

Original Article - Year 2015 - Volume 30 -
Microsurgical reconstructions in pediatric patients: a series of 12 cases
Reconstruções microcirúrgicas em pacientes pediátricos: uma série de 12 casos
ABSTRACT
INTRODUCTION: Reconstructive plastic surgery is used to treat defects of different sizes and locations. The advent of microsurgery has enabled the single-stage reconstruction of complex and large defects with lower morbidity rates. Despite being one of the first microsurgery applications, large pediatric microsurgical reconstruction series have been published only recently.
METHOD: Between January 2007 and December 2014, 12 consecutive patients underwent microsurgical reconstruction upon the removal of head and neck tumors or complex trauma in the limbs of pediatric patients. The medical records were retrospectively reviewed for injury location and etiology, flap type, and complications.
RESULTS: A total of 13 flaps were created for microsurgical reconstruction, including reconstruction upon head and neck tumor removal in five, limb complex post-trauma reconstruction in seven, and a microsurgical revascularization in the arm of one child.
CONCLUSION: Microsurgical reconstruction in children is peculiar. Our initial experience and the studies published in the literature to date show that in this particular group of patients, it is possible to achieve rewarding results that render this type of reconstruction feasible and highly successful in this age range.
Keywords: Microsurgery; Surgical flaps; Reconstructive surgical procedures.
RESUMO
INTRODUÇÃO: A cirurgia plástica reparadora depara-se com defeitos dos mais variados portes e localizações. O advento da microcirurgia possibilitou a reconstrução de defeitos complexos e extensos em um único estágio e com menor morbidade. Apesar de ter sido uma das primeiras aplicações da microcirurgia, a reconstrução pediátrica microcirúrgica só teve grandes series publicadas recentemente.
MÉTODO: No período de janeiro de 2007 a dezembro de 2014 foram operados 12 pacientes consecutivos de reconstruções microcirúrgicas pós-ressecção de neoplasias em cabeça e pescoço e traumas complexos em membros de pacientes pediátricos. Os prontuários foram revisados retrospectivamente quanto à localização e etiologia das lesões, tipos de retalhos e complicações.
RESULTADOS: Foram realizados 13 retalhos para a reconstrução microcirúrgica em 11 pacientes e uma revascularização microcirúrgica do braço, sendo cinco (41,7%) casos reconstruções pósressecção de neoplasias de cabeça e pescoço e sete (58,3%) casos pós-trauma complexos de extremidades. A taxa de viabilidade no nosso estudo foi de 84,6% dos retalhos realizados.
CONCLUSÃO: A reconstrução microcirúrgica em crianças tem particularidades. Nossa experiência inicial e a literatura mostram resultados gratificantes neste grupo especifico de pacientes, o que torna este tipo de reconstrução nessa faixa etária factível e com uma alta taxa de sucesso.
Palavras-chave: Microcirurgia; Retalhos cirúrgicos; Procedimentos cirúrgicos reconstrutivos.
Reconstructive plastic surgery is used to treat defects of different sizes and locations. The advent of microsurgery unequivocally modified reconstructive plastic surgery. Microsurgical flaps offer many advantages: complex and large defects can be repaired in a single stage, reduced length of hospital stay, hospital cost, and morbidity rates; and the possibility of primary closure of the donor area. There are a variety of donor areas that can be chosen and planned with the aim of achieving better aesthetic and functional outcomes as well as low morbidity rates1-3.
The improvements in microsurgery techniques have increased the recommendation for the use of free flaps in the pediatric population. Despite the greater technical difficulty associated with the procedure, children are an ideal group for microsurgical reconstructions due to their good health, preserved anatomy, greater functional reserve, greater neuronal plasticity, satisfactory healing, and absence of significant comorbidities as well as risk factors for atherosclerotic disease. The usual microsurgery indications in this age group are post-trauma reconstruction, postoncologic resections, congenital malformations, and replantation2,4-7.
OBJECTIVE
To demonstrate the technical feasibility and outcomes of a series of microsurgical reconstructions in pediatric patients after head and neck tumor resection or limb trauma.
METHODS
A retrospective clinical study was conducted between January 2007 and December 2014 in a series of 12 consecutive cases of microsurgical reconstructions upon head and neck tumor resection and extensive soft tissue loss with post-traumatic noble structure exposure in the limbs of pediatric patients.
Inclusion criteria were age < 16 years and having undergone microsurgical flaps reconstruction. We studied the following parameters: sex, age, etiology, lesion location, repair procedure, complications, and current clinical status. Flap choice was based on study of the defect, quantity and quality of the tissues requested, and vessel compatibility. This study was approved by the Ethics Committee of the University Hospital Walter Cantídio under protocol no. 044.04.15.
RESULTS
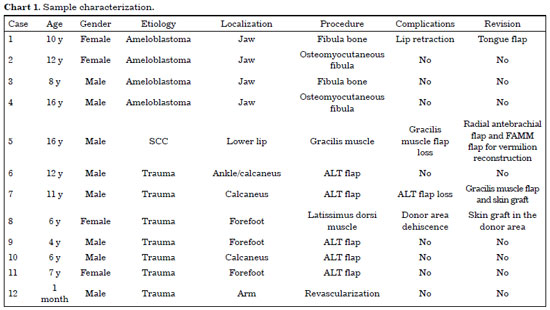
The sample included 12 patients, of whom eight were male (66.6%). The mean age was 9 years (range, 1 month to 16 years). In the study, ameloblastoma was the most prevalent tumor type (80%) observed in the reconstruction procedures carried out upon head and neck tumor removal. Among the cases of post-traumatic skin loss (58.3% of the sample), car accident was the leading cause of injuries (Chart 1).
Were carried out two microsurgical reconstructions with the fibula bone, two repairs with a fibula osteomyocutaneous free flap for jaw reconstruction, five anterolateral thigh (ALT) flaps for foot reconstructions, one latissimus dorsi muscle free flap, two gracilis muscle flaps, one radial antebrachial (Chinese), and one brachial artery revascularization in a 1-month-old infant.
Effective coverage of the large study defects was observed, showing good functional and aesthetic outcomes in all cases with minimal morbidity in the donor area. There was one case of total loss of the free ALT flap, which was reconstructed with a microsurgical myocutaneous flap of the gracilis muscle used for a calcaneus reconstruction and one case of free gracilis muscle flap total loss used for lip reconstruction. This led to a new reconstruction with a free radial antebrachial flap and facial artery musculomucosal (FAMM) flap for lip vermilion reconstruction. Regarding minor complications, a case of dehiscence of the donor area was observed and repaired with a skin graft.
All cases of head and neck reconstruction re-took a solid or pasty diet and intelligible speech. All patients who underwent limb reconstructions have resumed walking without the need for orthotics.
Thus, 13 flaps were created for microsurgical reconstruction in 11 patients, while a microsurgical revascularization was performed in the arm of one child. Our study's viability rate was 84.6%.
DISCUSSION
Microsurgical flaps are an option for the reconstruction of soft tissues in both the adult and pediatric population. The world literature shows that, despite the technical difficulties with anastomoses for small-diameter vessels, in the flap dissection and in the greater propensity to vasospasm, children are favorable candidates for this microsurgery. The pediatric population presents few risk factors that may lead to loose flaps, such as smoking and systemic diseases, in addition to free atherosclerosis vessels and a greater functional reserve, which allows the use of longer-duration anesthetic procedures and a rapid postoperative recovery. Harii and Ohmori were the first to describe a free flap transfer in children, a free inguinal flap. The list of free flaps at the disposal of the plastic surgeon continues to increase for muscle, fasciocutaneous, and bone. More recently, van Landuyt et. al. introduced the concept of free perforating flap in pediatric reconstructions4-8. Flap size and pedicle length are smaller in children than in adults, which requires planning and thorough measurements to ensure surgical success. The donor area morbidity as well as the functional and aesthetic results are important considerations in choosing the appropriate flap9,10.
Large head and neck tumors usually require free flap reconstruction. The jaw is the most common site for these tumors. Ameloblastoma, aneurysmal bone cyst, and fibromatosis are the most common benign lesions in this region. Ameloblastoma is one of the most common benign jaw tumors in adults; however, it may also occur in the pediatric population. This neoplasm, despite being a benign lesion, can expand aggressively, causing local destruction and possibly evolving into a malignant transformation in untreated cases. Thus, tumor removal is recommended, which causes large aesthetic and functional deformities. The use of non-vascularized bone grafts and local flaps is associated with higher complication rates, especially if associated with radiotherapy. The large resection and immediate reconstruction with vascularized tissues is the current gold standard for malignant jaw lesions, mainly for defects > 6 cm. The fibular flap is the gold standard for jaw reconstruction. However, it can also be very useful in the repair of extensive bone loss of the upper and lower limbs9-11. In this series, four jaw reconstructions were performed upon ameloblastoma removal. In both cases, the repair was performed using only vascularized fibula bone. In the other two, an osteomyocutaneous flap was used for bone floor of the mouth reconstruction (Figures 1 and 2).

Figure 1. Patients with jaw ameloblastoma who underwent central arch jaw reconstruction using a fibular osteomyocutaneous flap.

Figure 2. Patients with jaw ameloblastoma who underwent resection and reconstruction using a fibular osteomyocutaneous flap.
The ALT flap described by Song et al. is based on the descending branch of the lateral circumflex femoral artery. It is used mainly to reconstruct the head, neck, and limbs and presents the following advantages: large amount of skin available; long pedicle; possibility of several skin flaps with subcutaneous tissue, fascia, muscle, and bone; and a donor area presenting with low morbidity rates3,12,13. In the study, five foot reconstructions were performed (calcaneus and forefoot) with this free flap, while there was one case of total flap loss for venous thrombosis (Figure 3).

Figure 3. Skin loss in the dorsal region of the foot with bone and tendon exposure treated with reconstruction using an anterolateral thigh free flap.
The dominant pedicle of the free latissimus dorsi muscle flap contains the thoracodorsal artery. It can cover an extensive defect of the soft tissues in the head and neck, trunk, and upper and lower limbs and can be used with or without a skin island depending on the defect. It has a long pedicle and low morbidity in the donor area and it can be a closed primary flap that prevents aesthetic sequelae5,14. The microsurgical gracilis muscle flap is located in the medial region of the thigh and can be used as a muscle flap or skin muscle. Its dominant pedicle is the ascending branch of the medial femoral circumflex artery. This flap is used in reconstructions covering the head and neck and the upper and lower limbs as well as in facial paralysis. The radial antebrachial flap (Chinese flap) comprises an area of thin skin and is well vascularized in the anterior surface of the forearm. Its pedicle is based on the radial artery, and its venous system returns through the superficial and deep system of the forearm. It is used mainly in reconstructions of the head and neck as well as the upper and lower limbs. However, its disadvantage is the use of a skin graft for closing its donor area with a poor cosmetic outcome1-3. In the study sample, we conducted a free latissimus dorsi muscle flap for skin loss reconstruction with bone and tendon exposure in the forefoot, which was associated with skin graft in the muscle portion of the flap (Figure 4). A gracilis muscle flap for the reconstruction of the lower lip after squamous cell carcinoma resection resulted in total loss due to a venous thrombosis. A radial antebrachial recovery flap was created and associated with lip vermilion reconstruction with a FAMM flap (Figure 5). A muscular gracilis muscle flap was also performed for calcaneus reconstruction after total loss of the ALT flap (Figure 6).

Figure 4. Extensive skin loss with tendon and bone exposure on the dorsal surface of the forefoot treated with reconstruction using a latissimus dorsi muscle free flap and a skin graft.

Figure 5. Squamous cell carcinoma in the lower lip treated with resection and reconstruction using a radial antebrachial flap and vermilion reconstruction with a facial artery musculomucosal flap.

Figure 6. Skin loss with exposed bone in the calcaneus treated with reconstruction using a gracilis muscle free flap and a skin graft.
In several analyzed series, the success rate of free flaps in children was > 95%, a rate even higher than the average in the adult population. This average reported in the recent world literature was 89-97%3,4. In our series, the flap survival rate was 84.6% of the reconstructions performed, which was only slightly lower than the average described in the reviewed literature.
CONCLUSION
Microsurgical reconstruction in children is peculiar since these patients are less cooperative and their structures are more delicate. Although there is a higher incidence of vasospasm, pediatric patients are free of negative risk factors for vascular microsurgery such as smoking, atherosclerosis, and systemic diseases that are combined with a low morbidity of the donor area. Our initial experience and data published in the literature show the achievement of rewarding results in this particular group of patients, which renders this reconstruction type feasible, safe, reliable, and with a high success rate in this age group.
REFERENCES
1. Souza Filho MVP, Santos CC. Microcirurgia em reconstruções complexas: análise dos resultados e complicações. Rev Bras Cir Plást. 2009;24(2):123-30.
2. Wrublevski B, Groth AK, Ono MCC, Silva ABD. Retalhos microcirúrgicos na infância e na adolescência. Rev Bras Cir Plást. 2010;25(supl):1-102.
3. Torres ALG, Milcheski DA, Nakamoto HA, Tuma Júnior P, Ferreira MC. Aplicação da microcirurgia no reparo de lesões complexas. Rev Bras Cir Plást. 2009;24(2):131-7.
4. Pinder RM, Hart A, Winterton RI, Yates A, Kay SP. Free tissue transfers in the first 2 years of life-a successful cost effective and humane option. J Plast Reconstr Aesthet Surg. 2010;63(4):616-22. DOI: http://dx.doi.org/10.1016/j.bjps.2009.01.051
5. Konttila E, Koljonen V, Kauhanen S, Kallio P, Tukiainen E. Microvascular reconstruction in children-a report of 46 cases. J Trauma. 2010;68(3):548-52. DOI: http://dx.doi.org/10.1097/TA.0b013e3181a5f42c
6. Upton J, Guo L. Pediatric free tissue transfer: a 29-year experience with 433 transfers. Plast Reconstr Surg. 2008;121(5):1725-37. PMID: 18453997
7. Akçal A, Karşıdağ S, Sucu DÖ, Turgut G, Uğurlu K. Microsurgical reconstruction in pediatric patients: a series of 30 patients. Ulus Travma Acil Cerrahi Derg. 2013;19(5):411-6. DOI: http://dx.doi.org/10.5505/tjtes.2013.09515
8. Aboelatta YA, Aly HM. Free tissue transfer and replantation in pediatric patients: technical feasibility and outcome in a series of 28 patients. J Hand Microsurg. 2013;5(2):74-80. DOI: http://dx.doi.org/10.1007/s12593-013-0101-7
9. Sainsbury DC, Liu EH, Alvarez-Veronesi MC, Ho ES, Hopyan S, Zuker RM, et al. Long-term outcomes following lower extremity sarcoma resection and reconstruction with vascularized fibula flaps in children. Plast Reconstr Surg. 2014;134(4):808-20. DOI: http://dx.doi.org/10.1097/PRS.0000000000000555
10. Bilkay U, Tiftikcioglu YO, Temiz G, Ozek C, Akin Y. Free-tissue transfers for reconstruction of oromandibular area in children. Microsurgery. 2008;28(2):91-8. DOI: http://dx.doi.org/10.1002/micr.20457
11. Schwarz GS, Disa JJ, Mehrara BJ, Healey JH, Cordeiro PG. Reconstruction of oncologic tibial defects in children using vascularized fibula flaps. Plast Reconstr Surg. 2012;129(1):195-206. PMID: 22186510 DOI: http://dx.doi.org/10.1097/PRS.0b013e318230e463
12. Gharb BB, Salgado CJ, Moran SL, Rampazzo A, Mardini S, Gosain AK, et al. Free anterolateral thigh flap in pediatric patients. Ann Plast Surg. 2011;66(2):143-7. PMID: 21178758 DOI: http://dx.doi.org/10.1097/SAP.0b013e3181e35e38
13. Van Landuyt K, Hamdi M, Blondeel P, Tonnard P, Verpaele A, Monstrey S. Free perforator flaps in children. Plast Reconstr Surg. 2005;116(1):159-69. PMID: 15988263 DOI: http://dx.doi.org/10.1097/01.PRS.0000169697.06498.DF
14. Rinker B, Valerio IL, Stewart DH, Pu LL, Vasconez HC. Microvascular free flap reconstruction in pediatric lower extremity trauma: a 10-year review. Plast Reconstr Surg. 2005;115(6):1618-24. PMID: 15861066 DOI: http://dx.doi.org/10.1097/01.PRS.0000160698.68234.6C
1. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
2. Hospital Universitário Walter Cantídio da Universidade Federal do Ceará, Fortaleza, CE, Brazil
Institution: Universidade Federal do Ceará, Fortaleza, CE, Brazil.
Corresponding author:
Caio Alcobaça Marcondes
Rua Luiza Amélia Brandão, 916, São Cristóvão
Teresina, PI, Brazil Zip Code 64056-170
E-mail: caio_alcobaca@hotmail.com
Article received April 16, 2015.
Article accepted September 15, 2015.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter