

Original Article - Year 2015 - Volume 30 -
Breast reconstruction with autologous tissue: 380 consecutive cases
Reconstrução mamária com tecido autólogo: 380 casos consecutivos
ABSTRACT
INTRODUCTION: Breast reconstruction plays an important role in the treatment of breast cancer. Several options are available for autologous breast reconstruction, the more widespread being the transverse rectus abdominis myocutaneous (TRAM) flap, the latissimus dorsi myocutaneous (LDM) flap, and the local muscle (LM) flap. The objective of this work was to demonstrate the initial experience in breast reconstruction with autologous tissue, with or without implants.
METHOD: A retrospective analysis was performed of medical charts of 367 patients who underwent immediate and delayed breast reconstruction with the unipediculated TRAM flap, LD flap, or LM flap.
RESULTS: Three hundred eighty breasts were reconstructed. There were 156 TRAM flap procedures, 179 LD flap procedures, and 49 other techniques. The size of the implants ranged between 155 cc and 640 cc. The mean age of the patients was 49.33 years. One hundred ninety-seven patients underwent surgery on the right side and 169 on the left; 14 patients underwent bilateral reconstruction. Reconstruction was immediate in 80% of the patients. There were few moderate (partial dehiscence of the wound requiring suturing) and severe complications (flap liponecrosis, extrusion of the implant after infection, and pulmonary thromboembolism) and some minor complications that did not require surgical correction.
CONCLUSIONS: Breast reconstruction with autologous tissue provides the plastic surgeon with a consistent and reliable method of breast reconstruction, with very satisfactory aesthetic results and low morbidity in selected patients.
Keywords: Mammoplasty; Surgical flaps; Muscles; Breast tumors; Reconstructive surgical procedures.
RESUMO
INTRODUÇÃO: A reconstrução mamária desempenha papel importante no tratamento do câncer de mama. Várias opções estão disponíveis para a reconstrução autóloga, sendo as mais difundidas o retalho do reto abdominal (TRAM), o retalho de grande dorsal e retalho muscular local. O trabalho visa demonstrar a experiência inicial na reconstrução mamária com tecido autólogo, acrescido ou não de implante.
MÉTODO: Foi realizada análise retrospectiva de prontuários de 367 pacientes que foram submetidas à reconstrução mamária imediata e tardia com retalho do reto abdominal (TRAM) unipediculado ou retalho de grande dorsal (GD) ou retalho muscular local (RL).
RESULTADOS: Foram reconstruídas 380 mamas. Em 156 pacientes, a técnica foi TRAM; em 179, GD; e, em 49 pacientes, outras técnicas foram empregadas. O tamanho dos implantes variou entre 155 cc e 640 cc. A idade média das pacientes foi de 49,33 anos. 197 pacientes foram operadas do lado direito, 169 do lado esquerdo e em 14 pacientes a reconstrução foi bilateral. A reconstrução foi imediata em 80% das pacientes. Houve poucas complicações moderadas (deiscência parcial da sutura, com necessidade de ressutura) e graves (liponecrose do retalho, extrusão do implante após infecção e tromboembolismo pulmonar) e, ainda, algumas complicações menores que não demandaram correção cirúrgica.
CONCLUSÕES: A reconstrução mamária com tecido autólogo fornece ao cirurgião plástico um método consistente e confiável de reconstrução mamária, com resultados estéticos muito satisfatórios e com morbidade pequena para pacientes selecionadas.
Palavras-chave: Mamoplastia; Retalhos cirúrgicos; Músculos; Neoplasias da mama; Procedimentos cirúrgicos reconstrutivos.
Breast cancer remains one of the most common malignant tumors in women and is one of the major causes of cancer-related mortality.
The adoption of more urbanized lifestyles and changes in reproductive behavior may be involved in the increased worldwide incidence of this cancer1.
Despite the current emphasis on conservative breast surgery, the rates of mastectomy remain around 30%2. Mastectomy is often associated with significant psychological sequelae, including body-image distortion and sexual dysfunction. The restoration of the breast allows emotional and physical recovery, even partially, after the trauma inflicted by the disease2.
Breast reconstruction plays an important role in the treatment of breast cancer. The indication to implement it or not and the choice of the technique are individualized decisions, which should take into account the medical staff and the patient.
Advances in breast reconstruction and mastectomy techniques have increased expectations as to the outcome. Options include placement of breast implants or use of autologous tissue. The advantages of autologous reconstruction are the creation of a soft breast cone, with natural ptosis, which tends to be more similar to the contralateral breast, either with or without the use of a bra3,4. In addition, the thick dermis of autologous tissue allows for excellent results in reconstructions of the nipple-areolar complex5. The results obtained with reconstruction methods tend to change less over time and do not require periodic reviews as seen in reconstructions exclusively with implants4.
Several options of donor areas of tissue are available for autologous reconstruction. The more widespread are the transverse rectus abdominis myocutaneous (TRAM) flap, the latissimus dorsi myocutaneous (LDM) flap, the gluteus maximus flap, and the local muscle (LM) flap.
OBJECTIVE
The present work aimed to demonstrate the experience of the authors in breast reconstruction after mastectomy with autologous tissue, with or without silicone breast implants, by discussing epidemiological data and comparing it with published worldwide data, and to verify the applicability of the technique in the team's clinical practice.
METHODS
All 367 patients who underwent surgery between July 2006 and January 2014 were analyzed. This retrospective study followed the Principles of Helsinki. The patients underwent immediate or delayed breast reconstruction with the use of the following techniques: the TRAM flap, LDM flap, LM flap, and lateral thoracodorsal (Hölmstrom) flap; the last 3 procedures were associated with the insertion of silicone breast implants. When implants were used, they were natural-shaped, extra-high-projection, textured-surface implants.
The selection of the technique to be employed in each case initially followed the criteria outlined, and the final decision was taken together with the patient. Patients without abdominal obesity, non-smokers, and those without prior abdominal scarring (with the exception of a Pfannenstiel incision) were selected to be submitted to reconstruction with the TRAM flap. Patients with any of these conditions or who expressed the desire to become pregnant after the treatment were selected for reconstruction with the LDM flap. Finally, patients who requested smaller surgeries or had major comorbidities such as lung or heart diseases underwent reconstruction with the LM flap or Hölmstrom flap.
The technique used for reconstruction with the latissimus dorsi was described by Bostwick and Scheflan6, and involved creation of a transverse skin island on the dorsum and insertion of an implant in a muscular pocket between the latissimus dorsi flap and the greater pectoral muscle. Between 20 and 25 adhesion sutures were performed in the donor area to reduce the incidence of seroma and tension at the edges of the incision.
The technique used for reconstruction with the TRAM flap was described by Hartrampf6 and involved creation of a horizontal dermofat island, unipediculated and contralateral to the mastectomy defect, using areas 1 and 2 in full for the reconstruction of the breast and up to 30% of area 3. Area 4 was always discarded. Prior flap autonomization of the flaps was not followed. Reconstruction of the abdominal wall was performed with direct closure of the aponeurosis above the navel and affixing and suture of polypropylene mesh in the infraumbilical paramedian area.
Reconstruction with a local muscle flap was performed by detaching the greater pectoral muscle, serratus anterior muscle, and aponeurosis of the rectus abdominis, and constructing a muscular pouch between these structures to completely cover the silicone implant. In cases where it was necessary to recruit adjacent skin, the technique described by Hölmstrom with a lateral thoracic fasciocutaneous flap was used6.
In all cases, active drainage was performed in donor and recipient areas. The average length of hospital stay was 2 days. The surgical time ranged from 1 hour (LM flap) to 3 hours (bilateral LDM flap), with an average of 1 hour and 40 minutes (unilateral LDM flap) or 1 hour and 50 minutes (TRAM flap).
Prophylaxis for venous thrombosis was performed in all patients, following the protocol of the Brazilian Society of Angiology and Vascular Surgery7. Antibiotic prophylaxis with 2nd generation cephalosporin (intravenous) was prescribed for 2 days, followed by 1st generation cephalosporin (oral) until the drain was removed.
In patients reconstructed with the TRAM flap, the use of an abdominal and breast shaper after surgery was maintained continuously for 30 days after surgery and only during the day for 60 days. No shaper or special bra was used in patients reconstructed with LDM or LM flaps.
RESULTS
In total, 367 patients underwent surgery and 380 breasts were reconstructed in 384 surgical procedures. Regarding the surgical technique, there were 156 TRAM flap procedures (Figures 1 to 5), 179 LDM flap procedures together with insertion of a silicone breast implant (Figures 6 to 10), and 49 other techniques such as the LM flap (40 procedures) (Figure 11) and Hölmstrom flap (9 procedures) (Figure 12). The size of the implants ranged between 155 cc and 640 cc; the most frequently used volumes were 365 cc and 425 cc with the extra-high projection profile.

Figure 1. Postoperative appearance of the left breast after delayed reconstruction with the transversus rectus abdominis myocutaneous (TRAM) flap involving reconstruction of the nipple-areolar complex (NAC) and contralateral mammoplasty (frontal view).

Figure 2. Postoperative appearance of the left breast after delayed reconstruction with an autologous flap involving reconstruction of the NAC and contralateral mammoplasty (profile view).

Figure 3. Postoperative appearance of the left breast after immediate reconstruction with an autologous flap involving reconstruction of the NAC and contralateral mammoplasty (frontal view).

Figure 4. Postoperative appearance of the left breast after immediate reconstruction with an autologous flap involving reconstruction of the NAC and contralateral mammoplasty (profile view).

Figure 5. Postoperative appearance of the left breast after immediate reconstruction with the TRAM flap in skin-sparing mastectomy after radiotherapy.
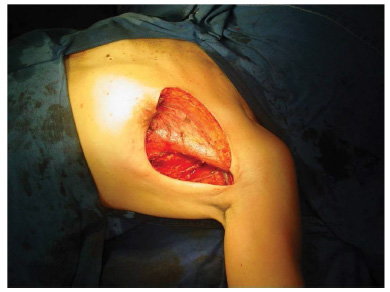
Figure 6. Transoperative representation of immediate reconstruction of the left breast.
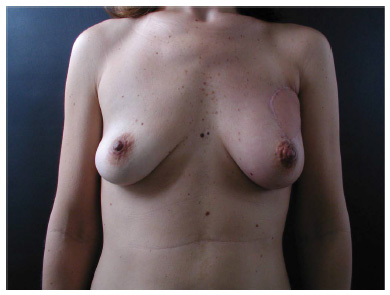
Figure 7. Postoperative appearance of the left breast after immediate reconstruction with the latissimus dorsi myocutaneous (LDM) flap in skinsparing mastectomy.

Figure 8. Preoperative image of nipple-sparing mastectomy.

Figure 9. Postoperative appearance of the left breast after immediate reconstruction with the LDM flap in nipple-sparing mastectomy.

Figure 10. Postoperative appearance of the left breast after immediate reconstruction with the LDM flap showing the position of the scar on the dorsum.

Figure 11. Postoperative appearance of the left breast after immediate reconstruction with the local muscle flap involving prosthetic reconstruction of the NAC and contralateral mammoplasty.
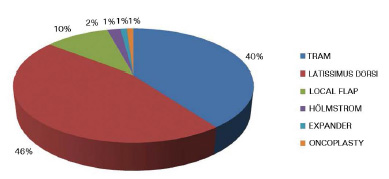
Figure 12. Techniques used in reconstruction.
The age of the patients varied between 24 and 88 years, with a mean age of 49.33. Among those who underwent reconstruction with the TRAM flap, the mean age was 48.55 years; with the LD flap, 48.93 years; and with the local flap and implant, 50.3 years.
One hundred ninety-seven patients underwent surgery on the right side and 169 on the left; 14 patients underwent bilateral reconstruction. Four cases underwent more than one type of technique because of failure of the first reconstruction with the same surgical team. Of note, in 4 of the reconstructed breasts, tumors were discovered on pathological examination of tissue removed in aesthetic mammoplasty, with no previous suggestive clinical or radiological signs. Ten other patients were referred from other services for reconstruction with autologous tissue after failure of reconstruction with skin expanders.
The time of follow-up of patients varied between 5 months and 7 years, and immediate reconstruction was implemented in 80% of patients (295 patients).
Moderate complications (5 cases) included dehiscence of part of the abdominal incision that needed resuturing (2 cases), skin necrosis at the mastectomy site that required a full-thickness skin graft on the TRAM flap (1 case), and abdominal bulging that required surgical correction with plication of the mesh screen and insertion of a new screen (2 cases) (Figure 13).
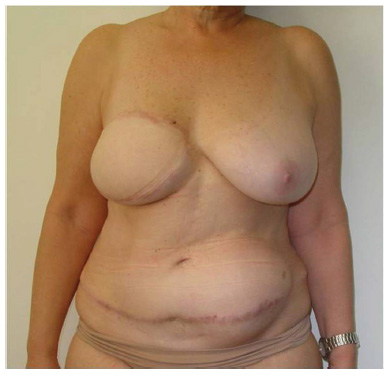
Figure 13. Abdominal bulging post-TRAM procedure.
Serious complications included total necrosis of the flap (2 TRAM cases and 1 LDM case) (Figure 14), total liponecrosis of the flap with preservation of the skin envelope (2 TRAM cases), extrusion of the implant after skin necrosis of a skin-sparing mastectomy followed by infection (11 LDM cases and 1 LM case), pulmonary thromboembolism (1 LM case), and deep venous thrombosis (1 case). There were no deaths.

Figure 14. Total necrosis of the TRAM flap in a smoking patient.
We observed 8 cases of capsular contracture around the implant; 3 of these patients underwent radiotherapy after immediate reconstruction while 5 did not.
There were minor complications, such as small dehiscence, seroma, or liponecrosis, which did not require secondary surgical procedures (Figure 15).
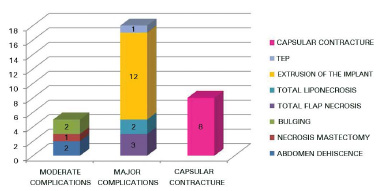
Figure 15. Complications.
Smoking was associated with massive liponecrosis of the TRAM flap in 2 patients, as well as loss of the implant in 7 patients submitted to the LDM flap. In these patients, the myocutaneous flap remained intact, but infection was introduced through skin necrosis of the skin-sparing mastectomy used in immediate reconstruction.
There were, in total, 13 patients who suffered skin necrosis at the mastectomy site: 11 who underwent reconstruction with the LDM flap and developed loss of the implant, 1 with an LM flap, and 1 who underwent reconstruction with a de-epidermized TRAM flap, which required a skin graft to promote healing and not delay the initiation of adjuvant therapy. With respect to the initiation of complementary therapy, delays occurred in 2 patients with delayed healing, one being a smoker and the other a patient with psoriasis.
The patient who had pulmonary thromboembolism had a previous history of deep venous thrombosis, and the precautions recommended by the angiology team were all implemented in the pre-, trans-, and post-operative periods. She progressed satisfactorily and without sequelae and, after 4 years, was submitted to balancing mammoplasty, without complications.
Complications in the donor area of the TRAM flap included abdominal bulging without hernia in 5 patients (1.7%), 2 of which required surgical correction, and seroma formation on the abdomen (4.6%), which required surgical treatment in 2 cases and was resolved with repeated punctures in 5 cases. Regarding the donor area of the LDM flap, 4% of patients developed seroma, treated with up to 2 punctures (7 cases). There was, however, seroma formation in the receiving area and axilla in 1.5% of cases and hematoma formation in the immediate postoperative period in the same region in 3 cases.
Among the 295 patients who underwent immediate reconstruction, 187 were submitted to radiotherapy in the postoperative period, 192 to chemotherapy, and 250 to hormone therapy.
Among the 75 patients who underwent late reconstruction, 57 had been previously submitted to chemotherapy and 49, radiotherapy. None had extensive radiodermatitis or ulceration of the skin at the time of the initial consultation. The interval between mastectomy and reconstruction ranged between 5 months and 12 years, with a mean of 3 years.
There was no contraindication for reconstruction in any of the patients presented for the initial assessment. In the cases of comorbidities, we chose to perform surgical techniques with lower morbidity.
DISCUSSION
Breast reconstruction has evolved significantly since its first reports, and currently we have an extensive arsenal of techniques that include new autologous tissue flaps and new techniques in the use of implants and extenders. Thus, the main objective-that initially was only to reconstruct the breast cone-reverted to reconstruction of the breast as naturally as possible and more similar to the contralateral breast5.
In addition, there has been a significant increase in the incidence of immediate breast reconstructions over the past 10 years, having grown from 20% to 31.8%, according to a report by Nelson et al.8. Although some reports associate this type of reconstruction with a higher incidence of complications and hospital readmission, Nelson et al., in a broad and general study, concluded that these disadvantages are only associated with obese patients and smokers.
Autologous breast reconstruction often provides a more favorable aesthetic outcome than other reconstruction options. The selection of the techniques to be used in reconstruction candidates in this series followed the criteria of the team, which are in agreement with published data3,4. The epidemiology of the sample showed very young patients already being affected by breast cancer1, encompassing economically active age groups, often without children, which necessitates special consideration regarding the desire of the patient to become pregnant after the end of treatment and the choice of the technique to be employed.
The methods of reconstruction used here are not free of complications, even though the incidence of severe complications is low. In this study, the incidence of flap necrosis is in accordance with that reported in the literature, although there is a wide variation in the values of each study (1%-24%)4,9,10.
Despite the advent of microsurgery, advances in surgeries of perforating vessels, and increased complexity of the procedures, the pedicled TRAM flap is still one of the most common methods of autologous reconstruction performed to date5.
Comparative studies between free and pedicled TRAM flaps found no significant differences in the function of the abdominal wall between the 2 groups11,12. Although some studies reported an objective advantage of deep inferior epigastric perforator (DIEP) flaps, this has not reflected in difficulties in performing activities of daily living11,13, as also found in our work. The abdominal bulging found did not prevent the patients from performing their daily professional or leisure activities; however, there was no patient in our study who performed intense physical activity prior to surgery.
The advantages of reconstruction with the TRAM flap include the achievement of breast volume in one surgical step, the creation of a soft and naturally ptosed breast, greater control over symmetry with the contralateral breast, and aesthetic benefits in the abdominal donor area4.
The main indication for reconstruction with a free TRAM flap-for which this flap is undeniably better than the pediculated flap-is patients with a higher risk of complications, such as obese patients and smokers, due to increased vascularization4,10,12. In this series, with these patients, we chose to use other surgical techniques, such as reconstruction with the LDM flap.
Reconstruction with the LDM flap and implant is an old and reliable technique, with a low rate of complications. In our study, the complications were restricted to 4 cases of seroma on the dorsum, resolved by puncture, and 4 cases of exposure with loss of the implant due to skin necrosis at the mastectomy site with resultant contamination and local infection. This rate of loss of the implant due to infection (6%) is similar to that found in the literature (7%-9%)10,14, while the rate of seroma is significantly lower. Branford et al.15 described a rate of up to 79% for seroma on the dorsum after implementation of the extended LDM flap without use of adhesion sutures; in addition, other more severe complications described in the same study, such as 30% for necrosis in the donor area and 1% for total necrosis of the flap, were not observed in our study. Miranda et al.16 reported a similar rate for seroma-approximately 72% with use of the conventional LDM flap.
We also observed an incidence of 20% for capsular contracture, with and without radiotherapy-a similar rate to that found in studies that assessed contracture after radiotherapy in immediate breast reconstruction14.
The analysis of complications between the groups shows a higher incidence of complications (small dehiscence and liponecrosis) in TRAM flaps than in LDM flaps, but when there was a complication with the LDM flap, however slight the dehiscence, there was loss of the implant, with evident aesthetic loss of reconstruction. There is a need, therefore, to evaluate the condition of the remaining skin at the end of the mastectomy and debride all the areas that have no reliable vascularization to minimize post-operatory necrosis14.
A major advantage of reconstruction with autologous tissue is that the deleterious effect of radiotherapy applied either before or after the reconstruction has less impact on the final aesthetic characteristics of the reconstructed breast14,17. In cases in which immediate breast reconstruction is indicated despite the certainty of adjuvant radiotherapy, the choice of reconstruction technique should be based on tissue characteristics and blood supply. Techniques involving reconstruction with autologous tissue should be given priority because they reflect higher vascularization and resistance to radiation18,19.
A disadvantage of the combination of reconstruction with autologous tissue and radiotherapy is the possibility of possible liponecrosis in the flap being mistaken for or masking tumor relapse, because definite diagnosis may not be possible with clinical examination. However, Matos et al.20 demonstrated unequivocal findings that characterize liponecrosis and facilitate the diagnosis with magnetic resonance imaging.
CONCLUSION
Breast reconstruction with autologous tissue provides the plastic surgeon with a consistent and reliable method of breast reconstruction, with very satisfactory aesthetic results and low morbidity in patients selected for this technique.
REFERENCES
1. Benson JR, Jatoi I, Keisch M. Esteva FJ, Makris A, Jordan VC. Early breast cancer. Lancet. 2009;373(9673):1463-79. PMID: 19394537 DOI: http://dx.doi.org/10.1016/S0140-6736(09)60316-0
2. Erić M, Mihić N, Krivokuća D. Breast reconstruction following mastectomy; patient's satisfaction. Acta Chir Belg. 2009;109(2):159-66.110
3. Tachi M, Yamada A. Choice of flaps for breast reconstruction. Int J Clin Oncol. 2005;10(5):289-97. DOI: http://dx.doi.org/10.1007/s10147-005-0527-4
4. Serletti JM. Breast reconstruction with the TRAM flap: pedicled and free. J Surg Oncol. 2006;94(6):532-7. DOI: http://dx.doi.org/10.1002/jso.20492
5. Hammond DC. Latissimus dorsi flap breast reconstruction. Clin Plast Surg. 2007;34(1):75-82. DOI: http://dx.doi.org/10.1016/j.cps.2006.11.008
6. Spear SL, ed. Surgery of the Breast Principles and Art. 2nd ed. Philadelphia: Lippincott Williams & Wilkins; 2006.
7. SBACV. Normas de orientação clínica para a prevenção, o diagnóstico e o tratamento da trombose venosa profunda. J Vasc Br 2005;4(Supl.3):S205-20.
8. Nelson JA, Fischer JP, Chung C, Wu LC, Serletti JM, Kovach SJ. Risk of readmission following immediate breast reconstruction: results from the 2011 American College of Surgeons National Surgical Quality Improvement Program data sets. Plast Reconstr Surg. 2014;134(2):193e-201e. DOI: http://dx.doi.org/10.1097/PRS.0000000000000319
9. Tribondeau P, Soffray F. Breast reconstruction with pedicled TRAM flap (a retrospective study of 115 consecutive cases). Ann Chir Plast Esthet. 2008;53(4):309-17. PMID: 17959299 DOI: http://dx.doi.org/10.1016/j.anplas.2007.05.009
10. Greco JA 3rd, Castaldo ET, Nanney LB, Wu YC, Donahue R, Wendel JJ, et al. Autologous breast reconstruction: the Vanderbilt experience (1998 to 2005) of independent predictors of displeasing outcomes. J Am Coll Surg. 2008;207(1):49-56. PMID: 18589361 DOI: http://dx.doi.org/10.1016/j.jamcollsurg.2007.12.052
11. Atisha D, Alderman AK. A systematic review of abdominal wall function following abdominal flaps for postmastectomy breast reconstruction. Ann Plast Surg. 2009:63(2):222-30. PMID: 19593108 DOI: http://dx.doi.org/10.1097/SAP.0b013e31818c4a9e
12. Andrades P, Fix RJ, Danilla S, Howell RE 3rd, Campbell WJ, De la Torre J, et al. Ischemic complications in pedicle, free, and muscle sparing transverse rectus abdominis myocutaneous flaps for breast reconstruction. Ann Plast Surg. 2008;60(5):562-7. PMID: 18434832 DOI: http://dx.doi.org/10.1097/SAP.0b013e31816fc372
13. Brockhurst AC, Alderman AK, Lowery JC, Davis JA, Wilkins EG. Survey assessment of physical function following postmastectomy breast reconstruction. Plast Reconstr Surg. 2008;121(4):1108-15. PMID: 18349627 DOI: http://dx.doi.org/10.1097/01.prs.0000302455.14889.d5
14. Michy T, Gimbergues P, Le Bouëdec G, Dauplat J. What surgical procedure for immediate breast reconstruction after preoperative radiotherapy and chemotherapy? J Chir (Paris). 2007;144(6):511-5.
15. Branford OA, Kelemen N, Hartmann CE, Holt R, Floyd D. Subfascial harvest of the extended latissimus dorsi myocutaneous flap in breast reconstruction: a comparative analysis of two techniques. Plast Reconstr Surg. 2013;132(4):737-48. PMID: 24076666 DOI: http://dx.doi.org/10.1097/PRS.0b013e31829fe4f
16. Miranda BH, Amin K, Chana JS. The drain game: back drains for latissimus dorsi breast reconstruction. J Plast Reconstr Aesthet Surg. 2014;67(2):226-30. DOI: http://dx.doi.org/10.1016/j.bjps.2013.10.010
17. Carlson GW, Page AL, Peters K, Ashinoff R, Schaefer T, Losken A. Effects of radiation therapy on pedicled transverse rectus abdominis myocutaneous flap breast reconstruction. Ann Plast Surg. 2008;60(5):568-72. PMID: 18434833 DOI: http://dx.doi.org/10.1097/SAP.0b013e31815b6ced
18. McKeown DJ, Hogg FJ, Brown IM, Walker MJ, Scott JR, Weiler-Mithoff EM. The timing of autologous latissimus dorsi breast reconstruction and effect of radiotherapy on outcome. J Plast Reconstr Aesthet Surg. 2009;62(4):488-93. PMID: 18262481 DOI: http://dx.doi.org/10.1016/j.bjps.2007.11.046
19. Munhoz AM, Duarte GG, Sacramento M, Cherotto A, Gemperli R, Pinotti M, et al. Reconstrução mamária pós-mastectomia com tecido autógeno: avaliação comparativa de resultados e complicações. Rev Bras Gincecol Obstet. 2002;13(2):60-6.
20. Matos AV, Canella Ede O, Koch HA, Boisson SP, Azevedo CL, Djahjah MC, et al. Fat necrosis in the breast after reconstruction with transverse rectus abdominis myocutaneous flap: MRI features. Eur J Radiol. 2012;81 Suppl 1:S97-8. DOI: http://dx.doi.org/10.1016/S0720-048X(12)70039-6
1. Universidade Federal de Juiz de Fora, Juiz de Fora, MG, Brazil
2. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
3. Clínica Prime, Juiz de Fora, MG, Brazil
Institution: Clínica Prime - Juiz de Fora, Juiz de Fora, MG, Brazil.
Corresponding author:
Larissa Silva Leitão Daroda
Rua Rei Alberto, 180 - Centro
Juiz de Fora, MG, Brazil Zip Code 36016-311
E-mail: larissaleitao1@ig.com.br
Article received September 02, 2014.
Article accepted May 28, 2015.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter