

Original Article - Year 2015 - Volume 30 -
Use of a double-layer polypropylene mesh in the donor area of a TRAM flap for breast reconstruction: evaluation of the incidence of hernia and abdominal bulging
Uso de duas telas de polipropileno na área doadora do TRAM para reconstrução mamária: avaliação na incidência de hérnia e abaulamento abdominal
ABSTRACT
INTRODUCTION: The transverse rectus abdominis myocutaneous flap is a well stablished surgery for breast reconstruction. Its main disadvantage is a large defect in its donor site, leading to weakness in the abdominal wall. Many surgical tactics has been described to address the donor site defect, including direct closure of the muscular aponeurotic and use of polypropylene mesh. The purpose of this study was to assess abdominal hernia and bulge after TRAM flap breast reconstruction using two layers of polypropylene mesh in the donor site defect.
METHODS: Prospective study in 24 patients who had unilateral TRAM flap breast reconstruction with two layers of polypropylene mesh to close the donor site defect. The patients were evaluated in 3.6 and 12 months of postoperative time for incidence of abdominal hernia and bulge.
RESULTS: It was observed one case of abdominal bulge (4.16%) and no case of abdominal hernia. There were no cases of mesh infection or extrusion.
CONCLUSION: The use of two layers of polypropylene mesh in the donor site defect of TRAM flap breast reconstruction resulted in low incidence of abdominal hernia and bulge.
Keywords: Mammaplasty; Hernia, abdominal; Surgical flaps; Myocutaneous flap; Polypropylenes.
RESUMO
INTRODUÇÃO: O retalho transverso do músculo reto abdominal (TRAM) é um método bem estabelecido para reconstrução mamária. Apresenta como principal desvantagem o grande defeito da área doadora, podendo causar fraqueza da parede abdominal, hérnias e abaulamentos. Diversas táticas de fechamento do defeito da área doadora foram descritas, incluindo fechamento direto da aponeurose do músculo reto abdominal e uso de telas de polipropileno. O objetivo deste estudo foi avaliar os índices de abaulamento e hérnia no pós-operatório de TRAM utilizando a tática cirúrgica de fechamento da área doadora com duas telas de polipropileno.
MÉTODOS: Estudo prospectivo em 24 pacientes submetidos à reconstrução mamária unilateral com TRAM monopediculado ou bipediculado e reparo da área doadora com duas telas de polipropileno. Os pacientes foram avaliados quanto à incidência de hérnia e abaulamento no pós-operatório de 3, 6 e 12 meses.
RESULTADOS: Ocorreu um caso (4,16%) de abaulamento abdominal e nenhum caso de hérnia. Não houve casos de infecção ou extrusão da tela.
CONCLUSÃO: O uso de duas telas de polipropileno na área doadora do TRAM propiciou baixa incidência de hérnias e abaulamentos abdominais.
Palavras-chave: Mamoplastia; Hérnia abdominal; Retalhos cirúrgicos; Retalho miocutâneo; Polipropilenos.
The transverse rectus abdominis myocutaneous (TRAM) flap, originally described in 19821, is an established method for breast reconstruction, especially in women who have voluminous breasts.
The TRAM flap has enough tissue to reconstruct larger-volume breasts without the need to use a silicone prosthesis. The disadvantage of the flap is the large defect of the donor area and may cause weakness of the abdominal wall, in addition to hernias and bulges2. The reconstruction of the breast with the TRAM flap can be immediately performed, simultaneously with mastectomy, or later. In addition, the TRAM flap can be based on one pedicle or two, being defined as monopedicled or bipedicled. The most common breast cancer in the female population is invasive ductal carcinoma1.
In 1987, Hartrampf3 reported his experience in 335 patients who underwent breast reconstruction with the TRAM flap, with a complication rate in the abdominal wall of 1.6%, of which 0.3% were abdominal hernias, 0.6% were bulges, and 0.6% were defects in the upper anterior rectus sheath. In another study, the authors reported incidence rates of hernias and abdominal bulges of up to 20% in patients who underwent breast reconstruction with a TRAM flap and closure of the donor area without a polypropylene mesh4.
Some authors advocate the partial preservation of the rectus abdominis muscle, arguing that this would reduce the incidence of hernias, bulges, and weakness of the abdominal wall. However, the use of this surgical approach has not been effective5.
The choice of the pedicled flap, either monopedicled or bipedicled, seems to influence the incidence of abdominal complications, with a higher incidence in bipedicled flaps, as the lesion in the donor area is greater. However, one study with a long-term follow-up observed no statistically significant difference in the incidence of hernias and bulges between patients with closed monopedicled and bipedicled TRAM flaps without the use of a polypropylene mesh6.
Innumerable factors contribute to the incidence of hernias and bulges in patients who have undergone reconstruction with the TRAM flap, not only the presence or absence of a polypropylene mesh or the type of pedicle. Therefore, these patients must undergo a multifactorial analysis, including factors such as age, smoking, postoperative radiation, and comorbidities7-9.
Among the various surgical attempts to decrease the postoperative incidence of hernias and bulges at the donor site of the TRAM flap, some authors have started to advocate the use of a polypropylene mesh in the area of the lesion. However, it has been used only in cases in which it is possible to close the abdominal defect primarily2,10. The routine use of a mesh has been restricted due to the argument of there being an increased risk of infections or extrusions2,11. Some studies have demonstrated the efficacy and safety of the use of the mesh along with incidences of hernias and infections of 1.5%12,13.
Two studies have advocated the use of a polypropylene mesh covering the whole of the abdomen, not only the defect, claiming that the use of the mesh resulted in better body contour and lower indexes of hernias and bulges14,15. In another study, the authors advocated the use of a double-layer Merselene mesh for the closure of the defect in the donor area of the TRAM flap and demonstrated a lower incidence of hernias and smaller bulges than those with closure without the mesh16.
In surgical practice, some surgeons have used two overlapping polypropylene layers in the donor area of the TRAM flap in an effort to further reduce the incidence of hernias and bulges when compared with the use of one mesh layer alone. However, this surgical approach has not been published yet and its efficacy has not been proven.
OBJECTIVE
The objective of this study was to report the surgical approach used in the repair of the donor area of a double-layer polypropylene mesh and to evaluate the incidence of hernias and bulging in the postoperative period of breast reconstructions with the TRAM flap.
METHODS
A prospective cohort study was conducted in 24 patients who underwent unilateral breast reconstruction with a monopedicled or bipedicled TRAM flap and repair of the donor area with two overlapping layers of a polypropylene mesh. The surgeries were performed by the same surgeon, between March 2011 and July 2012, at the Hospital Pérola Byington, a woman's health referral center, in São Paulo, SP.
The patients were evaluated as to the incidence of hernias and abdominal bulges through physical examination at 3, 6, and 12 months after operation. In addition, the demographic data of the patients were evaluated with the use of a questionnaire (Chart 1).
In the physical assessment, the examination of the patient was standardized, first, through abdominal palpation while standing and then lying down, with and without increased intra-abdominal pressure (Valsalva maneuver). All physical examinations were performed by members of the surgical team. In doubtful cases, ultrasonography examination of the abdominal wall was used as a complementary diagnostic tool to detect the presence of hernia or abdominal bulging.
For the purpose of this study, hernia was considered a protrusion of the abdominal wall through a defect of the fascia and bulging, a protrusion or flaccidity without a defect of the fascia.
Surgical Technique
In all the TRAM flaps, either monopedicled or bipedicled, the whole thickness of the rectus abdominis muscle was used; that is, partial preservation of the muscle was not adopted.
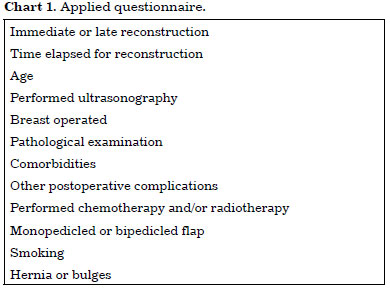
The closure of the TRAM flap donor area was performed with a polypropylene mesh. Initially, after the creation of the defect in the abdominal wall by the transfer of the TRAM flap, an approximation without tension of the anterior sheath of the aponeurosis of the rectus abdominis muscle was performed with a monofilament nylon 2-0 (Ethicon) and "X"-type sutures (Figure 1). To preserve the perforating vessels of the rectus abdominis muscle, it was necessary to include a portion of the anterior aponeurosis of the rectus abdominis muscle in the TRAM flap, creating an aponeurotic defect at the height of the umbilical scar in the region of the rectus abdominis of approximately 8 by 6 cm. The aponeurosis of the rectus abdominis was sutured approaching its borders without tension up to the portion of the defect created after the transfer of the TRAM flap to the breast.
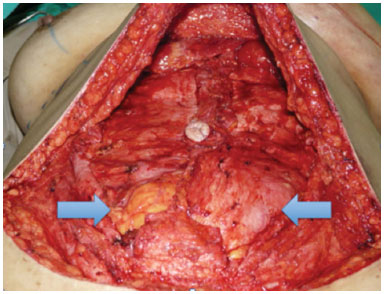
Figure 1. Defect in the donor area, indicated by the arrows, with a bipedicled TRAM flap.
Thereafter, a polypropylene mesh (Ethicon) the size of the defect of the aponeurosis was cut, placed in contact with the posterior sheath of the remaining abdominal fascia, and sutured with nylon monofilament 3.0 sutures (Ethicon) in "U" on the edges of the defect on the fascia and on the mesh (Figure 2).
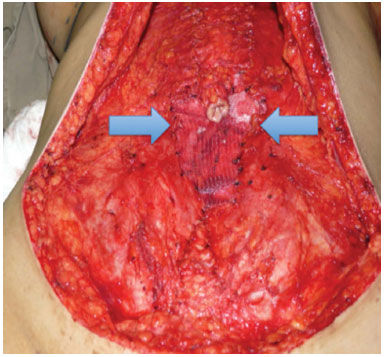
Figure 2. First polypropylene mesh layer, delimited by arrows, sutured to the edges of the aponeurotic defect of the bipedicled TRAM flap.
On top of this layer, another 20- ' 30-cm polypropylene mesh was placed to cover an area delimited inferiorly by the pubic symphysis, superiorly by the lower margins of the last ribs and laterally by the anterior superior iliac spines. The mesh was fixed with monofilament nylon 3-0, first in the periosteum of the anterior superior iliac spines and then with continuous suture, fixed throughout its perimeter to the oblique external aponeurosis muscle and rectus abdominis (Figure 3). An opening was made in the polypropylene mesh where the umbilicus was externalized.
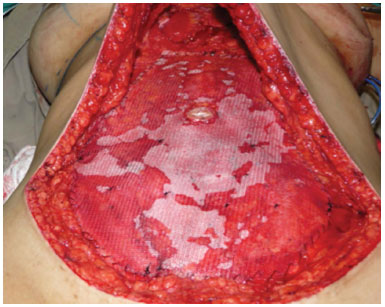
Figure 3. Second polypropylene mesh layer, superimposed on the first, covering the whole of the abdomen.
Before the suture of the abdomen by planes, the same was drained with a Porto-Vac 4.8 drain (Figure 4).

Figure 4. Sutured abdominal flap drained with a Porto-Vac tube in a patient who underwent left breast reconstruction with a bipedicled TRAM flap.
Inclusion Factors
Non-inclusion FactorsPatients who had undergone unilateral breast reconstruction with a monopedicle or bipedicle TRAM flap and closure of the aponeurosis defect according to the operative approach described earlier; Patients with a body mass index (BMI) lower than 30 kg/m2; Patients without hernias, bulges, or previous abdominal surgeries; Patients without comorbidities or with clinically controlled diseases.
Exclusion FactorBreast reconstruction with a bipartite TRAM flap; Patients who had undergone bilateral breast reconstruction with a TRAM flap or aponeurosis closure with other approaches; Patients with a BMI greater than 30 kg/m2; Patients with uncontrolled comorbidities.
- Patients who missed any scheduled follow-up in the study.
RESULTS
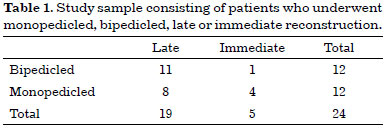
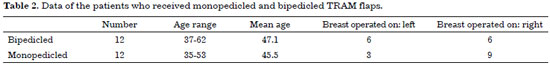
Of the 24 patients, 12 (50%) received monopedicled flaps and another 12 (50%) received bipedicled flaps (Table 1). Five (21%) patients underwent immediate reconstruction, and 19 (79%) patients underwent late reconstruction (Table 1). The age of the patients ranged from 35 to 62 years (mean, 46.3 years; Tables 2 and 3). All the patients were followed up for up to 1 year after surgery and evaluated at 3, 6, and 12 months postoperatively.
The left breast was operated in 9 patients (37.5%); and the right breast, in 15 (62.5%) (Tables 2 and 3). The patients who had late breast reconstruction had a delay between mastectomy and reconstruction of 8 months to 11 years (47.8 months on average; Table 3). The patient who waited 11 years to undergo operation had mastectomy performed at another service and lived in another state. Disregarding this patient, the mean waiting time was 24.5 months. All the patients in this study were diagnosed with invasive ductal carcinoma in the pathology examination (Table 4).
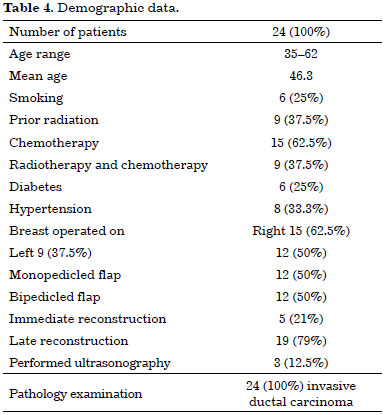
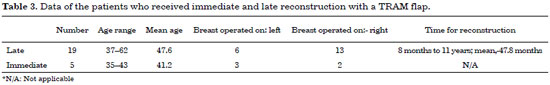
Only 1 patient (4.16%) who underwent late reconstruction with a bipedicled TRAM flap developed abdominal bulging at 12 months of follow-up (Tables 5 and 6). The bulging was located mainly in the lower abdomen and in the left portion of the upper abdomen (Figure 5). The patient did not mind this complication and did not want to be reoperated. None of the patients had an abdominal hernia. One patient (4.16%) had a granuloma in the periumbilical region observed at 6 months, which was reapproached with partial withdrawal of the mesh in the periumbilical region (Table 7). No cases of extrusion or infection of the mesh were encountered.
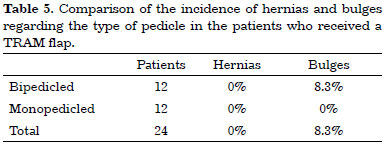
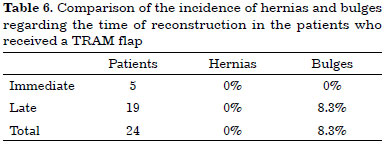
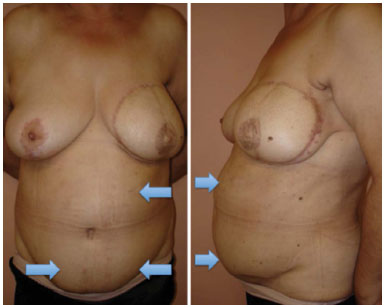
Figure 5. Bulging after late reconstruction with a bipedicled TRAM flap and closure of the aponeurotic defect with a double-layer mesh.
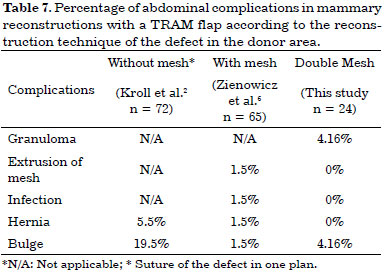
None of the patients who underwent reconstruction with a monopedicled TRAM flap developed any abdominal complication. Among the patients who underwent only reconstruction with a bipedicled TRAM flap, 8.3% had bulging (Table 5).
DISCUSSION
In reconstructive surgeries, the patient is subjected to a trade-off to improve the form and function of a compromised region of the body to the detriment of a smaller and acceptable loss of form and function in another area of the body. The relationship between the benefit and loss should always be analyzed; if this trade-off is not even, reconstruction is useless11. Given this premise, every effort should be made to reduce the incidence of abdominal complications associated with breast reconstruction with a TRAM flap.
The reported incidence of hernias and abdominal bulges post-breast reconstruction with TRAM flaps decreased significantly after the use of a polypropylene mesh in the donor area2,6,7. In medical practice, many plastic surgeons have used a double-layer polypropylene mesh in an attempt to further reduce the incidence of these complications compared with the use of only one layer. However, the existing literature has not described the surgical approach followed in this study.
The groups of patients in this study are heterogeneous and ideally should be compared with the same age groups and indicated to undergo the same reconstruction as follows: late or immediate, and monopedicled, or bipedicled. The fact that the reconstruction is immediate or late did not affect the results in terms of abdominal complications either with a monopedicled or bipedicled flap. This finding can be explained by the greater defect in the donor area in bipedicled TRAM flaps.
In monopedicled flaps, the lesser defect in the donor area and the preservation of the contralateral rectus abdominis muscle influences the lower incidence of hernias and bulges8. In this case, a large part of the defect could be closed primarily so that the amount of mesh used over the defect is lower. The second mesh used over the first is the same size as the one used in the bipedicled TRAM flap, as its fixation points are the same and do not change according to the size of the defect. Thus, a lower incidence of hernias and bulges is expected in cases of breast reconstruction with a monopedicled flap than with a bipedicled flap, as was observed in this study.
Another point that must be observed is regarding the time of postoperative follow-up, which varied considerably between the studies. In the present study, all the patients were followed up for 1 year, while in other studies, such follow-up ranged from months up to 7 years6,9. The hernias and bulges can manifest only after several years of surgery6. Thus, the incidences of hernias and bulges in the present study could be greater if the postoperative follow-up were to be extended.
In the present study, half of the patients underwent breast reconstruction with a bipedicled flap, a much larger number than that reported in some studies in which the bipedicled flap was used in less than 5% of patients2,12. This was due to the large number of mastectomized patients submitted to adjuvant radiotherapy and programmed for late reconstruction. In these cases of adjuvant radiotherapy, we opted for the use of the bipedicled flap due to its increased viability. Another indication of the use of bipedicled flaps was the large volume of the contralateral mastectomized breast. In immediate cases, the indication of the choice of the pedicle was based only on the size of the contralateral breast.
The use of a double-layer polypropylene mesh provides a higher volume of foreign material to the body, thus presenting a larger theoretical risk of complications related to the mesh, such as extrusions and infections6. In spite of this reasoning, as can be observed in Table 7 of this study, no complications related to the use of this material occurred. We found only one case of periumbilical granuloma, a complication that was not evaluated in other studies2,12.
Some of the limitations found in the present study include the following confounding variables: smokers and nonsmokers, with or without chemotherapy and/or radiotherapy, variation in age and, presence of comorbidities.
Further studies with longer follow-up periods and larger samples are required to confirm the superiority of this surgical approach to others in reducing abdominal complications.
CONCLUSION
The use of two polypropylene mesh layers in the closure of the defect in the donor area of breast reconstruction with TRAM flaps presented a low incidence of bulging and no incidence of abdominal hernia. None of the cases had infection or extrusion of the mesh. The approach described may be a safe option to decrease the incidence of hernias and bulges in breast reconstructions using TRAM flaps.
REFERENCES
1. Hartrampf CR, Scheflan M, Black PW. Breast reconstruction with a transverse abdominal island flap. Plast Reconstr Surg. 1982;69(2):216-25. PMID: 6459602 DOI: http://dx.doi.org/10.1097/00006534-198202000-00006
2. Kroll SS, Marchi M. Comparison of strategies for preventing abdominal-wall weakness after TRAM flap breast reconstruction. Plast Reconstr Surg. 1992;89(6):1045-51. DOI: http://dx.doi.org/10.1097/00006534-199206000-00007
3. Hartrampf CR. Breast reconstruction with a transverse abdominal island flap: A retrospective evaluation of 355 patients. Plast Reconstr Surg. 1987;(1):123-7. DOI: http://dx.doi.org/10.1055/s-2008-1081245
4. Lallement M, Missana MC, Bourgeon Y, Abbes M. Closure of the abdominal wall after removal of a mucocutaneous flap from the transverse rectus abdominis for breast reconstruction. Apropos of 48 cases. Review of the literature. Ann Chir Plast Esthet. 1994;39(6):733-41.
5. Hartrampf CR Jr, Bennett GK. Autogenous tissue reconstruction in the mastectomy patient. A critical review of 300 patients. Ann Surg. 1987;205(5):508-19. PMID: 2953315 DOI: http://dx.doi.org/10.1097/00000658-198705000-00009
6. Mizgala CL, Hartrampf CR Jr, Bennett GK. Assessment of the abdominal wall after pedicled TRAM flap surgery: 5- to 7-year follow-up of 150 consecutive patients. Plast Reconstr Surg. 1994;93(5):988-1002. DOI: http://dx.doi.org/10.1097/00006534-199404001-00013
7. Paige KT, Bostwick J 3rd, Bried JT, Jones G. A comparison of morbidity from bilateral, unipedicled and unilateral, unipedicled TRAM flap breast reconstructions. Plast Reconstr Surg. 1998;101(7):1819-27. DOI: http://dx.doi.org/10.1097/00006534-199806000-00007
8. Nahabedian MY, Manson PN. Contour abnormalities of the abdomen after transverse rectus abdominis muscle flap breast reconstruction: a multifactorial analysis. Plast Reconstr Surg. 2002;109(1):81-7. DOI: http://dx.doi.org/10.1097/00006534-200201000-00014
9. Ascherman JA, Seruya M, Bartsich SA. Abdominal wall morbidity following unilateral and bilateral breast reconstruction with pedicled TRAM flaps: an outcomes analysis of 117 consecutive patients. Plast Reconstr Surg. 2008;121(1):1-8. PMID: 18176197 DOI: http://dx.doi.org/10.1097/01.prs.0000295378.43033.c4
10. Bucky LP, May JW Jr. Synthetic mesh. Its use in abdominal wall reconstruction after the TRAM. Clin Plast Surg. 1994;21(2):273-7. PMID: 8187420
11. Drever JM. Abdominal closure after TRAM flaps. Plast Reconstr Surg. 1996;97(5):1080. DOI: http://dx.doi.org/10.1097/00006534-199604001-00038
12. Zienowicz RJ, May JW Jr. Hernia prevention and aesthetic contouring of the abdomen following TRAM flap breast reconstruction by the use of polypropylene mesh. Plast Reconstr Surg. 1995;96(6):1346-50. DOI: http://dx.doi.org/10.1097/00006534-199511000-00017
13. Wan DC, Tseng CY, Anderson-Dam J, Dalio AL, Crisera CA, Festekjian JH. Inclusion of mesh in donor-site repair of free TRAM and muscle-sparing free TRAM flaps yields rates of abdominal complications comparable to those of DIEP flap reconstruction. Plast Reconstr Surg. 2010;126(2):367-74. DOI: http://dx.doi.org/10.1097/PRS.0b013e3181de1b7e
14. Moscona RA, Ramon Y, Toledano H, Barzilay G. Use of synthetic mesh for the entire abdominal wall after TRAM flap transfer. Plast Reconstr Surg. 1998;101(3):706-10. DOI: http://dx.doi.org/10.1097/00006534-199803000-00018
15. Moscona R. Further clinical experience with synthetic mesh for the entire abdominal wall after TRAM flap breast reconstruction. Plast Reconstr Surg. 2005;116(6):1724-5. PMID: 16267438 DOI: http://dx.doi.org/10.1097/01.prs.0000185612.48585.fc
16. Drever JM, Hodson-Walker N. Closure of the donor defect for breast reconstruction with rectus abdominis myocutaneous flaps. Plast Reconstr Surg. 1985;76(4):558-65. PMID: 2930860 DOI: http://dx.doi.org/10.1097/00006534-198510000-00013
1. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
2. Hospital do Servidor Público Municipal de São Paulo, São Paulo, SP, Brazil
3. Hospital Pérola Byington, São Paulo, SP, Brazil
4. Universidade Federal de São Paulo, São Paulo, SP, Brazil
Institution: Hospital Pérola Byington - Centro de referência da saúde da mulher, São Paulo, SP, Brazil.
Corresponding author:
Ricardo Eustachio de Miranda
Rua Batataes, 324
São Paulo, SP, Brazil Zip Code 01423-010
E-mail: ricardomiranda@hotmail.com
Article received: July 13, 2013.
Article accepted: February 4, 2014.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter