

Articles - Year 2004 - Volume 19 -
Late Evaluation of Results of Periareolar Mammaplasties
Avaliação Tardia dos Resultados das Mamoplastias por Via Periareolar
ABSTRACT
The authors studied twenty-five patients submitted to periareolar mammaplasty with a lower glandular fiap and with more than 10 postoperative years. Data studied included type and amount of breast parenchyma resection; amount of skin resection; age at the time of surgery; patient's assessment of symmetry, final volume, shape/ptosis, shape of the areolar-nipple complex (ANC) and of scars; complications and level of patient satisfaction.
Keywords: Periareolar breast; lower glandular fiap; breast plastic surgery; mammaplasty
RESUMO
São estudadas 25 pacientes submetidas a mamoplastia periareolar com retalho glandular inferior, todas com mais de 10 anos de pós-operatório.
Foram levantados dados como tipo e quantidade de ressecção do parênquima mamário; quantidade de pele ressecada; idade na época da cirurgia; avaliação do paciente referente à simetria, volume final, forma/ptose, forma do complexo aréolo-mamilar (CAM) e das cicatrizes; complicações e graus de satisfação das pacientes.
Palavras-chave: Mama periareolar; retalho glandular inferior; cirurgia plástica de mama; mamoplastia
Whenever we consider or develop a mammaplasry technique, we need to bear in mind adequate aesthetic results and the sexual and lactation functions of the breasts(1-4). The aesthetic evaluation includes shape and symmetry attained, final volume and scars. Another concern is long-term results(5-8).
Another permanent concern is the reduction of scars(9,10). Many authors have studied approaches to limit scars to the area around the areolas(11,20).
We have been performing mammaplasty using the periareolar route with a lower glandular flap, and without a contention mesh, with satisfactory results(5-8)for more than fifteen years (Figs.1-8).
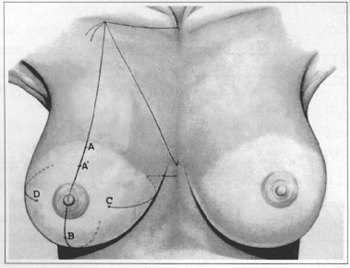
Fig. 1 - Marking of repair stitches for periareolar mammaplasty. Stitch A is 2 cm above A', which would be the mark in Pitanguy's technique.
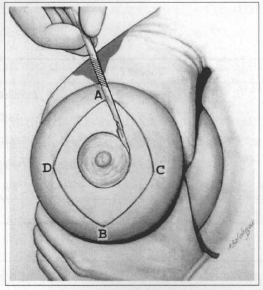
Fig. 2 - Incision in marking of ANC and on lines AC / CB / BD and AD.
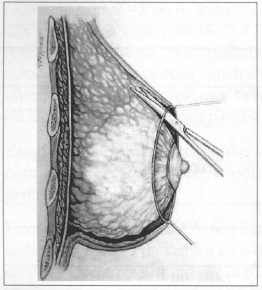
Fig. 3 - Skin is detached around me entire circumference of me breast, on the plane between subcutaneous cellular tissue and mammary parenchyma.
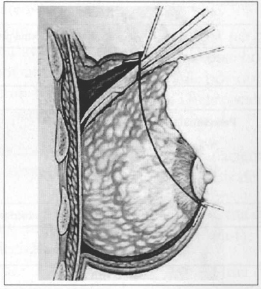
Fig. 4 - Detachment of glandular superior parenchyma, on the aponeurosis of me pectoralis major muscle.
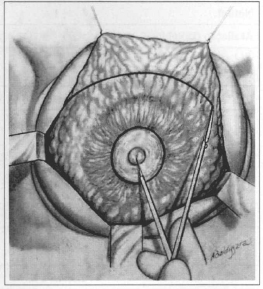
Fig. 5 - Marking of semicircle with downward concaviry with 7 to 8 cm radius from the nipple. The parenchyma is resected above th is mark.
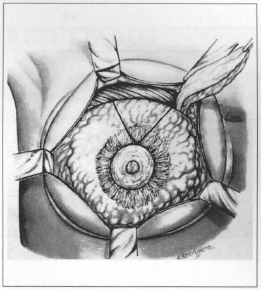
Fig. 6 - Resection of me upper pole of the mammary parenchyma and "V" mark to be resected. Resection is usually larger on me lateral pole.
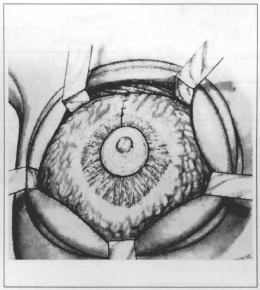
Fig. 7 - Flaps sutured on me upper pole.
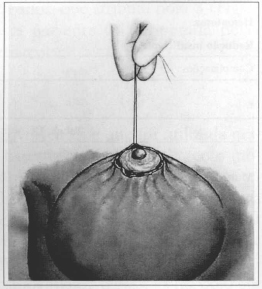
Fig. 8 - Intradermal purse-string suture with tension (round-block), bringing skin edges closer rogether to external ANC limits.
In order to prove the validity of the technique, we performed a late assessment of its results, that is, in patients with more than ten postoperative years.
METHODS
We assessed 25 randomly selected patients that had been submitted to the mammaplasty technique more than 10 years prior to the assessment. Patients were examined and interviewed in order to obtain information.
Data surveyed included type of glandular parenchyma resection (Figs. 5 and 6), amount of skin resection and age at the time of surgery. Patients were asked about 1) symmetry, 2) final volume, 3) shape/ptosis, 4) shape of ANC and 5) of scars. Patients graded each item as 2 - 1 or 0. There were 5 items, thus the final score on surgery results ranked between 0 and 10. We did not assess the surgeons' opinion because in previous srudies(5) we had observed great resemblance of their grades and patients' grades, although the latter were more strict.
We also studied the relationship between grades and age, skin resection and breast parenchyma resection.
We studied data on complications, re-operations, rates of satisfaction and the patients' decision between undergoing the present technique or a different one.
When patients came in for examination, another individual interviewed them after the consultation, in order to avoid any uneasiness.
RESULTS
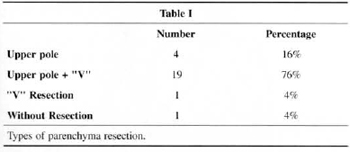
Regarding parenchyma resection (Figs. 6 and 7), there was a predominance of upper pole and "V" resections (76%) (Table I).
Regarding age, 48% were less than 19 years old, 24% were between 20 and 29, 16% between 30 and 39, and 12% between 40 and 49 years of age.
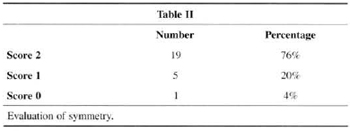
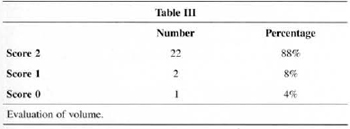
Patients ranked symmetry (76%) and volume (88%) with the highest scores (2) (Table 2 and Table 3).
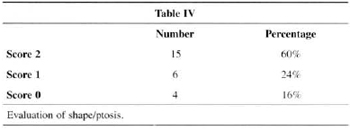
Shape/ptosis attained the highest score for 60% of patients (Table IV).
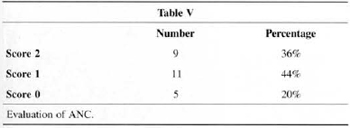
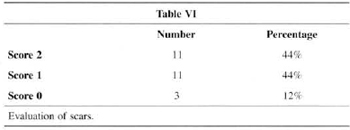
Shape of the ANC and aspect of scars, attained the highest score for 36% and 44% of patients, respectively (Table V and Table VI).
As to final scores, 16% were below 5, 16% totaled 7, 32% totaled 8, 16% totaled 9 and 16% totaled 10.
The relationships between grades and age, amount of skin resection and resection of breast parenchyma were studied (see discussion).
Complications are described in Table VII. ANC sensitivity remained the same on both sides.
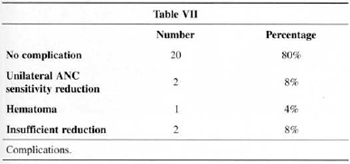
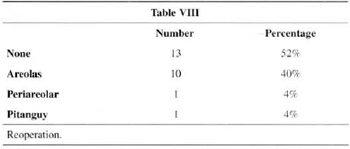
Table VIII presents the cases of re-operation with predominance of scar revision (40%).
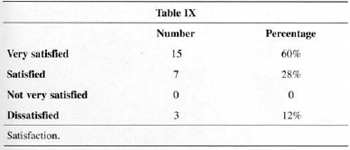
The level of satisfaction is presented in Table IX. No one referred a low level of satisfaction.
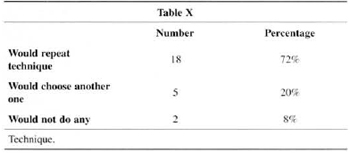
When asked what technique they would choose if they were to undergo surgery today, 71 % would repeat the same technique, 20% would choose a different one and 8% would choose neither (Table X). Two patients referred pregnancy and normal breastfeeding.
There were four patients with a postoperative of more than 10 years:
• An 18 year-old patient who gave score of 10 (Figs. 9a-f).
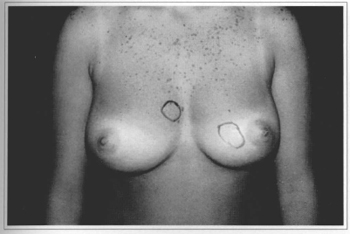
Fig. 9a - Preoperative frontal view, 18 year-old patient with mammary nodules marked.
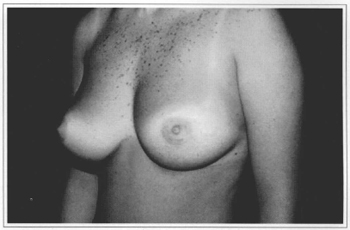
Fig. 9b - Preoperative side view.
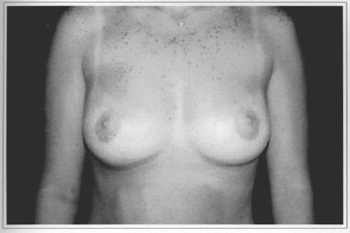
Fig. 9c - One year postoperative (after aréola correction at 6 months), with resection of 370 g from the right breast and 300 g from the left breast.
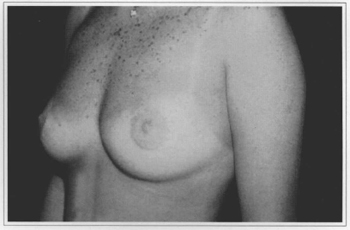
Fig. 9d - One year postoperative, side view.
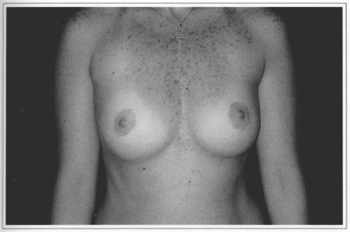
Fig. 9e - Ten years postoperative, frontal view. Gave score 10.

Fig. 9f - Ten years postoperative, side view.
• A 21 year-old patient who gave a score of 9 (Figs. 10a-f).
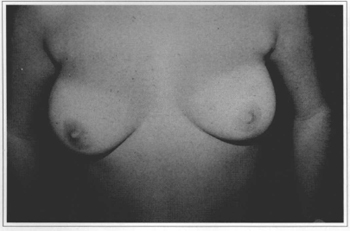
Fig. 10a - Preoperative frontal view, 21 year-old patient.
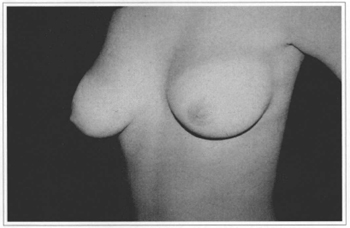
Fig. 10b - Preoperative, side view.
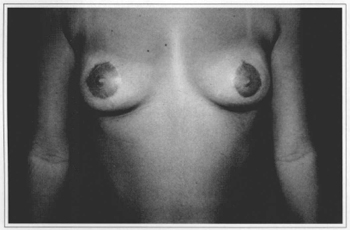
Fig. 10c - Six months postoperative (no areola correction), with resection of 220 g from the right breast and 130 g from the left breast.
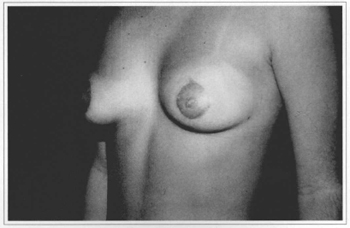
Fig. 10d - Six months postoperative, side view.
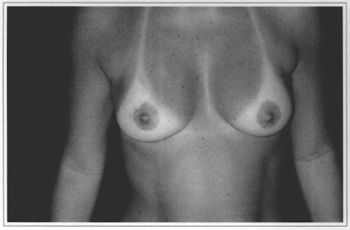
Fig. 10e - Eleven years postoperative, frontal view. Gave score 9.
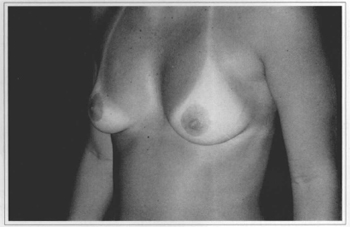
Fig. 10f - Eleven years postoperative, side view.
• A 41 year-old patient who gave a score 8 (Figs. 11a-f).
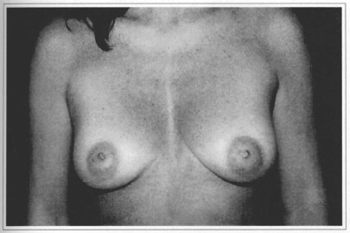
Fig. 11a - Preoperative frontal view, 41 year-old patient.

Fig. 11b - Preoperative, side view.
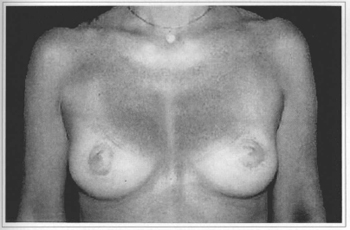
Fig. 11c - Eight months postoperative (no areola correction), with resection of 40 g from the left breast and without resection on the right breast.
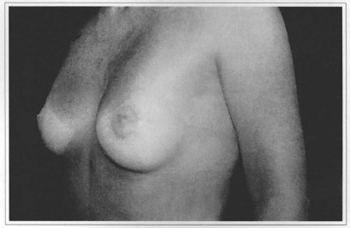
Fig. 11d - Eight months postoperative, side view.
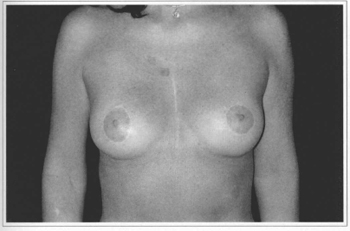
Fig. 11e - Eleven years postoperative, frontal view. Gave score 8.
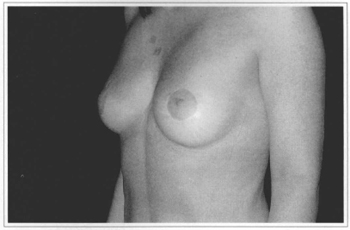
Fig. 11f - Eleven years postoperative, side view.
• A 20 year-old patient who gave a score 3 (Figs. l2a-f). This patient was re-operated on using the periareolar approach.
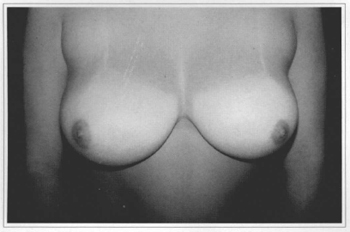
Fig. 12a - Preoperative frontal view, 20 year-old patient.
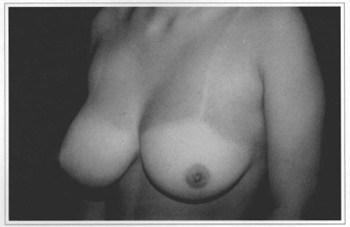
Fig. l2b - Preoperative, side view.
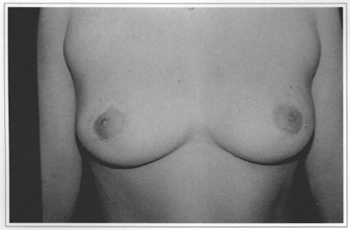
Fig. 12c - Eleven years postoperative (after areola correetion the 5th month), with reseetion of 500 g from the right breast and 350g from the left breast.
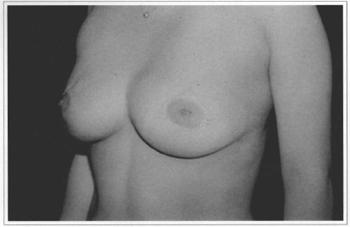
Fig. 12d - Eleven years postoperative, side view.
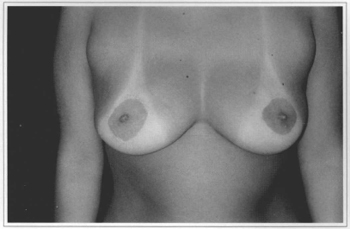
Fig. 12e - Ten years postoperative, frontal view. Gave score 3.
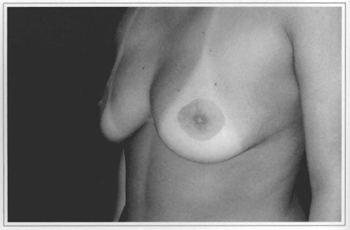
Fig. l2f - Ten years postoperative, side view.
DISCUSSION
The technique we developed and that we used on the patients srudied(5-8) is based on Bustos(12), with changes to avoid contention meshes. Meshes undoubtedly expand the indication of the technique, although authors that use them(12,14-17) have been constantly changing the material, showing some level of dissatisfaction. We resect the upper pole more and rotate lower glandular areolar flaps in the direction of upper skin. The maneuver aims to achieve a hyper-projection of the mammary cone, in order to resist the opposite pressure from the skin after the round-block(11).
Periareolar mammaplasty in general, and particularly the technique with a lower glandular flap without a contention mesh demands less skin resection than the techniques with final T, L or even vertical scars. This limits the indication of the technique to patients with very large breasts and particularly to patients with a great deal of skin flaccidity.
The results of our study (Table I) show a predominance of upper pole and "V" resections (Figs. 6 and 7) in 76% of cases, since most complaims are breast hypertrophy associated with ptosis.
There was a predominance of patients under 30 years of age (72%). This is due to the better quality of these patients' skin. Given there is less skin resection than in other techniques, we depend on satisfactory support provided by remaining skin. Naturally, older patients can also present with excellent skin texture (Fig.11).
Patients' assessment of results showed a very strong positive analysis of volume (88%) and symmetry (76%) (Tables II and III). We believe this is due to the development of the technique, with more rotation of lateral and medial flaps that allows for more projection of the mammary cone and avoids the flattened shapes observed in the early stages of the technique. The rate of satisfaction fell (60%) when shape and ptosis were analyzed (Table IV). The small amountt of skin resection and lack of elasticity are the major factors. These facts make us restrict the indication of the technigue or seek the development of support materials that are widely accepted by most surgeons and mastologists.
When we analyze ANC shape and the aspect of scars, we find the worst evaluations (Tables V and VI). We may analyze this fact in two ways. The first is that the suture of a large ring around the areolas is in fact more difficult than in other techniques and that the round-block (Fig. 10) is not always enough to hold ANC distension, especially in patients with poor skin resistance. The second way to evaluate this fact is that, like in any mammaplasry technigue, patients are strictest and complain most about scars(1,3,4,20). Because in this technigue they only exist on the areolas, complaints concentrate on this point. Probably both aspects analyzed are true, and further studies and advances are necessary regarding these items for us to expand the indication of the technique.
The analysis of final scores shows 80% of them above 7. Since the items "evaluation of ANC" and "evaluation of scars" overlapped, we observed that out of 5 items, 2 concentrated lower scores. As to satisfaction, 88% of the patients say they are very happy or happy (Table IX), which is similar to patient evaluation of other techniques(1,3,4,18-20).
In the analysis of scores in relation to age, there were some interesting facts. No patient below 19 years of age gave a score lower than 6, and all those who gave score 10 were below 29 years of age at the time of surgery.
The study of the amount of skin resection in relation to score is inconclusive, and may lead us to assume that the guality of the skin is more important than the amount resected.
When we analyze how the guantity of tissue resected relates to the score, we will notice a greater concentration of good scores in the larger resections, and all scores of 10 (4 patients) in resections above 200 g. This emphasizes the previous assumption: when having to support less weight, good skin is able to hold and keep the good shape of the new breasts.
We have included insufficient reduction in the item "complication" (Table VII) (although it is not in fact a complication) because they were the two cases that underwent reoperation, one by the periareolar technigue and the other by Pitanguy's technigue. We also noticed two cases of reduction in ANC sensitivity, both unilaterally, which indicates a problem in the execution rather than in the technigue.
In the item "reoperation" (Table VIII), the frequent incidence of areola scar revision (40%) stands out. These revisions were performed at the outpatient level under local anesthesia, 6 months after the initial surgery. By then, excess skin and tension on the areolas had already accommodated, and basically the scar was resected, with a new round-block (with thinner nylon 4-0) and intradermal suture. The control of this rype of event was straightforward so long as patients were warned preoperatively of the possibility (and in some cases the probability) of a revision being necessary.
In Table IX it is possible to see satisfaction in 88% of the cases. Of the three cases that reported dissatisfaction, two were reoperated as described above, and one did not want to undergo new surgery. The main complaint of this patient was ptosis.
In the analysis of which technigue they would choose if they were to undergo surgery today (Table X), interesting facts arose. The two patients who were reoperated said they would not undergo any surgery. And, in spite of the high satisfaction rate, four of the patients who said they were happy claimed they would choose another technigue. They all said that they would decide to place an implant, with or without skin resection, maybe as a conseguence of a current trend towards larger breasts.
The patients presented herein show consistem results when there is good guality skin, which is not totally related to age (Fig. 11). When we are dealing with thinner skin, poor in elastic fibers, (Fig. 12), we see the occurrence of ptoses and/or stretching of the areolas. The indication of this technigue should be thoroughly discussed with patients in the preoperative appointment.
CONCLUSION
• The technigue of periareolar mammaplasty with lower glandular flap attains high satisfaction rates (88%) for long-term results.
• Ir is a technique with good indication for selected cases, and it is a good option in the surgeon's armamentariurn.
• Complication rates are similar to those of other techniques.
• Further studies should be conducted to improve scar appearance.
• Scar revision rates are high (40%).
REFERENCES
1. Aboudib Jr JH, Castro CC, Coelho RS, Cupello AM. Analysis of late results in post pregnancy mammoplasry Ann Plasr Surg 1991; 26:111-6.
2. Erol OO, Spira MA. Mastopexy technique for mild to moderate ptosis. Plast Reconstr Surg 1980; 65(5):603.
3. Peixoto G. Reduction mammaplasty: a personal technique. Plast Reconstr Surg 1980; 65:217.
4. Pitanguy L Breast hypertrophy. Transaction of International Sociery of Plastic Surgeons, 2nd Congress, London, 1959. Edinburgh E. and S. Livingstone, Ltd; 1960.
5. Aboudib Ir JH. Padronização técnica da mastopatia por via periareolar e avaliação de seus resultados. Dissertação apresentada à Faculdade de Medicina da USP, para obtenção do título de mestrado em Cirurgia Plástica; 1996.
6. Aboudib Jr JH, Castro CC. Mammaplasty utilizing the periareolar approach. Aesth Plast Surg 1998; 22:51-7.
7. Aboudib Jr JH, Castro CC, Schnabi EB. Tratamento de assimetria mamária pela redução unilateral através da via periareolar. J Bras Ginecol jul 1997; 107(7):239-42.
8. Aboudib Jr JH, Mamaplastia periareolar. Atualização em Cirurgia Plástica Estética. SBCP-SO. São Paulo: Ed Robe Editorial; 1994. p. 309-13.
9. Toledo LS, Matsudo PKR. Mammoplasty using liposuction and periareolar incision. Aesth Plast Surg 1989; 13:9-13.
10. Andrews JM, Yshizuka MA, Martins DMSF, Ramos RR. An areolar approach to reduction mammaplasty. Br J Plast Surg 1975; 28:166-70.
11. Benelli L. A new periareolar technique for mammary reduction and elevation. Aesth Plast Surg 1993; 17:311-6.
12. Bustos RA. Periareolar mammaplasry with silicone supporting lamina. Plast Reconstr Surg 1992; 89(4):646-57.
13. Felicio Y.Periareolar reduction mammaplasty Plast Reconstr Surg nov 1991; 88(5)789-98.
14. Goés JCS. Periareolar mammaplasry double skin technique. Rev Bras de Cirurg Plást 1989; 4(23)55-63.
15. Goés JCS. Periareolar mammaplasry double skin technique with application of polyglactine 910 mesh. Rev da Soc Bras de Cirurg Plást Estét e Reconstr 1992; 7(1,2,3):1-6.
16. Goés JCS. Periareolar mammaplasty double skin technique with application of polyglactine or mixed mesh. Plast Reconstr Surg 1996; 97:959.
17. Goés JCS. Periareolar Mastopexy: Double skin technique with mesh support. Aesth Surg J 2003; 23:129-35.
18. Martins PDE. Periareolar mamaplasty with flap transposition. Rev da Soc Bras de Cirurg Plást 1991; 6(1,2):1-6.
19. Rosel E, Stark RB. Circum areolar mastopexy. American Society of Plastic and Reconstructive Surgeons Conventions; 1973 October 23; Hollywood, Florida.
20. Almeida CIC. Mammaplasty with L - lncison. Aesth Surg J 2004; 24:102-11.
I - Faculty of the Plastic Surgery Discipline of UERJ.
Plastic Surgery Discipline of Universidade do Estado do Rio de Janeiro (UERJ)
Address for correspondence:
José Horácio Aboudib, MD
Av. Ataulfo de Paiva, 341 - Sls. 801/02
22440-030 - Rio de Janeiro - RJ Brazil
Phone: (5521) 2511-3390 - Fax: (55 21) 2239-8927
e-mail: aboudib@mtecnet.com.br


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter