

Original Article - Year 2015 - Volume 30 -
Analysis of the clinical care of patients with chronic ulcers of the lower limbs
Análise do atendimento clínico de portadores de úlceras crônicas em membros inferiores
ABSTRACT
INTRODUCTION: Chronic ulcers of the lower limbs may have different etiologies, with the most frequent being venous, arterial, traumatic, infectious, and diabetic. The treatment of these wounds is dynamic and depends on the evolution of tissue repair. This treatment includes clinical and surgical methods, and dressings are the most frequently used. Dressings can range from inert covers to vehicles for actuation of active substances in the wound bed. The main indication for these substances is related to the effects of debridement and control of the bacterial population, enabling the preparation of wound beds for surgical or spontaneous resolution.
METHODS: This study is an observational, cross-sectional, retrospective study, with random sampling, aimed at assessing the care provided to patients with chronic ulcers of the lower limbs in the Outpatient Clinic for chronic wounds of the Plastic Surgery Division, HCFMUSP, between 2011 and 2013.
RESULTS: The clinical charts of 481 patients of both sexes, with a mean age 60 years, were analyzed; all had chronic ulcers in different stages of evolution. Comorbidities, underlying disease, size of the lesion, treatments, and evolution of wounds were evaluated. A predominance of vascular disease (69.2%) was the underlying cause. All patients were initially treated with dressings containing active agents, for preparation of the wound bed. Of these, 84% were referred for surgical management of wounds. There was no spontaneous closure in 1.5% of cases. The remaining patients (14.5%) showed worsening of lesions with topical treatment, and required other forms of preparation of the wound bed.
CONCLUSION: Topical agents may be an effective outpatient/home method to prepare the wound bed of chronic ulcers for surgical management.
Keywords: Leg ulcer; Venous ulcers; Diabetic foot; Diabetic ulcers of the foot; Healing; Papain
RESUMO
INTRODUÇÃO: Úlceras crônicas em membros inferiores podem apresentar diferentes etiologias, sendo as mais frequentes: venosa, arterial, traumática, infecciosa e diabética. O tratamento dessas feridas é dinâmico e depende da evolução da reparação tecidual. Esse tratamento inclui métodos clínicos e cirúrgicos, sendo o curativo o método não cirúrgico mais frequentemente utilizado. Curativos podem ser desde de coberturas inertes até veículos para atuação de princípios ativos no leito da ferida. A principal indicação de ativos está relacionada a efeitos de desbridamento e controle da população bacteriana, possibilitando o preparo desses leitos para resolução cirúrgica ou espontânea.
MÉTODO: Esse estudo é observacional, longitudinal, retrospectivo, de amostra randomizada no qual pretendemos analisar o atendimento prestado aos portadores de úlceras crônicas em membros inferiores no Ambulatório de Feridas Crônicas da Divisão de Cirurgia Plástica do HCFMUSP entre 2011 e 2013.
RESULTADOS: Foram analisados prontuários de indivíduos de ambos os gêneros, idade média 60 anos, portadores de úlceras crônicas em diferentes estágios evolutivos. Foram pesquisadas comorbidades, doença de base, tamanho da lesão, tratamentos utilizados e evolução das feridas. Notouse predomínio das causas vasculares (69,2%) como doenças de base. Todos os pacientes foram primeiramente tratados com curativos contendo princípios ativos, para preparo do leito das feridas. Desses, 84% foram encaminhados para resolução cirúrgica das feridas. Houve fechamento espontâneo em 1,5% dos casos. Os demais pacientes (14,5%) apresentaram piora das lesões com tratamento tópico, necessitando outras formas de preparo desse leito.
CONCLUSÃO: Agentes tópicos podem ser uma forma ambulatorial/domiciliar efetiva de preparo do leito de úlceras crônicas para resolução cirúrgica.
Palavras-chave: Úlcera de perna; Úlcera venosa; Pé diabético; Úlcera diabética do pé; Cicatrização; Papaína.
Several diseases can cause the formation of chronic ulcers in the lower limbs, and include venous, arterial, traumatic, infectious, and diabetic etiologies1. Despite the wide variety of etiological factors, the main causes of chronic ulcers of the lower limbs are venous and arterial diseases. Ulcers of venous origin affect 1% of the world's population and correspond to 75% of all chronic ulcers2.
Various studies have reported a prevalence of active, unhealed venous ulcers of approximately 0.3%, i.e., around one case per 350 adults, while the incidence of healed ulcers, regardless of their etiology, is approximately 1% in the adult population. This prevalence increases with age, and is more than 4% in people older than 65 years. When not properly managed, approximately 30% of the healed venous ulcers recur in the first year, with the rate rising to 78% after two years3.
These ulcers have significant socioeconomic impact owing to their recurrent nature and long healing time. The patient needs care from health professionals, is frequently absent from work, and often takes early retirement. All these factors are a significant burden on health and welfare systems, in addition to interfering with the patient's quality of life; the high cost of treatment or absenteeism and loss of employment do not take into account the decrease in enjoyment of daily activities3.
Venous insufficiency is the result of long-term venous hypertension caused by valve insufficiency and/or obstruction3. Ulcers due to venous insufficiency involve the skin and subcutaneous tissue, and they are predominantly found in the gaiter area, which is the region between the ankle and the lower half of the calf, and the medial leg above the medial malleolus. Their clinical characteristics include edema that worsens at the end of the day and improves with limb elevation, hyperpigmentation or dermatitis, lipodermatosclerosis, acute and progressive pain, eczema, and single or multiple ulcerations. In general, these wounds have an irregular surface shape, initially with well-defined borders and yellowish exudate. After six weeks without healing, the wound is considered chronic4.
Wound treatment depends on the evolution of the healing process, and includes clinical and surgical methods; dressings are the most common clinical treatment5.
Dressings are used to improve the condition of the wound bed, and can sometimes be definitive treatment. However, in many situations, this is only an intermediate step before surgical treatment.
Papain has been used in Brazil as a dressing for wound treatment since 19836. This extract has topical activity, primarily providing enzymatic and autolytic debridement, and acting to control the bacterial population during the preparation of the wound bed. Papain is extracted from the leaf and fruit latex of green papayas, Carica papaya, and the fruit extract is more effective that the leaf extract. Papain is a complex mixture of proteolytic enzymes and peroxidases. This active agent causes proteolysis or degradation of proteins to amino acids in devitalized and necrotic tissue, without affecting healthy tissue. Other properties of this extract are its anti-inflammatory, bacteriostatic, and bactericidal activities. The antibacterial action is only demonstrated at a concentration of 10%, by inhibiting the growth of Staphylococcus aureus and Pseudomonas aeruginosa. There are also reports of antibacterial action against Escherichia coli7.
Hydrogel is composed of water, carboxymethylcellulose (CMC), and propylene glycol (PPG); its main function is to soften and remove devitalized tissues (autolytic debridement). The water keeps the environment moist, CMC facilitates cellular rehydration and debridement, and PPG stimulates the release of exudate. Its best indication is for the treatment of superficial wounds with moderate or low exudate. Hydrogel can be combined with calcium alginate. In this situation, sodium in the exudate and blood interacts with calcium in the dressing. This ionic exchange assists in autolytic debridement, and has great capacity for absorption, thus resulting in the formation of a gel that keeps the environment moist for healing and induces hemostasis8.
The closure of the wound should be performed as soon as possible in those who present with clinical conditions and locations requiring surgical procedures. The main surgical options for resolution of these ulcers are skin grafts and local and/or free flaps9.
OBJECTIVE
The objective of this study was to retrospectively analyze the care provided to patients with chronic ulcers in the Outpatient Clinic for chronic wounds of the Division of Plastic Surgery at HCFMUSP.
METHODS
This was an observational, longitudinal, retrospective study with a randomized sample. The study was approved by the Ethics Committee for Research of the Hospital das Clinicas, Faculty of Medicine, Universidade de Sao Paulo (HCFMUSP), CAAE: 35417614.1.1001.0068.
From 2011 to 2013, 467 patients with chronic lower limb ulcers were treated in the Outpatient Clinic.
Using software specific for this purpose (Microsoft Excel random function RANDBETWEEN [1]), a sample of 68 patients was selected randomly. The patient sample had wounds in the lower limbs, included both sexes, were 42 to 86 years old (mean 60 years), and had an average presentation of approximately 7 months. The patients' medical records were evaluated for the following data: etiology, comorbidity, size of ulcers, treatment used, clinical outcome, and complications.
The treatment specified the use of different active principles and concentrations of papain formulated gel for topical use. We also evaluated the variation in treatment time with these topical agents, in addition to their use alone, or in association with other agents, and the effect on the progress of the lesion.
RESULTS
The etiological factors of chronic ulcers included vascular insufficiency, diabetes mellitus, and immunological diseases (lupus, scleroderma, psoriatic arthritis, and cutaneous tuberculosis). There was a predominance of vascular causes (69.2%). Among these, there was a higher incidence of venous ulcers (67.7%) compared to ulcers resulting from arterial occlusion (1.5%), as shown in Figure 1.
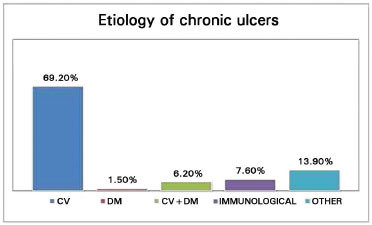
Figure 1. Etiology and incidence of diseases leading to formation of chronic ulcers of the lower limbs. Note the predominance of vascular causes in association with diabetes mellitus (CV + DM) and immunological disorders (IMMUNE). Other etiologies include traumatic ulcers and burns.
The topical agents used in the initial treatment of these wounds, as well as the variation in their concentrations, are specified in Figure 2, and were always used in daily dressing changes.
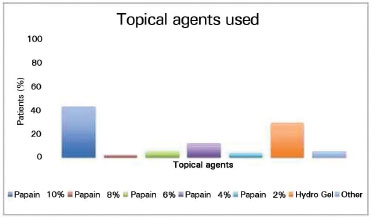
Figure 2. Description of the various topical agents used as first choice in the treatment of chronic ulcers.
The most common active agent used was 10% papain (in 19.1% of patients), followed by hydrogel (in 13.3%). In 41.2% of cases, the initial agent required replacement with a second agent to complete the treatment. Nevertheless, in 3 patients (4.5% of the cases treated with a second agent), the response was inadequate, requiring treatment other than topical management.
The initial size of the wounds evaluated was 38.75 ± 5.69 cm2. An average reduction of 6.68 cm2 was observed with topical treatment, with adequate preparation of the bed for surgical treatment after the use of dressings for a mean of 7 months. A total 4.5% of the patients had worsening of the lesions despite topical treatment, with the presence of necrotic tissue in 1.5%, and/or clinical signs of infection in 3%, leading to a mean increase of 3.53 cm2 in the original wound size. This phenomenon showed no apparent relationship with the mean age of the individuals or etiology of the lesions. Other forms of wound bed preparation were used in these patients (such as subatmospheric pressure therapy) before surgical coverage.
There was no spontaneous closure in 1.5% of clinically managed patients. However, 84% of the patients (n = 57) were referred for surgical management, with the need for hospitalization on our service, which advocates surgical treatment as early as possible, when indicated.
All patients in the study remained in follow-up in other medical specialty clinics for their underlying pathologies; however, patients with ulcers of vascular origin did not receive adjuvant treatment by the referring surgical clinic.
DISCUSSION
Chronic lower limb ulcers of venous origin affect 1% of the world's population, and correspond to approximately 75% of all chronic ulcers10. This distribution in the population was reflected in our sample, with a predominance of venous ulcers (67.7%).
These ulcers may take months or years to resolve, despite being treated appropriately. Once healed, there is the possibility of recurrence in 18% to 28% of cases if there is no follow-up and treatment of the cause. It is also well known that the size and duration affect the prognosis of these lesions11.
There are several products on the market to treat wounds, which makes the choice of a correct dressing a difficult and challenging task. In this regard, some factors should be considered12. Factors related to the wound and the adjacent skin include etiology, size, depth, anatomical location, volume of exudate, risk or presence of infection, and condition of the adjacent skin. Factors related to the patient include nutritional status, underlying diseases, need for pain control, and patient preferences. Factors related to the dressing include indications, contraindications, advantages and disadvantages, availability, durability, adaptability, and ease of use.
From the data analyzed, it is notable that topical treatments significantly improved the healing process. The literature reports that papain has been used as a topical agent in various types of wounds, in patients of different age groups, with positive effects in the stimulation of the healing process, and with a low incidence of side effects13.
Nonetheless, we should stress that the use of papain in different concentrations during different treatment phases allows better management of the progress of the ulcer, resulting in a decreased healing time and a more aesthetic appearance.
Patients who have allergic reactions to the latex of Carica papaya may present a similar reaction to papain. However, individuals who do not have this reaction can definitely apply papain to the skin14,15.
The healing time of the wound is another important factor discussed in the literature. Several studies16 have shown that treatment of chronic wounds with papain shortens the healing time. Salomé17 associated the use of EFA with papain, noting that these products are valuable resources in the treatment of wounds. In agreement with that data, our study observed an 85.5% reduction of lesions among the patients analyzed.
Papain is used in various pharmaceutical formulations in the treatment of wounds, such as powder, gel, cream, and solutions at a concentration of 2% to 10%16. Currently, a concentration of 2% is recommended for stimulation of the formation of granulation tissue, 4% to 6% to remove liquefactive necrosis, and 8% to 10% for coagulation18. In our hospital, we use papain as a gel, because this formulation maintains a moist wound environment, which is a precondition for the healing process; in addition, this avoids the inconvenience of preparation at the time of application, and it may be stored for long periods. Furthermore, it can be easily applied within the limits of the wound, and is easily removed from the lesion by washing with saline19.
This results in a net cost that is 10% of that of hydrogel, making the use of papain more in accord with the reality of the Brazilian health services.
A second agent was used to treat the injuries when there was no further need for proteolytic action or stimulation of granulation tissue or when there was an adverse response after the use of the first agent.
With regard to unsuccessful results, it is important to note that some patients interrupted treatment or were noncompliant owing to complaints of hyperalgesia or bleeding. In these cases, early surgical debridement was proposed for wound bed preparation20.
CONCLUSION
Topical agents may be an effective outpatient or home-based means of preparing the wound bed of chronic ulcers for surgical management. This treatment could reduce the need for hospitalization and reduce the socioeconomic impact of these lesions. The possibility of a shorter hospital stay has a positive effect on the quality of life of these patients, and can increase personal satisfaction in daily activities.
REFERENCES
1. Bergqvist D, Lindholm C, Nelzén O. Chronic leg ulcers: the impact of venous disease. J Vasc Surg. 1999;29(4):752-5. DOI: http://dx.doi.org/10.1016/S0741-5214(99)70330-7
2. Salomé GM, Ferreira LM. Qualidade de vida em pacientes com úlcera venosa em terapia compressiva por bota de Unna. Rev Bras Cir Plást. 2012;27(3):466-71. DOI: http://dx.doi.org/10.1590/S1983-51752012000300024
3. Abbade LPF, Lastória S. Abordagem de pacientes com úlcera da perna de etiologia venosa. An Bras Dermatol. 2006;81(6):509-22. DOI: http://dx.doi.org/10.1590/S0365-05962006000600002
4. Classer ST. A New Treatment For Sloughing Wounds. Amer J Surg. 1940;50(2):320-2. DOI: http://dx.doi.org/10.1016/S0002-9610(40)90619-5
5. Grupo Associativo de Investigação de Feridas. Escala de Cicatrizacao da Úlcera de pressão [Acesso 20 Nov 2014]. Disponível em: http://www.gaif.net/sites/default/files/
6. Leite AP, Oliveira BGRB, Soares MF, Barrocas DLR. Uso e efetividade da papaína no processo de cicatrização de feridas: uma revisão sistemática. Rev Gaúcha Enferm. 2012;33(3):198-207. DOI: http://dx.doi.org/10.1590/S1983-14472012000300026
7. Telgenhoff D, Lam K, Ramsay S, Vasquez V, Villareal K, Slusarewicz P, et al. Influence of papain urea copper chlorophyllin on wound matrix remodeling. Wound Repair Regen. 2007;15(5):727-35. DOI: http://dx.doi.org/10.1111/j.1524-475X.2007.00279.x
8. Smaniotto PHS, Ferreira MC, Isaac C, Galli R. Systematization of dressings for clinical treatment of wounds. Rev Bras Cir Plást. 2012;27(4):623-6.
9. Caldwell MD. Wound surgery. Surg Clin North Am. 2010;90(6):1125-32. DOI: http://dx.doi.org/10.1016/j.suc.2010.09.001
10. Fowkes FG, Evans CJ, Lee AJ. Prevalence and risk factors of chronic venous insufficiency. Angiology. 2001;52 Suppl 1:S5-15. PMID: 11510598
11. Jemec GB, Kerihuel JC, Ousey K, Lauemøller SL, Leaper DJ. Cost-effective use of silver dressings for the treatment of hard-to-heal chronic venous leg ulcers. PLoS One. 2014;9(6):e100582. DOI: http://dx.doi.org/10.1371/journal.pone.0100582
12. Hess CT. Tratamento de feridas e úlceras. Rio de Janeiro: Reichmann & Affonso; 2002.
13. Sanchez Neto R, Barone B, Teves DC, Simões MJ, Novo NF, Juliano Y. Aspectos morfológicos e morfométricos da reparação tecidual de feridas cutâneas de ratos com e sem tratamento com solução de papaína a 2 por cento. Acta Cir Bras. 1993;8(1):18-23.
14. Lopes PS, Ruas GW, Baby AR, Pinto CASO,Watanabe IS, Velasco MVR, Kaneko TM. In vitro safety assessment of papain on human skin: A qualitative Light and Transmission Electron Microscopy (TEM) study. Rev Bras Cienc Farm. 2008;44(1):151-6. DOI: http://dx.doi.org/10.1590/S1516-93322008000100017
15. Shi L, Ermis R, Lam K, Cowart J, Attar P, Aust D. Study on the debridement efficacy of formulated enzymatic wound debriding agents by in vitro assessment using artificial wound eschar and by an in vivo pig model. Wound Repair Regen. 2009;17(6):853-62. DOI: http://dx.doi.org/10.1111/j.1524-475X.2009.00545.x
16. Rogenski NMB, Baptista CMC, Sofia MH. O uso da papaína a 2% nas lesões provocadas pela Síndrome de Fournier: a propósito de 14 casos. Rev Paul Enferm. 1998;17(1/3):39-45.
17. Salomé GM. O enfermeiro frente ao paciente com lesão neuropática: relato de experiência. Nursing. 2007;9(107):171-5.
18. Leite AP. A Efetividade de um protocolo de uso do gel de papaína a 2% e 4% na cicatrização de úlceras venosas. [Acesso 20 Nov 2014]. Disponível em: http://www.bdtd.ndc.uff.br/tde_arquivos
19. Roque M, Souza MBB, Ferreira NMLA, Castro SLS. Uso da papaína no tratamento das úlceras por pressão: ensaio clínico randomizado e duplo cego. In: Anais de Eventos da UFSCar; 2009, São Carlos: Congresso de Iniciação Científica; 2009.
20. Grazul-Bilska AT, Johnson ML, Bilski JJ, Redmer DA, Reynolds LP, Abdullah A, et al. Wound healing: the role of growth factors. Drugs Today (Barc). 2003;39(10):787-800. DOI: http://dx.doi.org/10.1358/dot.2003.39.10.799472
Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo, São Paulo, SP, Brazil
Institution: Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo - Divisão de Cirurgia Plástica, São Paulo, SP, Brazil.
Corresponding author:
Cesar Isaac
Av Dr Arnaldo, 455 - Cerqueira Cesar
São Paulo, SP, Brazil Zip code 01246-903
E-mail: cesaris@plastica.fm.usp.br
Article received: September 5, 2014.
Article accepted: April 21, 2015.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter