

Original Article - Year 2015 - Volume 30 -
Anatomical representation of the latissimus dorsi and its application in plastic surgery
O estudo da representação anatômica do músculo latíssimo do dorso e a sua aplicação em cirurgia plástica
ABSTRACT
INTRODUCTION: The latissimus dorsi muscle (LDM) is an important element in the lateroposterior wall of the thorax. The LDM is valued in plastic surgery for its constant anatomy, and its use is recommended for mammary reconstruction, microsurgery, and upper limb reconstruction among other procedures, which makes it a versatile flap for reconstructive surgery. However, its representation in books and anatomical studies is controversial. Mathes & Nahai described that the position of the LDM is configured in a location where the muscle is found in the lateroposterior thoracic segment but with a more posterior than lateral representation. A great number of anatomists share the same opinion. The objective of this study was to discuss and describe the real position of the LDM through study of its anatomy and comparison with images published in books.
METHODS: We studied the anatomical description and representation of the LDM in drawings published in books and articles by classical authors. The drawings were compared with the neurovascular and muscular anatomy of the LDM during its dissection from 47 fresh cadavers in the dorsal decubitus (DD) position.
RESULTS: Study of the anatomical description and representation of the LDM in the revised books compared with the dissection of fresh corpses in the DD position revealed that the published authors described the LDM in a more posterior position than that found in the body.
CONCLUSION: This study identified the LDM position as being more anterior than that described by drawings in published books. LDM rotation and individualization with the patient in a DD position is a safe approach.
Keywords: Anatomy; Plastic surgery; Microsurgery; Superficial muscles of the back; Dorsal decubitus.
RESUMO
INTRODUÇÃO: O músculo latíssimo do dorso (MLD) é um importante elemento da parede látero-posterior do tórax. A aplicabilidade do MLD em cirurgia plástica é reconhecida por sua anatomia constante, sendo indicado, na reconstrução mamária, na microcirurgia, nas reconstruções de membros superiores, entre outros, tornando-se um retalho versátil em cirurgia reconstrutora. Sua representação em livros e estudos anatômicos apresentam controvérsias. Mathes & Nahai expressam que a posição do MLD é configurada em uma localização onde o músculo encontra-se em segmento torácico látero-posterior, mas com uma representação mais posterior que lateral. Um grande número de anatomistas escreve da mesma forma. O objetivo é o de discutir e descrever a real posição do MLD por meio do estudo da sua anatomia e comparação com imagens publicadas em livros.
MÉTODOS: Estudou-se a descrição e representação anatômica do MLD em desenhos publicados em livros e artigos de autores clássicos. Os desenhos foram comparados com o estudo da anatomia vásculo-nervosa e muscular do MLD durante a dissecção, na posição de Decúbito Dorsal (DD), de 47 cadáveres frescos.
RESULTADOS: O estudo da descrição e representação anatômica do MLD em livros de autores consultados, comparada com a dissecção em DD de cadáveres frescos, permitiu conhecer que estes autores identificam o MLD em uma posição mais posterior do que a encontrada na anatomia.
CONCLUSÃO: Este estudo identifica a posição do MLD com uma representação mais anterior do que os desenhos dos livros estudados. A rotação e individualização do MLD com o paciente em decúbito dorsal é uma abordagem segura.
Palavras-chave: Anatomia; Cirurgia plástica; Microcirurgia; Músculos superficiais do dorso; Decúbito dorsal.
The latissimus dorsi muscle (LDM) comprises one of the most important elements of the lateroposterior wall of the thorax1. Mathes & Nahai2 claimed that the LDM is configured in an anatomical area located in the lateroposterior thoracic segment but has a much more posterior than lateral representation.
Studies have described the little variability of the vascular anatomy of the LDM: the vascular pedicle of the LDM has a constant size and may present division into two or three intramuscular branches; the artery and vein originate at the same level and show little evidence of atherosclerosis3,4. Even in cases of anatomical variation of the thoracodorsal artery, its dimension is sufficient for it to serve as a muscle flap5.
The LDM is widely used in plastic surgery due to its only slight anatomical variability and its multiple applications3,4. The LDM flap is versatile, which enables its use in the reconstruction of thoracic deformities, such as a mammary flap, and those that involve the distal extremities, such as the apex of the scalp, plantar side of the foot, and complex lesions in the upper limbs3,4,6,7.
In LDM flap individualization and rotation, intraoperative patient position is of great importance. Positioning of the patient in the ventral and lateral decubitus position for the dissection requires an intraoperative position change for flap transference, which can increase morbidity and intraoperative time4. Performing procedures in the dorsal decubitus (DD) position eliminates the need for intraoperative position changes and creates an option for reconstructions used in repair plastic surgery4.
Here we questioned the iconographic representation of the LDM in the literature.
OBJECTIVE
The aim of this study was to discuss and describe the real position of the LDM through a study of its anatomy and vascularization in fresh corpses and by comparing it with images published in articles and books.
METHODS
This work was performed in agreement with the standards of the National Committee for Ethics in Research resolution 96/166. A total of 47 formaldehyde-untreated corpses were analyzed during the investigations on the cause of death in the Forensic Institute Estácio de Lima at the Federal University of Alagoas, and a total of 41 men and six women aged 27-50 years were included.
The corpses were dissected using a scalpel and scissors in the horizontal DD position with the arms in the abduction position. The incision performed to access the LDM was initiated with a Z-shaped cut in the axillary segment and extended longitudinally accompanying the mid-axillary line (MAL). After flap demarcation, the cadaver was positioned in the DD position with the arms in the abduction position with the aid of a hand operating table. Subsequently, a pad was placed (large surgical drape approximately 30 cm long and 14 cm in diameter folded around itself) longitudinally along the paravertebral line on the side subjected to surgery to elevate the lateral portion of the cadaver (Figure 1).
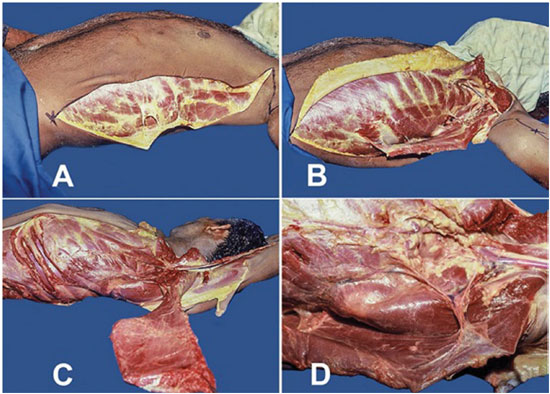
Figure 1. Demarcation and approaching the neurovascular pedicle in corpses at dorsal decubitus position - Technique by J. M. Servant. A. Incision performed with longitudinal extension along the mid-axillary line; B. Detachment of the latissimus dorsi muscle (LDM) from the thoracic segment; C. Separation of the LDM; D. Visualization of the thoracodorsal artery, vein, and nerve for the serratus muscle as well as the scapular, subscapular, and axillary circumflex arteries.
The LDM was separated in its connection to the integument and the musculocutaneous vascularization was assessed; it was also disconnected from the thoracic segment with the purpose of visualizing the thoracodorsal artery, vein, and nerve, and scapular, subscapular and axillary circumflex arteries. This study was compared with that of Bartlett et al.3
Subsequently, images illustrating the anatomical position of the LDM were analyzed and the descriptions of its anatomy in medical books were studied. The images were compared with the displays of dissected muscle from both fresh corpses and patients who underwent mammary reconstruction using the LDM in the DD position according to the technique by J.M. Servant published by Andrade4,8 with the aim of describing its real position for its procurement and use in surgical practice.
RESULTS
Using 47 corpses, we observed and registered the neurovascular and muscular anatomy of the LDM. The vases that irrigate the LDM comprise the thoracodorsal artery and vein. These vases branch from the subscapular artery and vein, which give origin to the axillary artery and vein, respectively. In our case series, 90% of the dissected corpses (41/47 corpses) presented similar anatomy with the vein adjacent to the artery and a predominance of the posterior artery adjacent to the vein. Only in 10% of cases was the origin of the subscapular artery not adjacent to the subscapular vein.
After the axillary vases originate, the subscapular artery and vein bifurcate in the circumflex vases of the scapular and thoracodorsal vases, which was observed in 68% of dissections (32/47). The double scapular circumflex vein was observed in 10.6% (5/47) and the double scapular circumflex artery in 12.7% (6/47). In 18%, small branches of the subscapular artery were observed prior to the bifurcation of the subscapular artery into the scapular circumflex and thoracodorsal arteries.
The blood supply of the LDM occurs through the thoracodorsal artery and vein. In its course, the artery may originate one, two, or three branches before penetrating the muscle. A unique branch was observed in 53.2%, two branches were observed in 45.8%, and three branches were observed in 1% of cases.
In all dissections (100%), the lateral limits of the LDM were observed to be located in the segment between the MAL and the anterior axillary line (AAL) with the patient in the DD position. The MAL is defined as the line that follows the apex, the deepest part of the axillary fossa, parallel to the AAL, whereas the AAL is defined as the line that follows vertically along the anterior axillary fold that is formed by the lateral lower border of the pectoralis major muscle when it passes the rib cage into the humerus1.
Analyzing the anatomical representation of the LDM in works and books from revised authors was a way to assess the real anatomical position of this muscle. According to Strauch & Yu9, in Atlas of Microvascular Surgery published in 1992, the LDM has a thin tendinous insertion with an incorrect orientation of the muscle fibers and is represented by a completely posterior position, and there is a decrease in the size of the muscle in the craniocaudal direction (Figures 2A, 2B). The studies by McCraw et al.10 and Tobin11 in Clinics in Plastic Surgery published in 1979 and 1990 showed a drawing in which the LDM was located in a more posterior segment and the representation of its vascularization was positioned in the same topography of the muscle fibers (Figures 2C, 2D). The study by Hochberg12, Myocutaneous Flap Manual, published in 1984 represents the LDM in a similar manner to that by Strauch & Yu9 (Figure 2E). According to Mathes & Nahai2 in Clinical Applications for Muscle and Musculocutaneous Flaps published in 1982, the LDM is represented as being situated completely within the dorsal segment of the human body (Figures 2F, 2G, and 2H). On the other hand, in the study by Bostwick13, Breast Reconstruction: A Comprehensive Approach published in 1979, the LDM was represented in a similar way to that published by McCraw et al.10 and Tobin11 (Figure 2I).
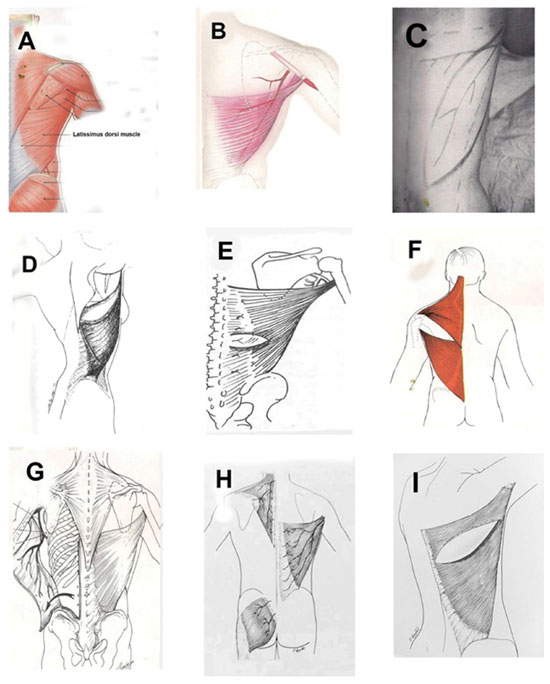
Figure 2. Classical anatomical representations of the latissimus dorsi muscle. A and B: Atlas of Microvascular Surgery, Strauch, pp. 324 and 484; C and D: Clinics in Plastic Surgery, Mccraw & Tobin, pp. 65 and 685; E: Myocutaneous Flap Manual, Hochberg, p. 134; F, G and H: Clinical Applications for Muscle and Musculocutaneous Flaps, Mathes & Nahai, pp. 165, 237, and 349. I: Breast Reconstruction: a Comprehensive Approach, Bostwick J 3rd. Clin Plast Surg. 1979;6(2):143-62.
DISCUSSION
This vascular study of the subscapular artery and its branches was similar to that by Bartlett et al.3 (Table 1, Figure 3). The LDM is a component of the lateroposterior wall of the thorax, and knowledge of its topography is of great importance for its identification during surgery. This muscle is large, with a triangular base and external axillary apex, and covers an extensive part of the dorsal region. The muscle presents in the form of a hand fan, extending from the torso to the humerus and acting directly on the shoulder articulation and indirectly on the scapulothoracic articulation (upper limb cingulate)1.
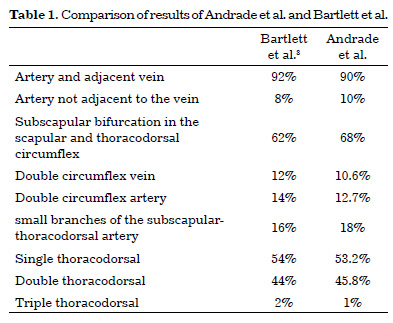

Figure 3. 1. Artery and axillary vein ; 2. Artery and subscapular vein ; 3. Artery and scapular circumflex vein ; 4. Thoracodorsal artery, vein, and nerve; 5. Division of the thoracodorsal neurovascular bundle of the latissimus dorsi muscle. 6. Branch for the serratus muscle.
The LDM originates from the thoracolumbar fascia, traverses the T2-L5 spinous processes, dorsal side of the sacro and iliac crests, and the muscular fascicules from the three or four lowest ribs to connect with the external oblique muscle of the abdomen. Its insertion is formed by a terminal tendon that is 7-10 cm long and 0.5-1.5 cm wide after an axial torsion of 180º at the bottom of the humerus bicipital canal. Its motor innervation occurs through the thoracodorsal nerve, a branch of the posterior cord of the brachial plexus, and the sensory innervation of the skin that covers the muscle is performed by the perforating branches of the intercostal nerve, which is located 3 cm below the vases1. The primary vascularization of the LDM is performed by the thoracodorsal artery, which, together with the scapular circumflex artery, forms the terminal branch of the subscapular artery14. It is important to identify the route of the subscapular artery and vein, which will be descendent, and its differentiation into the thoracodorsal artery will occur after the subscapular artery and vein emit the scapular circumflex artery and vein. The thoracodorsal artery may emit branches for the anterior serratus muscle and teres major muscle, and, when penetrating the LDM, it bifurcates into horizontal and vertical muscular branches, thus forming the musculocutaneous perforators3,15,16. The secondary vascularization is performed by perforating branches of the posterior intercostal artery and posterior lumbar artery17,18.
In the representations from the literature, in the books of the revised authors, it was observed that the LDM is located much more posteriorly than anteriorly, being almost completely visualized in anatomical models that show the posterior wall of the thorax with little or no lateral portion, a claim that contrasts with what was found in the dissections performed here as well as in surgical practice. The overlook of the real position of the LDM may have caused the surgeons to decrease the versatility and recommended the use of this muscle. The term "line," when restricted to body surface areas, does not have delimited parameters; thus, the importance of the identification of the MAL is important to the delimiting of the start of the body segment defined as the AAL and the identification of the anterior margin of the LDM that is located between two imaginary lines.
In the study by Andrade et al.4, a dynamic evaluation of the LDM was performed with the patient standing or sitting with forced arm adduction and the hands over the iliac crests. The demarcation of the anterior limit was initiated with the muscle under contraction with the objective of visualizing and palpating the anterior margin of the LDM. After flap demarcation, the patient was placed in the DD position with the arms in an abduction position with the aid of a hand operating table. Subsequently, a pad (large surgical drape approximately 30 cm long and 14 cm in diameter folder over itself) was placed longitudinally along the paravertebral line on the surgically targeted side to laterally elevate the patient. The approach of the neurovascular pedicle was initiated after flap demarcation through an inverted V-shaped incision in the upper border of the ellipse that delimited the flap with a medial apex and angle of approximately 140º that involved the skin and subcutaneous cellular tissue. The incision was subsequently extended according to the drawing of the desired flap and constitution. The rotation axis of the flap corresponds to the origin of the vascular pedicle, which is located in the center of the axillary fossa, with the arm in a completely elevated and abducted position.
The use of the DD position when creating microsurgical flaps of the LDM enables the following: the possibility of two teams working concomitantly during the procedure, one working on the donor site and the other on the recipient site, decreasing the intraoperative time; simplification of the surgical procedure, with greater comfort for the surgeon, who can perform the entire dissection and hemostasis more easily while sitting since there are no changes in patient position; ease of synthesis of the donor area; and facilitation of the pedicle, which is short when it penetrates the LDM and is near the anterior margin of the muscle, with the DD position and with the arms naturally in abduction. The degree of difficulty of the surgical procedure with the patient in the DD position, which cannot be compared with that in the revised literature due to lack of elements, should be highlighted; however, the position for individualization of the LDM is achievable and, based on the case series of Andrade et al.4, complications strictly due to the surgical position have not occurred.
The visualization of muscle dissection in formaldehyde-untreated cadavers demonstrated the feasibility of the procedure, showing that it is possible for the LDM to be completely individualized with the patient in the DD position, which would not have been possible if its location was consistent with that shown in the literature. It is important to perform studies on the anatomy of the LDM along the dorsal, lateral, and anterior topography to better define its real position.
CONCLUSION
This study allowed us to conceptualize that the vascular anatomy of the LDM presents little variation and that it is not exclusively located in the posterior region of the thorax but is set in a much more lateral position than that represented in the articles and books of the revised authors, which enables surgery and dissection of this muscle with the patient placed in a horizontal DD position.
REFERENCES
1. Moore KL, Dalley AF. Anatomia orientada para a clínica. 5a ed. Rio de Janeiro: Guanabara Koogan; 2007.
2. Mathes EJ, Nahai F. Clinical applications for muscle and musculocutaneous flaps. Toronto: Mosby; 1982. p.733.
3. Bartlett SP, May JW Jr, Yaremchuk MJ. The latissimus dorsi muscle: a fresh cadaver study of the primary neurovascular pedicle. Plast Reconstr Surg. 1981;67(5):631-6. DOI: http://dx.doi.org/10.1097/00006534-198105000-00010
4. Andrade FAG, Servant JM, Ferreira LM, Revol M, Traber H, Nascimento Júnior CP, et al. O decúbito dorsal nos retalhos microcirúrgicos do músculo latíssimo do dorso - Técnica de J. M. Servant. Rev Soc. Bras Cir Plast. 2000;15(2):35-46.
5. Rowsell AR, Davies DM, Eisenberg N, Taylor GI. The anatomy of the subscapular-thoracodorsal arterial system: study of 100 cadaver dissections. Br J Plast Surg. 1984;37(4):5746. DOI: http://dx.doi.org/10.1016/0007-1226(84)90152-8
6. Andrade FAG. Decúbito dorsal nos retalhos microcirúrgicos do Músculo Grande Dorsal [Dissertação de Mestrado]. Universidade Federal de São Paulo. Escola Paulista de Medicina. São Paulo; 1998.
7. Mahboub T, Ghareeb F, Said TA, Abdelnaser WS. The reconstructive and functional role of latissimus dorsi flap in complex upper extremity injuries. Egypt J Plast Reconstr Surg. 2003;27(2):255-61.
8. Andrade FAG, Cavalcanti CO, Acioli Neto TL, Mota PKV, Nascimento RPN. O decúbito dorsal nos retalhos microcirúrgicos do músculo latíssimo do dorso - "técnica de Jean Marie Servant". An Fac Med Univ Fed Pernamb. 2002;47(1).
9. Strauch B, Yu HL, eds. Atlas of microvascular surgery: anatomy and operative approaches. Nova York: Thieme; 1992. p.560.
10. McCraw JB, Bostwick J 3rd, Horton CE. Methods of soft tissue coverage for the mastectomy defect. Clin Plast Surg. 1979;6(1):57-69.
11. Tobin GR. Segmentally split pectoral girdle muscle flaps for chest-wall and intrathoracic reconstruction. Clin Plast Surg. 1990;17(4):683-96. PMID: 2249389
12. Hochberg J, ed. Manual de retalhos miocutâneos: axiais, osteomiocutâneos, musculares, fasciocutâneos e livres. Porto Alegre: AMRIGS; 1984. p.443.
13. Bostwick J 3rd. Breast reconstruction: a comprehensive approach. Clin Plast Surg. 1979;6(2):143-62.
14. Costa KCM, Kiyohara LY, Jorge HMH, Araújo MP, Torres LR, Barros Filho TEP. Estudo do alcance do retalho do músculo grande dorsal para o revestimento cutâneo da coluna. Acta Ortop Bras. 2009;17(5):305-8. DOI: http://dx.doi.org/10.1590/S1413-78522009000500011
15. Rowsell AR, Eisenberg N, Davies DM, Taylor GI. The anatomy of the thoracodorsal artery within the latissimus dorsi muscle. Br J Plast Surg. 1986;39(2):206-9. DOI: http://dx.doi.org/10.1016/0007-1226(86)90083-4
16. Saijo M. The vascular territories of the dorsal trunk: a reappraisal for potential flap donor sites. Br J Plast Surg. 1978;31(3):200-4. DOI: http://dx.doi.org/10.1016/S0007-1226(78)90082-6
17. Taylor GI, Palmer JH. The vascular territories (angiosomes) of the body: experimental study and clinical applications. Br J Plast Surg. 1987;40(2):113-41. DOI: http://dx.doi.org/10.1016/0007-1226(87)90185-8
18. Watanabe K, Kiyokawa K, Rikimaru H, Koga N, Yamaki K, Saga T. Anatomical study of latissimus dorsi musculocutaneous flap vascular distribution. J Plast Reconstr Aesthet Surg. 2010;63(7):1091-8. DOI: http://dx.doi.org/10.1016/j.bjps.2009.05.042
1. Universidade Federal de Alagoas, Maceió, AL, Brazil
2. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
Institution: Faculdade de Medicina, Universidade Federal de Alagoas, Maceió, AL, Brazil.
Corresponding author: Fernando Gomes de Andrade
Rua José Freire Moura, nº 191/104, Ponta Verde
Maceió , SP, Brazil Zip Code 57000-000
E-mail: fernandogomes1911@hotmail.com
Article received July 19, 2013.
Article accepted April 22, 2015.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter