

Case Report - Year 2015 - Volume 30 -
Reintegration of distal digital amputation with composite graft and plasmatic diffusion expanded distally on the palmar dermal plane - a case report of a 2-year-old child and a literature review
Reintegração de amputação digital distal com enxerto composto e difusão plasmática ampliada distal no plano dérmico palmar - relato de um caso em criança de 2 anos de idade e revisão da literatura
ABSTRACT
In more-distal amputations of the fingertips, microsurgical replantation is not feasible. For these cases, composite graft provides the best functional and aesthetic results. However, its reintegration is uncertain. Several techniques have been proposed to improve bulky graft survival by basically reducing its volume, regardless of whether a skin flap is connected. Other techniques create an additional contact surface for plasmatic diffusion, the so-called subcutaneous pocket, without reducing the composite graft volume and yielding high success rates. This article presents a case of amputation of the distal tip of the fifth digit (Ishikawa zone I) of a 2-year-old child. Because of the impossibility of microsurgical replantation, a composite graft was used to reintegrate the amputated stump, without debridement, by creating a new contact surface for plasmatic diffusion at the distal end of the grafted stump, on the dermal plane in the hypothenar region, thereby increasing the contact area and decreasing the radial distance for the plasmatic diffusion of the composite graft. Twelve days later, the additional contact was separated and both surfaces presented bleeding. Full reintegration occurred with minimal scarring of the finger and hypothenar region. A brief literature review was conducted, discussing surgical concepts and factors that influence composite graft survival. The most appropriate and best vascularized anatomic plane for additional contact with the graft in the recipient area needs to be determined.
Keywords: Amputation; Amputation stumps; Composite grafts; Child; Finger injuries.
RESUMO
Nas amputações mais distais da ponta dos dedos, o reimplante microcirúrgico pode não ser praticável. Nestes casos, o enxerto composto oferece os melhores resultados funcionais e estéticos, sendo, porém, incerta a sua reintegração. Várias técnicas foram aventadas para melhorar a sobrevida do enxerto volumoso, basicamente diminuindo o seu volume, associando ou não um retalho cutâneo. Outras técnicas criam uma superfície adicional de contato para difusão plasmática, o "bolso subcutâneo", sem diminuir o volume do enxerto composto, com altas taxas de sucesso. O presente artigo apresenta um caso de amputação da ponta distal do dedo mínimo (zona I de Ishikawa) numa criança de 2 anos de idade. Impossível de reimplante microcirúrgico, a reintegração foi feita com enxerto composto do coto amputado, sem desbridamento, e com a criação de uma nova superfície de contato para difusão plasmática, na extremidade distal do coto enxertado, no plano dérmico da região hipotênar, aumentando assim a área de contato e diminuindo a distância radial da difusão plasmática no enxerto composto. Doze dias após, esse contato adicional foi separado e ambas as superfícies apresentaram sangramento. A reintegração foi total, com mínimas cicatrizes no dedo e na região hipotênar. Uma breve revisão bibliográfica foi feita e discutidos os conceitos cirúrgicos, assim como os fatores que influenciam na sobrevida do enxerto composto. Na área receptora, o plano anatômico mais adequado e melhor vascularizado, para o contato adicional com o enxerto, necessita ser determinado.
Palavras-chave: Amputação; Cotos de amputação; Enxertos compostos; Criança; Traumatismos dos dedos.
The fingertip is a highly specialized tissue containing complex nerve endings plus the fingernail, which are both functional and aesthetically irreplaceable. Microvascular replantation is the gold standard for the treatment of amputations1. However, in very distal amputations (Tamai zone I, Ishikawa subzones I and II, Hirase zones I, IIA, and IIB, Fulcher zone III, and Allen types I, II, and III;2 Figure 1), microsurgical anastomosis can be extremely difficult or unfeasible, especially venous anastomosis1,2. Several treatment alternatives can be applied in these cases, such as wound healing by secondary intention, direct primary closure, skin grafting, local flaps, cross-finger flaps, distance flaps, and composite grafting3.
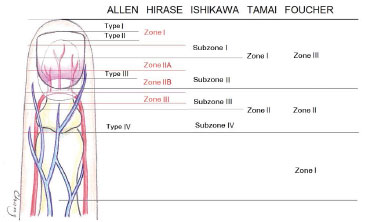
Figure 1. Level classifications of fingertip amputations.
Among these techniques, composite grafting seems to provide better functional and aesthetic results, as it restores the original tissue4. However, reintegration cannot be predicted, and the success rate is not high, particularly in adults. To increase the survival of the grafted stump and preserve the shape and function of the fingernail, several techniques have been published based on removal of fat from the stump5, bone resection, and connections with local flaps6, that is, decreasing graft volume for plasmatic diffusion. The cap technique decreases the proximal stump7. These techniques result in shortening, and often in nail atrophy and deformities. The Hirase technique cools the grafted stump at 4°C in the first 72 hours, without shortening it. The technique of decorticating the entire amputated stump, reintegrating it as a composite graft without reducing its volume, and "burying" the finger in an abdominal or palmar subcutaneous pocket to increase the contact area for plasma infusion seems to have high success rates without shortening the finger8-10.
This work presents a 2-year-old child who underwent amputation of half of the distal phalanx, Ishikawa zone I, which was treated using a composite graft by creating an area of dermal contact distally with the hypothenar region to increase the area of plasmatic diffusion (Figure 2) in order to evolve into a complete reintegration. In addition, a literature review is presented and discussed.
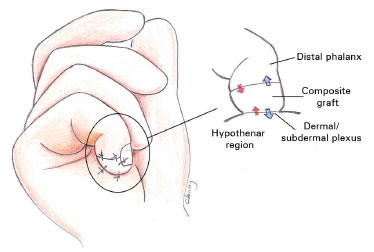
Figure 2. Reintegration of the amputated stump for composite grafting, without debridement, with the creation of an additional distal contact area in the dermal plane of the hypothenar region. This technique decreases the thickness of the composite graft in half and doubles the contact area for plasmatic diffusion.
CASE REPORT
W.M.M., a 1 year and 11 months-old male child, sustained complete amputation of the distal half of the distal phalanx on the right fifth digit by smashing it against the door of their home. A pediatrician immediately referred him to the author's office, where he was brought by his parents, along with the amputated distal stump wrapped in gauze, inside a dry plastic bag, which was inside a styrofoam box filled with ice. Examination revealed full amputation of the distal half of the distal phalanx, Ishikawa type I, with nail avulsion (Figure 3). A small bone fragment from the phalanx in the distal stump was found. Reattachment was indicated, with the possible attempt at composite grafting if microsurgical anastomosis was not feasible.
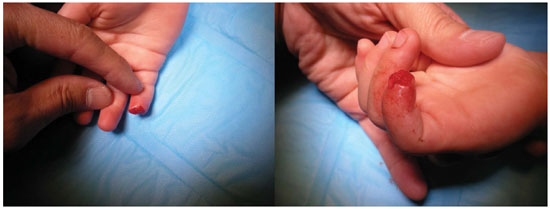
Figure 3. Guillotine-type amputation of half of the distal phalanx, with distal phalanx fracture and nail avulsion.
The time interval between amputation and the beginning of surgery was 6 hours. Under general anesthesia and with the use of a surgical microscope for magnification, the proximal and distal stumps were carefully cleaned and thoroughly examined. Given that no vessel candidates for anastomosis were found, composite grafting was the solution. However, as the amputated stump was bulky for grafting, the author chose not to "slim down" the graft (to prevent phalanx shortening) and proceeded to thoroughly suture the distal stump and nail bed, reinsert the avulsed nail for protection, and decorticate an area of approximately 5 × 5 mm from the distal end of the grafted stump and from a similar area in the hypothenar region. The two decorticated surfaces were joined and sutured as a second grafting area in order to increase the area of diffusion. The hand was immobilized in the physiological position with a plaster cast. After 72 hours, the dressing was removed and the graft presented with good coloring. The cast was removed to avoid compression injury, and an occlusive dressing was applied.
Twelve days after surgery, the graft was in good condition, and the fingertip was separate from the palm. Upon removal of the sutures and carefully rubbing the two surfaces, bleeding occurred (Figure 4). In the clinic, anesthetic ointment was applied 15 minutes prior to the procedure, and lidocaine was applied during the procedure. In subsequent dressings, the graft showed progressive improvement, with epithelium exchange and growth of the nail.
RESULTS
At 199 days after the surgery, the growth of the nail was normal, without any deformity. The entire epidermis renewed spontaneously, without sequelae in the decorticated area. The scar was barely noticeable (Figure 5). No marked difference in size or length was observed as compared with that of the contralateral finger. Discriminating sensitivity was not tested because the patient was a 2-year-old child. Nonetheless, the child had no complaints of pain and intolerance to cold. The mother reported that the child was able to perform all activities normally and make use of the hand and finger without any restriction.
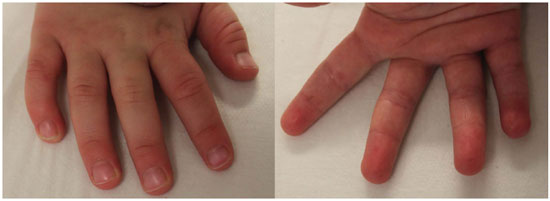
Figure 5. Result 199 days after surgery. Note that the fifth-digit nail and digital pulp present no deformities or sequelae.
DISCUSSION
Graft survival or reintegration depends, in the first phase, on plasmatic diffusion and, subsequently, on rechanneling and neovascularization. Increasing and improving the distribution in the contact area between the graft and the recipient seems to make perfect sense conceptually and can result in a bulkier graft. Decorticating the graft and suturing it within a subcutaneous pocket on the contralateral chest wall was first described by Brent7 in 1979. Arata et al.8 replaced the thoracic subcutaneous pocket with an ipsilateral palmaris, which is more convenient for patients, mainly for children6. The article reports full reintegration in 81% of the patients treated and 19% of patients with a small area of necrosis around the tip, of whom two patients required removal of the exposed bone and in one patient there was spontaneous healing of the exposed bone but with no total loss.
If compared to the microsurgical replantation success rate, which is 86% in the statistics reported by Yamano, this composite grafting technique reached quite close levels. However, when comparing it to a series of conventional composite grafts and minimum debridement in children, Moiemen and Elliot10 obtained full reintegration in 22% of their patients, partial reintegration in 52%, and total necrosis in 26%. Lin et al.9 replaced the subcutaneous pocket with the subdermal pocket in the contralateral abdomen. The authors believe that the contact of the subdermal planes in the two extremities would connect better than the subcutaneous or fascial planes, in addition to the easier monitoring of the holding strength of the graft.
Nonetheless, the reintegration of the fingertip with composite grafting does not depend solely on the contact area for diffusion and revascularization. Heinstein and Cook4 prospectively analyzed the factors affecting graft survival in 57 amputations treated with grafting and concluded that smoking is the strongest independent cause of graft loss. Diabetes and blunt trauma have secondary negative influence only. Moiemen and Elliot10 added yet another determining factor, which is the time between amputation and grafting. Grafts made within 5 hours of the amputation have a high success rate, and the authors found no difference in prognosis between children and adults. In relation to sensitivity recovery, Arata et al.8 did not observe any differences between cases where the nerves were repaired and those where they were not. Nishi et al.11 researched on nail regeneration after fingertip replantation and concluded that this depends on the degree of amputation, whether or not the germinal and sterile matrix is injured, and the circulatory conditions after the replantation.
In this case, the trauma was blunt and the amputated stump was subjected to cooling with direct contact with the ice. The degree of the amputation was in Ishikawa zone I, and the ischemia time was 6 to 7 hours. The author was uncertain about the graft volume and reluctant to shorten the finger. Thus, the author decided to create a contact area at the distal end of the grafted stump on the ipsilateral hypothenar region by leaving the graft with proximal and distal areas of diffusion to increase the total area and radially decrease, perhaps in half, the plasmatic diffusion distance of the graft.
The dermal plane was opted for both sides, as it is more vascularized than the subcutaneous plane, and the graft was not buried as in the pocket technique described by Brent7 and modified by Arata et al.8 and Lin et al.9. The relatively short time between the amputation and the grafting, the fracture of half of the distal phalanx (zone I), and the correct management of the amputated stump before reaching the hospital indisputably contributed to the success of the graft. In fact, 12 days after the surgery, the graft integrated its distal side to the hypothenar skin and both surfaces showed bleeding at the time the finger was separated from the palm. To a greater or lesser degree, the creation of a distal dermal contact area may have contributed to the security and full reintegration of the composite graft.
CONCLUSION
When a microvascular replantation is not feasible, composite grafting by restoring the original tissue can provide the best functional and aesthetic results for the most distal amputation of the fingertip4. According to the literature review, the main factors that influence graft survival are smoking, which has a strong negative impact4, and the time interval between amputation and grafting, in which prognosis within 5 hours is better. Age, type of trauma, and diabetes mellitus are secondary factors10. The germinal and sterile matrix must be thoroughly repaired to prevent or reduce nail deformities. The concept of increasing the contact area of the bulky graft with the recipient and reducing the radial distance for plasmatic diffusion into a bulky graft, that is, creating another contact surface with the vascularized tissue at the distal end of the graft, appears to increase the survival and full reintegration of the graft, according to the works of Brent7, Arata et al.8, and Lin et al.9. The most vascularized and adequate anatomic plane of the graft recipient area has yet to be studied.
REFERENCES
1. Chang CY, Nassif T. Reimplante e revascularização da ponta do dedo: revisão de literatura e relato de caso de amputação da ponta de dedo mínimo na criança de um ano de idade. Rev Bras Cir Plást. 2011;26(4):714-7. DOI: http://dx.doi.org/10.1590/S1983-51752011000400032
2. Sebastian SJ, Chung KC. A systematic review of the outcomes of replantation of distal digital amputation. Plast Reconstr Surg. 2011;128(3):723-37. DOI: http://dx.doi.org/10.1097/PRS.0b013e318221dc83
3. Russel RC. Fingertip injuries. In: McCarthy JG, ed. Plastic Surgery. Philadelphia: Saunders; 1990. p.4477-98.
4. Heistein JB, Cook PA. Factors affecting composite graft survival in digital tip amputations. Ann Plast Surg. 2003;50(3):299-303. PMID: 12800909 DOI: http://dx.doi.org/10.1097/01.SAP.0000037260.89312.BF
5. Uysal A, Kankaya Y, Ulusoy MG, Sungur N, Karalezli N, Kayran O, et al. An alternative technique for microsurgically unreplantable fingertip amputations. Ann Plast Surg. 2006;57(5):545-51. PMID: 17060737 DOI: http://dx.doi.org/10.1097/01.sap.0000226944.08332.41
6. Dubert T, Houimli S, Valenti P, Dinh A. Very distal finger amputations: replantation or "reposition-flap" repair? J Hand Surg Br. 1997;22(3):353-8.
7. Brent B. Replantation of amputated distal phalangeal parts of fingers without vascular anastomoses, using subcutaneous pockets. Plast Reconstr Surg. 1979;63(1):1-8. PMID: 432310 DOI: http://dx.doi.org/10.1097/00006534-197901000-00001
8. Arata J, Ishikawa K, Soeda H, Sawabe K, Kokoroishi R, Togo T. The palmar pocket method: an adjunct to the management of zone I and II fingertip amputations. J Hand Surg Am. 2001;26(5):945-50. DOI: http://dx.doi.org/10.1053/jhsu.2001.27763
9. Lin TS, Jeng SF, Chiang YC. Fingertip replantation using the subdermal pocket procedure. Plast Reconstr Surg. 2004;113(1):247-53. PMID: 14707643 DOI: http://dx.doi.org/10.1097/01.PRS.0000095950.31223.09
10. Moiemen NS, Elliot D. Composite graft replacement of digital tips. 2. A study in children. J Hand Surg Br. 1997;22(3):346-52.
11. Nishi G, Shibata Y, Tago K, Kubota M, Suzuki M. Nail regeneration in digits replanted after amputation through the distal phalanx. J Hand Surg Am. 1996;21(2):229-33. DOI: http://dx.doi.org/10.1016/S0363-5023(96)80105-5
1. Sociedade Brasileira de Cirurgia Plástica, Rio de Janeiro, RJ, Brazil
2. Hospital dos Servidores do Estado do Rio de Janeiro, Rio de Janeiro, RJ, Brazil
3. Sociedade Brasileira de Microcirurgia Reconstrutiva, Rio de Janeiro, RJ, Brazil
Institution: Clínica Chang Yung Chia, Rio de Janeiro, RJ, Brazil.
Corresponding author:
Chang Yung Chia
Rua Carlos Oswald, 140, Bloco I, Apto. 206
Rio de Janeiro, RJ, Brazil Zip Code 22793-120
E-mail: changplastica@gmail.com
Article received: April 13, 2012.
Article accepted: July 23, 2012.



 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter