

Articles - Year 2004 - Volume 19 -
Plastic Surgery after Gastroplasty: Surgery Planning and Techniques
Cirurgia Plástica após a Gastroplastia Redutora: Planejamento das Cirurgias e Técnicas
ABSTRACT
Plastic Surgery aims to remove the subcutaneous panniculus subsequent to the major weight loss that follows gastroplasty, which makes it a hygiene surgery in some cases. Surgery planning and order should befollowed according to medical indication and patients' complaints. Abdominoplasty is the most frequent procedure. The surgery varies technically according to type of previous scar presence of hernias or skin excesso Mastopexy with or without silicone prosthesis, crural, thoracobrachial and cervicofacial liftings are also necessary. Some strategies should be used in former obese patients in order to optimize the final result. These surgeries aim to remove the remaining stigma of obesity, allowing the patient to attain a better quality of life.
Keywords: Gastroplasty; abdominoplasty; lift; skin excesso
RESUMO
A cirurgia plástica tem como objetivo retirar o panículo dermogorduroso decorrente da grande perda de peso que ocorre após a gastroplastia redutora, tornando-se em alguns casos uma cirurgia higiênica. A planificação e a ordem das cirurgias devem ser seguidas conforme a indicação médica e a queixa do paciente. O procedimento mais realizado é a abdominoplastia. Esta cirurgia apresenta variações na técnica conforme o tipo de cicatriz anterior, a presença de hérnias e excesso de pele. Também são necessárias mastopexias com ou sem inclusão de prótese de silicone, lifting crural, toracobraquial e cervicofacial. Nos pacientes ex-obesos, algumas táticas devem ser empregadas para otimizar o resultado final. Estas cirurgias têm como objetivo retirar o último estigma da obesidade, permitindo ao paciente uma melhor qualidade de vida.
Palavras-chave: Gastroplastia redutora; abdominoplastia; lift; excesso de pele
Obesity has reached epidemic levels, and gastroplasty is the most recent and powerful weapon used for the treatment of morbid obesity. The Center for the Obese of the State of Ceará (Núcleo do Obeso do Ceará) is comprised by twenty-two professionals, three of whom are plastic surgeons, and was founded in 1996. Since then, more than two-hundred and eighty gastroplasties and forty-five plastic surgeries have been performed. The Capella surgery is the preferred indication of the Brazilian Society of Bariatric Surgery, since it delivers better results. It is a vertical gastroplasty with a band (a small vertical pouch of approximately 50 ml), circled by a Sylastic ring, that works as a valve, sphincter or hourglass, associated with a Roux Y gastrojejunal bypass. It results in a weight loss of approximately 45% in relation to the initial weight of the obese individual in a year. Other technigues with the same objective are performed, including video laparoscopic surgeries (Gastroenteroanastomosis), the inflatable gastric band surgery and the intragastric balloon, inserted endoscopically (and removed after roughly 6 months). The surgery is indicated for patients with a body mass index (weight/height2) above 40 kg/m2. Inclusion and exclusion criteria are assessed by the general surgeon who will perform the procedure. Pre and postoperative multidisciplinary assessment (surgeons, dieticians, endocrinologists, cardiologists, physical therapists, psychologists, etc.) is essential.
Patients' weight loss results in substantial skin excess one year after gastroplasty. The assessment of the plastic surgeon and the correct planning of surgical stages, bearing in mind patients' complaints, are essential for the final result and in order to minimize complications. The most commonly affected region and main patient complaint is the abdomen (70% of cases), followed by breasts and thighs and then back, arms, buttocks and face. Usually three to four surgical interventions are necessary, with an ideal average interval of six months, although cases vary according to the clinical status ofthe patient and previous surgical complications. The present study aims to presem a routine for enhanced surgery follow-up, in order to minimize the number of complications. These patients are more prone to complications mainly due to the extension of detached flaps and compromised nutritional status, such as iron-deficiency anemia and hypovitaminosis or other conditions inherent to the obese patient.
METHODS
The authors performed a retrospective study of 26 patients submitted to 45 operations from November 1999 to January 2003 (Tables I and II). The mean age was 36 years. Seventy-five per cent of cases were female patients. The highest volume removed of abdominal skin flap and fat was 10 kg and the lowest 1.2 kg. Regarding the number of operations, 20 abdominoplasties, 9 mammoplasties, two of which were with placement of 200 cc texturized silicone prostheses, 2 gynecomasties, 3 crural lifts, 3 brachial lifts, 2 cervicofacial lifts and 4 liposuctions were performed. It was necessary to re-suture small areas of flap end necroses and dehiscence in four patients. One patient was re-operated on in order to remove a post-seroma abdominal pouch. The most frequent abdominal complications were seroma (30% of cases), hematomas (10%), necrosis (4%) and steatonecrosis in two patients (7%).

We recommend serum iron, total proteins and albumin as a preoperative routine, in addition to all tests. The general practitioner and general surgeon always make a prior assessment, and may ask for additional tests such as an abdominal ultra-sound, and rule out the possibility of incisional hernias. Local hygiene is essential to avoid contact dermatitis or infections, mainly in inner thighs and abdominal apron fold.
The site of the gastroplasty scar, whether a longitudinal supra-umbilical or a transversal bicostal scar, should be observed during the assessment of the abdomen. We prefer to correct the scar during a second surgical time, when the patient is submitted to another operation, to avoid it to join the abdominoplasty scar. Whether to remove it or not depends on the guality of the scar and the patient's wishes. Resection may be subdermal or total, to remove the whole subcutaneous panniculus. Patients may presem with two or three aprons, called abdominal and suprapubic aprons. The third apron, found in one patient, was due to an incisional hernia (Fig. 1). We do not believe that wearing an abdominal strap in the preoperative period to tighten the abdomen is necessary, unless there are large abdominal hernias that may lead to respiratory restriction after correction.
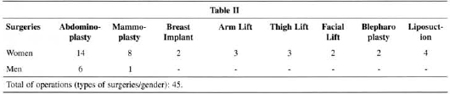
Figs. 1A-C - Type of abdominal apron in former obese patient.
General anesthesia is indicated in patients above 100 kg or with conditions contraindicating another option. Some patients however can receive epidural anesthesia with bupivacaine or ropivacaine. The decision depends on the anesthetist and all the information given by the patient during the pre-anesthetic visit. Surgical marking is similar to that of traditional techniques, with an excess in side lengths due to the large skin excess at flanks. We avoid large, normaliy inverted "V", detachments only to allow for the rectoabdominal muscle plicature (Fig. 2). In patients with large aprons or with a condition contraindicating a long surgical time, only hygiene surgery can be performed, that is to say without detachments or plicature (Fig. 3). Surgical correction of hernias should be performed along with the abdominoplasty and, in some cases, the presence of a general surgeon may be necessary (Fig. 4). The incision for transposition of the umbilicus should be performed by the surgeon's preferred technique, pointing out that the pedicle is long and one should be attentive to the plicature at the aponeurosis. Excess of plicatures make it difficult to position the umbilicus because of tension, widen the scar and leave an ungraceful aspect. After resection of the flaps, planes are sutured. Plicature and correction of the hernia is done with double 0 nylon. Fixation of the umbilicus is done with 3-0 Mononylon, and the subdermal and intra-dermal sutures with 70 cm 4-0 Monocryl. The abdomen is drained through a closed suction system, for an average of 5 days, that is, when we have 20 to 30 ml af daily drainage we remove the drain. In three of our cases, in addition to the suction drain, we put two Penrose n.1 drains at the ends of the scar, because the major lateral detachment and gravity do not aliow suction in this region. This capillarity drain was removed 48 hours postoperative. Dressing was performed with an abdominal strap for two months.
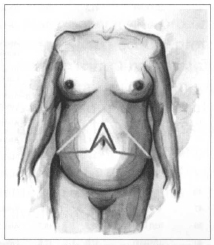
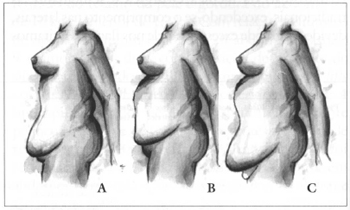
Fig. 2 - Levels of abdominoplasty detachment in former obese patient.
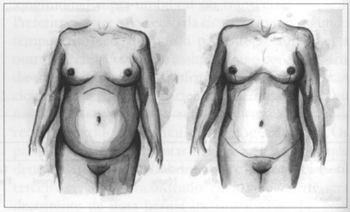
Fig. 3 - Reverse abdomen + abdominoplasty with minimal detachment.

Fig. 4 - Patient with large incisional hernia; 10 kg flap was removed. Two months postoperative period.
In comparison to other surgeries, mammoplasty in women is performed using the surgeon's preferred technique and in some cases silicone prostheses may be used for better breast projection. In men, skin resections are continued to the posterior axillary line, with care to preserve the areolomamillary complex. The surgery can be performed along with a brachial lift, and is called thoracobrachial lift. In thigh, back, arm and hip lifts the scar should be placed in barely visible sites or at natural folds. Detachments should be superficial and avoid lymphatic vessels, which can lead to prolonged edema when injured. We use subdermal and intradermal 70 cm 4-0 Monocryl sutures. In cervicofacial lifts, the approach should be the lower third of the face and neck, utilizing the SMAS plicature. Inpatient stay of these patients should not exceed two days. Prophylactic antibiotics are indicated according to the determination of the Hospital Infection Committee: Ist dose half-hour before skin incision, and every 3 hours of surgery duration and every 8 hours in the postoperative, without exceeding 24 h (2 g kefazol).
DISCUSSION
The classification of human shapes in terms of somatotypes: mesomorphic, ectomorphic and endomorphic(1), will determine the most affected regions after weight loss. In endomorphic individuals that have excess of fat in the abdomen and short limbs, skin excess is restricted mainly to the abdomen and lower limbs. Mesomorphic and ectomorphic individuals also have skin flaccidity in the upper segment after weight loss, in which arms, face and trunk are more affected.
There is a naturally high degree of variability within the three types. Regarding the abdomen, Lewis(2,3,4,5) describes three different kinds of skin flaccidity: pendular, globose, and flaccid. The pendular abdomen has a fat accumulation in the lower abdomen and around the navel, and, as the person loses weight, it folds over the pubis, in an apron-like form, due to excess weight (Fig. 1A). A globose abdomen is rounded, with generalized distension and a variable amount of fat, with or without flaccidity of the musculoaponeurotic system, with more than one apron after weight loss (Fig. 1B). A flaccid abdomen has redundant and thin skin, often has striae, and major flaccidity in the flanks and epigastric region (Fig. 1C), thus enabling anchor-shaped or reverse abdominoplasty.
Pitanguy(6,7) divides abdominal deformities into aesthetic and functional alterations. Aesthetic defects are chiefly due to flaccidity of the abdominal wall, with fat accumulation and a weak musculoaponeurotic system. Functionally, we analyze in the abdominal wall marked diastases, eventrations, natural hernias (umbilical, supra-umbilical), and incisional hernias.
Abdominoplasties in formerly obese people also present a hygienic aspect due to the existence of dermatitides and intertrigos resulting from the large excess of skin on natural folds. Suture dehiscences may be more freguent during the first phases of the healing process (from the 1st to 21st postoperative day), as a result of hematomas, infections, failure in the production of collagen tissue and, increased intracavity pressure; they also cause ruptures in the incisionalline and may lead to an incisional hernia. These dehiscences may also start later, even after the first postoperative month, due to the same reasons, and, more freguently, due to reduced scar resistance resulting from a sudden and sharp increase in intracavity pressure (undue effort in the postoperative period). Other sequelae, like scars of inappropriate positioning of incisions or after infections, make the abdomen look unpleasant and unaesthetic (7).
Formerly obese patients reguire greater care, not only due to local and clinical features, but also due to their psychological implications. They are tired of many previous treatments, personal, family and social traumas, which makes them more labile and rebellious in the postoperative. The postoperative of gastroplasty is different from other plastic surgeries that reguire greater and longer rest. The possibility of seroma(8), which may occur in up to 30% of cases, requires surgeons to be more vehement in their recommendations.
In the pubic hair region, because it is a region where there is greater occurrence of dehiscences and necroses, we prefer to use separate sutures, which also enable draining collections. We have decided to remove drains late when there is dark bloody discharge, which indicates the presence of clots and hematomas. We agree with Nurkin and Pedro Martins(9), that suction drains are effective to prevent hematomas and seromas through prolonged active drainage. Keeping the postoperative drain for more than eight days is toa long, though, and may increase the risk of infection and cause discomfort to patients. We believe that a maximum of seven days or serous drainage below 30 ml/ 24h are appropriate criteria for deciding to remove suction drains. Local postoperative care should be mainly a dressing, which, due to the extension and position of scars (normally large and in places with difficult access), favor inadequate asepsis (10). The clinical picture of these patients, normally with hypovitaminosis and iron deficiency anemia, leads to poor healing, with greater risk of infection and necrosis in flaps.
For these reasons, we prefer more conservative surgeries, with less flap detachment, avoiding the union of scars as much as possible (Fig. 5), like in the case of the anchor technique in the abdomen. In some thin patients, only the skin may be removed from the regions affected (with subdermal detachment) , and mainly in the abdomen, associating deep liposuction, if necessary (11,12). For other patients, with flaccidity limited to the region of the pubis, alternative techniques may be useful (13). We believe that the use of continuous intradermal suture with Monocryl 4-0 facilitates dressing with the maintenance of micropores over the suture, thus reducing dermatitides and granulo mas resulting frorn knots in the separate sutures, both externally and internally. Finally, not having to remove sutures is more easily accepted by patients, in addition to making the life of surgeons easier. In the late postoperative period, as Monocryl is absorbed within approximately three months, we avoid removing foreign body granulomas, common in nylon sutures.

Fig. 5 - Flap of 120 em and 7.1 kg. Photo of immediate PO.
As to results, we believe patients are more satisfied than surgeons. Their relief with the removal of excess skin is greater than the problems with the resulting scars. Men, in our experience, settle more easily and are happy with just the abdominal dermolipectomy.Women want a more comprehensive treatment, undergo more surgeries, and want treatment for the entire body contour (circumferential body lifting)(l5, 16, 17,18) (Fig. 6). Due to the greater number of complications, we do not perform combined surgeries in these patients, especially in the first phase, chiefly due to postoperative anemia. We give patients recommendations in relation to vitamin and iron supplementation. The average interval between surgeries is six months, a period which may be shortened depending on the clinical status of the patient and type of surgery. Some surgeries require a second postoperative time, especially those in the abdomen, with scar revision, ear resections, and liposuction.
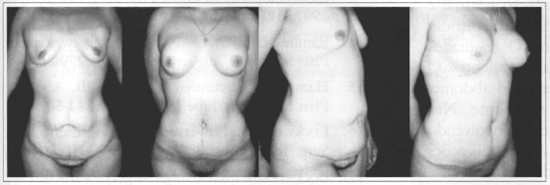
Fig. 6 - Patient who underwent five surgeries: breast implant, abdominoplasty, arm lifting, thigh lifting, and liposuetion.
CONCLUSION
Plastic surgery in formerly obese patients who underwent gastroplasty provides better quality of life, facilitating hygiene and movement, reinforcing self-esteem, restoring self-image, personal satisfaction, and reintegrating these people into society, which both patients and their families desired. Results are satisfactory, especially for patients. The most important thing is to treat the abdomen, which is often enough in men. Women demand a more comprehensive treatment, including the face and the entire body contour. Complications are greater than the average, but are local and correctible.
REFERENCES
1. Sheldon WH. The variety of human physique. New York: Hafner; 1963.
2. Lewis Jr. Atlas of Aesthetic Plast Surg. Boston: Little, Brown; 1973.
3. Lewis Jr. Miniabdominoplasty. Aesthetic Plast Surg. 1979; 3:195-9.
4. Lewis Jr, The Art of Aesthetic Plastic Surgery. Boston: Little, Brown; 1989.
5. Theimourian B, Marofat S. Cirugía del contorno de la parte media del tronco. In: Coiffman F, Cirugía Plástica Reconstructiva Estética. Barcelona: Masson-Salvat; 1994. rv p. 3117.
6. Pitanguy I, et al. Evaluation of body contouring surgery today: a 30-year perspective. Plast Reconstr Surg. Apr 2000; 105(4):1499-514.
7. Jaimovich CA, Mazzarone F, Parra JFN, Pitanguy L Semiologia da parede abdominal: seu valor no planejamento das abdominoplastias. Rev Soe Bras Cir Plást. 1999; 14(3):21-50.
8. Baroudi R, Ferreira CAA. Seroma: how to avoid it and how to treat it Aesthetic Plast Surg. November/December 1998; 18(6):439-41.
9. Nurkim MV, Martins p, et al. Incidência de hematoma e seroma em abdominoplastia com e sem uso de drenos. Rev Soc Bras Cir Plást. 2002; 17(1):69-74.
10. Matarasso A. Awareness and avoidance of abdominoplasty complications. Aesthetic Plast Surg. 1997; 17(4):256-61.
11. Avelar J. Abdominoplasty withour panniculus underming and resection: Analysis and 3-year follow- up of 97 consecutive cases. Aesthetic Plast Surg. 2002; 22(1)76-87.
12. Saldanha OR, Souza P, Bolivar E, et al. Lipoabdominoplasty without undermining. Aesthetic Plast Surg. November/December 2001; 21(6):518-26.
13. Moufarrège R. The Moufarrège horseshoe abdominoplasty. Aesthetic Plast Surg. March/April 1997; 17(2):91-6.
14. Ramirez, Oscar M. U-M Abdominoplasty. Aesthetic Plast Surg. July/August 1999; 19(4):279- 86.
15. Hamra ST. Circumferential body lift. Aesthetic Plast Surg. May/June 1999; 19(3):244-50.
16. Lockwood T. Lower-body lift. Aesthetic Plast Surg. July/August 2001; 21(4):355-70.
17. Lockwood T. Medial thigh surgery. Aesthetic Plast Surg. Summer 1996; 16(2):94-6.
I - Senior Member of the Brazilian Society of Plastic Surgery (SBCP), Physician of the Plastic Surgery Service of the Santa Casa de Misericórdia de Fortaleza and Instituto Dr. José Frota - IJF
II - Member of the Brazilian Society of Plastic Surgery and Instructor of the Plastic Surgery Service of Hospital Geral de Fortaleza.
III - Senior Member of the SBCP, President of SBCP - CE, President of the Brazilian Burns Society and Plastic Surgeon of the Burns Service of Instituto Dr. José Frota. Head of the plastic surgery residency program of IJF and HGF.
Núcleo do Obeso do Ceará (Center for the Obese of the State of Ceará)
Address for correspondence:
Edmar Maciel Lima Júnior, MD
Av. Sen. Virgílio Távora, 1901 sala 1103
60170- 251 - Fortaleza - CE Brazil
Phones: (55 85) 261-2028/261-9082
e-mail: edmarmacielsbcp@secrel.com.br


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter