, it would be necessary to determine the characterization/modification of soft tissue in patients with the syndrome, as described in related literature.
The aim of this study was to analyze scientific papers published in a refereed database that discourse on muscle and/or functional alterations of the orofacial myofunctional system in Parry-Romberg syndrome.
METHOD
This was a critical literature review performed to verify the possible orofacial myofunctional alterations in patients with Parry-Romberg syndrome. For the establishment of the research method, the precepts of the Cochrane Handbook were followed22.
The literature review was performed by using the PubMed database, and the following descriptors were crosschecked: "facial hemiatrophy," "progressive facial hemiatrophy," "stomatognathic system," "stomatognathic," "muscle," "facial," "facial bones," "skin disease," and "connective tissue." The criteria for the inclusion of articles were as follows: research in humans, written in English, and published within the 10-year period (January 2002 to July 2012).
Articles in the database were searched individually by three researchers to minimize possible quote losses. Each quote recovered in the database was analyzed independently by the study researchers in order to determine their relevance to the research and whether to include them in the study.
The quotes that did not allow access to the full text and duplicated citations by overlapping keywords were excluded from the study. Of the complete texts obtained, literature reviews and articles were excluded when not directly related to the subject, such as surgical methods, brain atrophy, specific complaints of vision, medical treatments, and life story of the authors of the studied disease.
The articles that were effectively related to the research proposal were analyzed. All stages of the study were conducted separately by the researchers, and when there was disagreement among the researchers, only articles in which the final position was consensual were included.
According to the crosscheck of the descriptors, 719 articles were initially found. Of these, only 326 were not duplicated citations because of overlapping keywords. Next, an individual analysis of the articles found by the researchers was conducted, listing 21 articles on the final consensus.
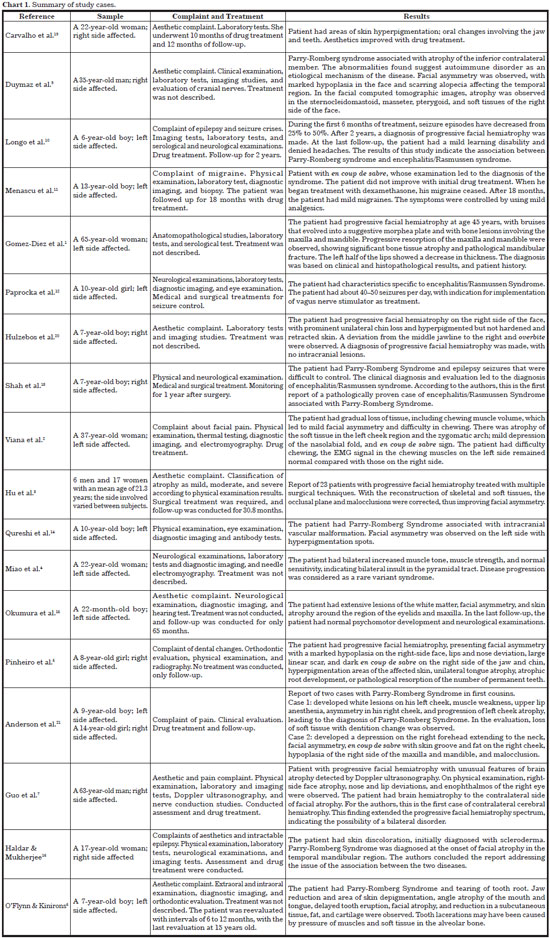
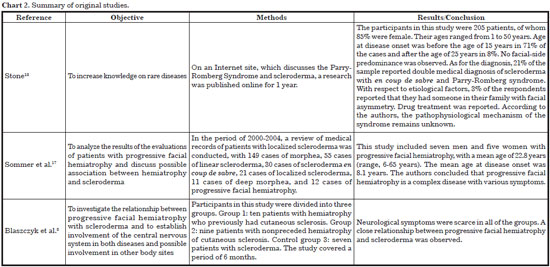
Analysis of the articles was performed, dividing the studies into two segments as follows: case reports and original articles. The parameters studied in case reports were participants' characteristics, sex, age, facial side involved, complaints, clinical findings, evaluations, treatments, time to intervention, results, and conclusions. For original articles, objectives, methods, results, and conclusions were selected as parameters.
Figure 1 shows the flowchart of the search and selection of articles for analysis in the study.
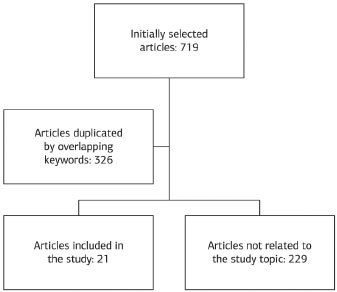
Figure 1. Flowchart of full texts selected for analysis.
RESULTS
The study results are briefly described in Chart 1 (case studies) and Chart 2 (original studies).
DISCUSSION
On the findings of this review, we observed that only a few original articles are related to the topic. Most studies report isolated cases, addressing the clinical and objective assessment, and methods for diagnosing the syndrome. We also observed that only few studies discourse about the treatment, which when approached, describes the control of neurological symptoms.
Among the case reports, 16 showed single-case descriptions1,2,4,5,7,9-17,19,20, one described the disease in two participants who were inbred cousins21, and one described the disease in 23 patients3.
In the 16 case reports of single-case descriptions1,2,4,5,7,9-17,19,20, male patients were the most affected6,7,9-11,13-15,20. According to the literature, the highest incidence of the disease is among female patients4,5,9. The left facial side has a higher prevalence1,2,4,6,10-12,14,15. The literature does not show any predominance of hemifacial involvement in the disease18.
Regarding age, we found a mean age of 20.6 years among the study patients. The youngest patient was less than 22 months old15, and the oldest patient was 65 years1. As already described in the literature, the age of atrophy onset is between the first and second decades of life1,2,4-6,9,10,12,13,16,17,21. However, in case studies, one should take into consideration that cases that are distinct from the standard are often of interest to describe.
A study that describes the Parry-Romberg Syndrome in consanguineous cases is worth reporting21. Given that the etiology of the syndrome remains unknown1-8,17,19-21, the authors pointed out the need to further investigate genetic characteristics in order to objectively define the diagnosis.
With regard to complaints, aesthetic compromise was the most frequently reported3,6,9,15,19,20, followed by epilepsy10,12,13,16 and pain2,7,11,14. The symptoms most often cited in the literature are migraine2,16,17,18, epilepsy2,11-13,17,18, facial pain2,16,18, and aesthetics5.
The assessments presented to the description of the cases were imaging tests such as radiography, magnetic resonance imaging, computed tomography, and electroencephalography2,4-7,9-12,14-16,20; laboratory tests1,4,7,9-12,14,16,19,20; physical examination2,3,6,9,11,13-16,21; neurological examination4,7,9,10,12,13,15,16; ophthalmological examination12,14,20; tissue biopsy1,11; electromyography2,4; orthodontic evaluation5,6; thermal test2, and hearing examination15.
With respect to methods of treatment, eight studies did not describe the use of treatment1,4-6,9,14,15,20, seven reported drug treatment2,7,10,11,16,19,21, two described the association between medical and surgical treatments12,13, and one described only surgical treatment3. The treatments often cited in the literature for this syndrome are drug and surgical treatments18.
From the original studies, the common goal was to describe the disease characteristics. The first article18 studied the characteristics of the disease through a questionnaire posted on a specific pathological site and involved 205 patients; the second17 retrospectively analyzed medical records of patients; and the third8 evaluated 26 individuals to verify possible comorbidities between the syndrome and other diseases.
Finally, it is worth noting the numerous muscular and functional impairments described with the syndrome that can potentially lead to changes in the superomedial orbit (SMO).
Considering that the craniofacial complex muscles are required for the integrity and functionality of SMO, the soft tissue atrophy observed in patients with Parry-Romberg Syndrome can have a direct effect on the functions performed by this complex (chewing, swallowing, speaking, and facial expressions). In the studies presented here, the following specific changes were observed: atrophy of the sternocleidomastoid, masseter, and pterygoid9 muscles; atrophy in the cheek region and mild depression of the nasolabial fold2; deviation of the lips and nose5,7; and tongue unilateral atrophy5,6 and atrophy of the mouth angle6.
Other changes described as alterations of the maxilla, jaw, and teeth can also affect the imbalance between jaw mobility and the chewing and speaking functions. Some authors also showed the involvement of hard tissue as an important atrophy of bone tissue and pathological mandibular fracture1; atrophy of the zygomatic arch, frontal bone, and facial asymmetry2; atrophic development of roots or pathological roots resorption of permanent teeth5; and reduction of jaw and late tooth eruption6. Again, this points out that the bony framework integrity of the craniofacial complex is essential for the harmonious functioning of muscles that integrates this system.
Based on this review, we consider the importance of conducting clinical studies that address issues related to speech therapy regarding the diagnosis and rehabilitation of patients with SMO changes resulting from Parry-Romberg syndrome.
CONCLUSIONS
Despite the growing interest in the diagnosis and symptomatic description of individuals with Parry-Romberg Syndrome, publications that address functional and interdisciplinary treatments are scarce. Specific studies aimed at improving the quality of life of these patients are needed.
REFERENCES
1. Gomez-Diez SG, López LG, Escobar ML, Gutiérrez LJ, Oliva NP. Progressive facial hemiatrophy with associated osseous lesions. Med Oral Patol Oral Cir Bucal. 2007;12(8):E602-4. PMid:18059248.
2. Viana M, Glastonbury CM, Sprenger T, Goadsby PJ. Trigeminal neuropathic pain in a patient with progressive facial hemiatrophy (parry-romberg syndrome). Arch Neurol. 2011;68(7):938-43. http://dx.doi.org/10.1001/archneurol.2011.126. PMid:21747035.
3. Hu J, Yin L, Tang X, Gui L, Zhang Z. Combined skeletal and soft tissue reconstruction for severe Parry-Romberg syndrome. J Craniofac Surg. 2011;22(3):937-41. http://dx.doi.org/10.1097/SCS.0b013e31820fe27d. PMid:21558914.
4. Miao J, Liu R, Lin H, Su C, Li H, Lei G, et al. Severe bilateral pyramidal tract involvement in a patient with Parry-Romberg syndrome. Am J Med Sci. 2009;337(3):212-4. http://dx.doi.org/10.1097/MAJ.0b013e31818226f9. PMid:19174689.
5. Pinheiro TPS, Silva CC, Silveira CSL, Botelho PCE, Pinheiro M, Pinheiro JJ. Progressive hemifacial atrophy--case report. Med Oral Patol Oral Cir Bucal. 2006;11(2):E112-4. PMid:16505785.
6. O'Flynn S, Kinirons M. Parry-Romberg syndrome: a report of the dental findings in a child followed up for 9 years. Int J Paediatr Dent. 2006;16(4):297-301. http://dx.doi.org/10.1111/j.1365-263X.2006.00730.x. PMid:16759329.
7. Guo ZN, Zhang HL, Zhou HW, Lan WJ, Wu J, Yang Y. Progressive facial hemiatrophy revisited: a role for sympathetic dysfunction. Arch Neurol. 2011;68(9):1195-7. http://dx.doi.org/10.1001/archneurol.2011.190. PMid:21911700.
8. Blaszczyk M, Królicki L, Krasu M, Glinska O, Jablonska S. Progressive facial hemiatrophy: central nervous system involvement and relationship with scleroderma en coup de sabre. J Rheumatol. 2003;30(9):1997-2004. PMid:12966605.
9. Duymaz A, Karabekmez FE, Keskin M, Tosun Z. Parry-Romberg syndrome: facial atrophy and its relationship with other regions of the body. Ann Plast Surg. 2009;63(4):457-61. http://dx.doi.org/10.1097/SAP.0b013e31818bed6d. PMid:19745718.
10. Longo D, Paonessa A, Specchio N, Delfino LN, Claps D, Fusco L, et al, and the Clinical and Neuroimaging Features. Parry-Romberg syndrome and Rasmussen encephalitis: possible association. Clinical and neuroimaging features. J Neuroimaging. 2011;21(2):188-93. http://dx.doi.org/10.1111/j.1552-6569.2009.00398.x. PMid:19555404.
11. Menascu S, Padeh S, Hoffman C, Ben-Zeev B. Parry-Romberg syndrome presenting as status migrainosus. Pediatr Neurol. 2009;40(4):321-3. http://dx.doi.org/10.1016/j.pediatrneurol.2008.11.007. PMid:19302950.
12. Paprocka J, Jamroz E, Adamek D, Marszal E, Mandera M. Difficulties in differentiation of Parry-Romberg syndrome, unilateral facial sclerodermia, and Rasmussen syndrome. Childs Nerv Syst. 2006;22(4):409-15. http://dx.doi.org/10.1007/s00381-005-1262-x. PMid:16247619.
13. Shah JR, Juhász C, Kupsky WJ, Asano E, Sood S, Fain D, et al. Rasmussen encephalitis associated with Parry-Romberg syndrome. Neurology. 2003;61(3):395-7. http://dx.doi.org/10.1212/WNL.61.3.395. PMid:12913207.
14. Qureshi UA, Wani NA, Altaf U. Parry-Romberg syndrome associated with unusual intracranial vascular malformations and Phthisis bulbi. J Neurol Sci. 2010;291(1-2):107-9. http://dx.doi.org/10.1016/j.jns.2010.01.003. PMid:20144465.
15. Okumura A, Ikuta T, Tsuji T, Kato T, Fukatsu H, Naganawa S, et al. Parry-Romberg syndrome with a clinically silent white matter lesion. AJNR Am J Neuroradiol. 2006;27(8):1729-31. PMid:16971623.
16. Haldar A, Mukherjee A. Parry Romberg's disease with intractable partial epilepsy. Neurol India. 2007;55(2):160-2. http://dx.doi.org/10.4103/0028-3886.32791. PMid:17558124.
17. Sommer A, Gambichler T, Bacharach-Buhles M, von Rothenburg T, Altmeyer P, Kreuter A. Clinical and serological characteristics of progressive facial hemiatrophy: a case series of 12 patients. J Am Acad Dermatol. 2006;54(2):227-33. http://dx.doi.org/10.1016/j.jaad.2005.10.020. PMid:16443052.
18. Stone J. Parry-Romberg syndrome: a global survey of 205 patients using the Internet. Neurology. 2003;61(5):674-6. http://dx.doi.org/10.1212/WNL.61.5.674. PMid:12963760.
19. Carvalho MV, Nascimento GJ, Andrade E, Andrade M, Sobral APV. Association of aesthetic and orthodontic treatment in Parry-Romberg syndrome. J Craniofac Surg. 2010;21(2):436-9. http://dx.doi.org/10.1097/SCS.0b013e3181cfe917. PMid:20216455.
20. Hulzebos CV, de Vries TW, Armbrust W, Sauer PJJ, Kerstjens-Frederikse WS. Progressive facial hemiatrophy: a complex disorder not only affecting the face. A report in a monozygotic male twin pair. Acta Paediatr. 2004;93(12):1665-9. http://dx.doi.org/10.1111/j.1651-2227.2004.tb00861.x. PMid:15918232.
21. Anderson PJ, Molony D, Haan E, David DJ. Familial Parry-Romberg disease. Int J Pediatr Otorhinolaryngol. 2005;69(5):705-8. http://dx.doi.org/10.1016/j.ijporl.2004.12.004. PMid:15850693.
22. The Cochrane Collaboration. Cochrane handbook for systematic reviews of intervention [Internet]. 2011 [acesso 2011 Maio 11]. Disponível em: www.cochrane.org/training/cochrane-handbook.
1. Instituto Central do Hospital das Clínicas, Divisão de Fonoaudiologia, Faculdade de Medicina, Universidade de São Paulo (USP), São Paulo, SP, Brazil
2. Departamento de Fisioterapia, Fonoaudiologia e Terapia Ocupacional, Faculdade de Medicina, Universidade de São Paulo (USP), São Paulo, SP, Brazil
Institution: Study performed at the Departamento de Fisioterapia, Fonoaudiologia e Terapia Ocupacional and Hospital das Clínicas of the Faculdade de Medicina of the Universidade de São Paulo (USP), São Paulo, SP, Brazil.
Corresponding author:
Claudia Regina Furquim de Andrade
Rua Cipotânea, 51 - Cidade Universitária
São Paulo, SP, Brazil CEP 05360-160
E-mail: clauan@usp.br
Article received: July 12, 2013.
Article accepted: October 30, 2013.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter