

Original Article - Year 2015 - Volume 30 -
Incidence of cleft palate fistula after von Langenbeck palatoplasty with extended intravelar veloplasty
Incidência de fistula após palatoplastia à Von Langenbeck com veloplastia intravelar estendida
ABSTRACT
INTRODUCTION: Cleft lip and palate is the most common craniofacial deformity, with an estimated incidence of 1 case per 600 live births in Brazil. The aim of this study was to determine the incidence of fistula among patients undergoing palatoplasty with extended intravelar veloplasty.
METHODS: This retrospective descriptive study evaluated 25 patients operated between September 2011 and September 2012 by the same surgeon. The von Langenbeck technique combined with extended intravelar veloplasty was performed in all patients. The study excluded patients with palatal fistulas, syndromes, or other malformations. The age at palatoplasty varied between 12 and 159 months, and the average age was 30.6 months. Nineteen patients were selected, comprising 11 (58%) male patients and 8 (42%) female patients. Isolated cleft palate was the most common deformity, found in 9 (47%) patients. Unilateral (left) trans-foramen cleft was present in 7 (37%) patients, and bilateral trans-foramen cleft was seen in 3 (16%) patients.
RESULTS: Only 2 (11%) patients had palatal fistula in a postoperative follow-up period of 6 months.
CONCLUSION: The von Langenbeck technique associated with extended veloplasty resulted in a low incidence of cleft palate fistulas (11%) compared with the rate found in previous studies (7%-42%).
Keywords: Cleft lip and palate; Cleft palate; Reconstructive surgical procedures; Craniofacial abnormalities.
RESUMO
INTRODUÇÃO: A fissura labiopalatina é a deformidade craniofacial mais frequente e sua incidência é estimada em 1:600 nascidos vivos no Brasil. O objetivo desse estudo é avaliar a incidência de fístulas para os pacientes submetidos à palatoplastia com veloplastia intravelar estendida.
MÉTODOS: Trata-se de estudo descritivo retrospectivo com 25 pacientes que foram operados pelo mesmo cirurgião no período de setembro de 2011 a setembro de 2012. A técnica de Von Langenbeck, juntamente com a veloplastia intravelar estendida, foi realizada em todos os pacientes. Foram excluídos do estudo os pacientes com fístulas palatinas, portadores de síndromes ou outras malformações. A idade média da realização da palatoplastia foi de 30,6 meses, variando de 12 meses a 159 meses. Foram selecionados 19 pacientes: onze (58%) do gênero masculino e oito (42%) do gênero feminino. A fissura palatal isolada foi a mais comum, encontrada em nove (47%) pacientes. A fissura transforame esquerda estava presente em sete (37%) pacientes e três (16%) pacientes eram portadores de fissura transforame bilateral.
RESULTADOS: Somente dois (11%) pacientes evoluíram com fístula palatina até o acompanhamento pós-operatório de 6 meses.
CONCLUSÃO: A técnica de Von Langenbeck associada à veloplastia estendida mostrou-se com baixa incidência de fístulas palatinas (11%) quando comparada ao índice encontrado na literatura mundial (7% a 42%).
Palavras-chave: Fissura labiopalatina; Fissura palatina; Procedimentos cirúrgicos reconstrutivos; Anormalidades craniofaciais.
Cleft lip and palate is the most common craniofacial deformity and is caused by a defect in the closure of the lateral frontonasal processes with the medial processes between the 8th and 12th week of intrauterine life. It has a multifactorial inheritance and may be associated with nutritional deficiencies, use of some medications, tobacco and alcohol use, and radiation, and is associated with other syndromes in 20% to 30% of the cases1. In Brazil, its incidence is approximately 1 in 600 live births2, and this incidence is higher in East Asian countries (1:400) and lower in countries with Caucasian populations (1:1500 to 1:2000). The performance of palatoplasty between the age of 12 and 18 months involves closing the communication between the oral and nasal cavities and the repair of the soft palate muscles, with the view to promote adequate speech development and dental alignment with minimal impact on craniofacial growth3-5.
The first technique used for surgical repair of the palate dates from 1891 and was reported by von Langenbeck. It consists in preparing anterior and posterior bipediculated mucoperiosteal flaps for the closure of the oral mucosa, as well as for the detachment and repair of the nasal mucosa6. Later, other techniques were developed to increase the palatal length with the use of V-Y flaps in the anterior palate (Veau-Wardill-Kilner); however, these techniques still had unsatisfactory results7,8. In the 1960s, Braithwaite and Kriens highlighted the importance of the repositioning of the soft palate muscles, especially the elevator and tensor muscles of the soft palate, because of the need to perform intravelar palatoplasty.
In 1980, Leonard Furlow proposed palatal stretching with the preparation of double triangular flaps (double-opposing Z-plasty) of muscles and the mucosa of the soft palate, and this technique improved the palatal length and the contracture of the linear scar, leading to a lower risk of scar retraction; improved the movement of the palate; and decreased, to some extent, the presence of velopharyngeal insufficiency (VPI)9. However, Furlow's technique had a limited indication for patients with broad cleft palates owing to the major technical difficulties in preparing the triangular flaps. In addition, the literature still reports high rates of VPI with the use of these techniques, reaching 35% at some centers and an incidence of cleft palate fistulas of approximately 7% to 42%.
In 2003, Brian Sommerlad performed a major detachment of the soft palate muscles with the use of a microscope, discriminating the tensor and elevator muscles of the soft palate, its repair and retropositioning10,11, resulting in a long palate and lower failure rates for VPI (5% to 10%) and an incidence of cleft palate fistulas between 10% and 15%12.
OBJECTIVE
The aim of this study was to determine the incidence of cleft palate fistulas in patients undergoing palatoplasty with the von Langenbeck technique with extended intravelar veloplasty, but without using a microscope and discriminating the velopharyngeal muscles.
METHODS
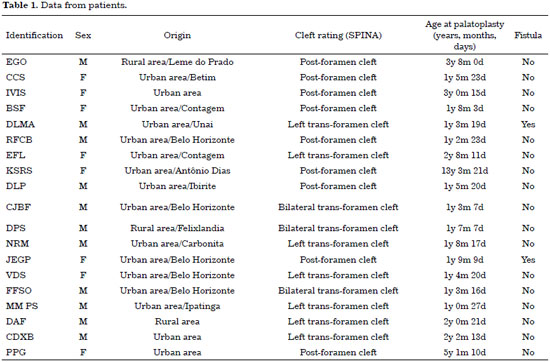
In this retrospective descriptive study, we analyzed the medical records of 25 patients registered at the Treatment and Rehabilitation Center for Craniofacial Deformities and Cleft Lip and Palate (Centro de Tratamento e Reabilitação de Fissuras Labiopalatais e Deformidades Craniofaciais-CENTRARE) between September 2011 and September 2012. Nineteen patients were selected, comprising 11 (58%) male patients and 8 (42%) female patients. Isolated cleft palate was the most common deformity, represented by 9 (47%) cases. Seven (37%) patients presented unilateral (left) trans-foramen cleft, and 3 (16%) patients presented bilateral trans-foramen clefts (Figure 1). The age at palatoplasty varied between 12 and 159 months, and the average age was 30.6 months. Most patients (79%) were urban dwellers of the metropolitan region of Belo Horizonte, state of Minas Gerais, Brazil, and of the interior of the state, and only 4 (21%) patients were from rural areas. The parents did not sign any consent form because this procedure was initiated at our service only in January 2013 and the patients were operated before this date.

Figure 1. Classification of clefts.
All patients were operated by the same surgeon and were monitored in an outpatient basis for a minimum of 6 months, for the evaluation of cleft palate fistulas on the basis of clinical examination alone. The surgical technique used in all patients was von Langenbeck palatoplasty with extended intravelar veloplasty. Surgery was performed under balanced general anesthesia associated with the local infiltration of an anesthetic solution consisting of 0.5% lidocaine, 0.15% bupivacaine, and epinephrine at 1:100,000.
The surgery was initiated without prior methylene blue demarcation, and the incision was made in the transition between the oral and nasal mucosa and the preparation of the mucoperiosteal flaps, which were detached as bipediculated flaps in the anterior and posterior region of the oral mucosa for the repair of the hard palate by using lateral relaxing incisions. The velopharyngeal muscles were thoroughly released en bloc from the posterior nasal spine and palatine bone through muscle retropositioning for the repair of the soft palate (Figures 2 and 3). Therefore, the hard palate was repaired in two layers (nasal and oral mucosa) and the soft palate was repaired in three layers (nasal mucosa, velopharyngeal muscles, and oral mucosa).

Figure 2. Identification and dissection of the palatal muscles.
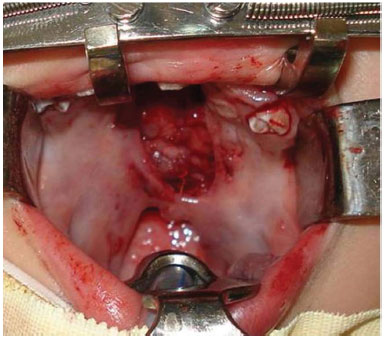
Figure 3. Repair of the palatal muscle.
Vicryl 4.0 was used for all sutures. Prophylactic cephalothin (30 mg/kg) was administered for anesthetic induction, and the patients were discharged on the next day. All patients took an oral antibiotic (amoxicillin) at home for 7 days, and outpatient visits were scheduled after 7, 21, 45, 90, and 120 days. A liquid/soft diet was maintained for 30 to 45 days, and most patients were referred for speech therapy at 45 days after the surgery. The cleft palate fistulas were identified on an outpatient basis according to complaints of nasal reflux and physical examination of patients, by using tongue depressors and inspection of the palate (Table 1).
RESULTS
Of the 25 patients selected, 6 were excluded because of the presence of syndromes and congenital anomalies (1 patient), or cleft palate fistula after a previous palatoplasty (5 patients). There were no immediate complications postoperatively, including bleeding, dehiscence, infections, or airway obstruction. The incidence of cleft palate fistula was 11% (2 patients), and the patients were monitored on an outpatient basis for 6 months. The two cases of cleft palate fistula were located in the transition between the hard and soft palate, and their transverse diameter was < 5 mm. The patients in those cases had nasal reflux only for liquids, with mild hypernasality, and did not need to use mime or exert effort during speech. They were monitored by the speech therapist, and the decision for surgical treatment of the fistulas was based on the symptoms observed after the end of the speech therapy.
DISCUSSION
We believe that the combination of von Langenbeck palatoplasty with extended intravelar veloplasty can be a good strategy for closing the palate in patients with cleft lip and palate or isolated cleft palate, and results in a low incidence of cleft palate fistulas (11%), with a lower impact on craniofacial growth and better speech outcomes owing to the retropositioning of the velopharyngeal muscles.
It is known that cleft palate fistulas are the most common complications after palatoplasty (10%-42%). They are commonly found in the transition between the hard and soft palates and in the anterior (alveolar) region of the hard palate. Cleft palate fistulas with symptoms of nasal reflux and hypernasality should be considered for surgical treatment. Several techniques can be used to close the palate, and the Veau-Wardill-Kilner technique is the most commonly performed at many reference centers; nevertheless, the von Langenbeck technique with bipediculated flaps is also common.
We believe that the von Langenbeck technique we selected can be easily executed, particularly in patients with isolated cleft palate. However, several factors influence the occurrence of acute complications, such as age, preoperative and intraoperative conditions, infection at the surgical site and upper airways, condition and maintenance of the teeth, and access to referral centers; this latter factor may limit the access of patients who live in rural and provincial areas. Often, early diagnosis and proper treatment of infections in the upper airways can prevent dehiscence of the surgical wound on the palate and decrease the likelihood of the occurrence of cleft palate fistulas. One of these factors may have contributed to the formation of the fistulas reported in our study because both patients lived in rural areas.
At our service, it is routine to maintain oral sequential antibiotic therapy for 7 days for all patients, considering that most patients live in remote locations and have limited access to health care. Tooth decay is also a contributing factor for the increase of the incidence of wound infections and consequently of cleft palate fistulas. The preoperative tests requested should be within normal limits, and the hemoglobin level should not be < 10 g/dL. Nutritional factors are also important in wound healing, and postoperative care is essential for a good recovery. A liquid/soft diet should be maintained for 30 to 45 days to prevent high blood pressure in the palatal tissue during healing and to facilitate cleaning after feeding; moreover, we believe that it can decrease the possibility of infections in the surgical site due to the accumulation of food debris.
The average age at palatoplasty of 30.6 months was considered high because the protocol adopted in CENTRARE suggests the performance of the surgery at ages between 12 and 18 months. In patients who are operated late, particularly those aged > 5 years, there is a higher technical difficulty for detachment of the flaps, which are closely attached in most of these cases, have limited mobility, and have a greater probability of bleeding, dehiscence, and necrosis. However, in our study, cleft palate fistulas did not occur in patients who were operated late. Most patients came from urban provincial regions of the state, often with poor access to specialized centers, and therefore were registered late in the reference centers.
Veloplasty with extended dissection of the velopharyngeal muscles was performed to improve the speech of the patients, and in consideration of the reported rates of VPI in the literature of up to 35%. This treatment can be difficult, with limited results. Normally, we perform palatoplasty by using Furlow's technique with double-opposing Z-plasty for the correction of VPI, or even repalatoplasty with extended veloplasty in patients initially operated with another technique or those coming from other services. In complicated cases with limited palate mobility, our choice is the preparation of the superior pedicle pharyngeal flaps by using the technique described by Hynes. The evaluation and follow-up by experienced speech therapists are essential to recover the speech of the patients, particularly those who were operated late and presenting with compensatory articulation disorders.
The evaluation of the presence of cleft palate fistulas was exclusively clinical in our patients. Endoscopic tests such as fibronasolaryngoscopy are primarily used to evaluate the function of the velopharyngeal sphincter and are required in cases of VPI. After the examination, we can schedule the best treatment for VPI, either by using palatal stretching with Furlow's technique in cases of mobile and short palate or the preparation of the pharyngeal flaps as described by Hynes in patients with limited velopharyngeal mobility and good movement of the lateral and posterior walls of the pharynx12-14.
Single-stage palatoplasty is the technique most commonly used at many reference centers for the treatment of fissures. This choice is based on the repair of the palate during the acquisition of speech (age between 12 and 18 months), facilitating speech development and reducing the occurrence of articulation disorders. Significant deficits in maxillary growth were not demonstrated scientifically compared with two-stage palatoplasty, in which intravelar veloplasty is performed at the age of 12 months and the hard palate is repaired later, approximately at the ages of 5 to 7 years. However, both techniques produce deficits in craniofacial growth that are absent in patients who did not undergo any surgery15,16. We believe that the presence of scars, fibrosis, and particularly areas of healing by secondary intention in the anterior palate are largely responsible for the imprisonment of the maxilla and the consequent limitation in growth. This leads to angle class III malocclusion, and sometimes patients undergo orthognathic surgery in adolescence.
Future studies with a larger sample size and longer follow-up are necessary for further assessment of speech outcomes and maxillary growth.
CONCLUSION
von Langenbeck palatoplasty with extended intravelar veloplasty resulted in a low incidence of cleft palate fistulas (11%), despite the stronger detachment of the posterior region of the palate. The rates found in the literature range between 7% and 42%.
REFERENCES
1. Rajion ZA, Alwi Z. Genetics of cleft lip and palate: a review. Malays J Med Sci. 2007;14(1):4-9.
2. Franco D, Iani M, Passalini R, Demolinari I, Arnaut M, Franco T. Profile evaluation of patients with cleft lip and palate undergoing surgery at a reference center in Rio de Janeiro, Brazil. Plast Surg Int. 2012;2012:620302. DOI: http://dx.doi.org/10.1155/2012/620302
3. da Silva Filho OG, Rosa LA, Lauris Rde C. Influence of isolated cleft palate and palatoplasty on the face. J Appl Oral Sci. 2007;15(3):199-208. DOI: http://dx.doi.org/10.1590/S1678-77572007000300009
4. Gongorjav NA, Luvsandorj D, Nyanrag P, Garidhuu A, Sarah EG. Cleft palate repair in Mongolia: Modified palatoplasty vs. conventional technique. Ann Maxillofac Surg. 2012;2(2):131-5.
5. de Ladeira PR, Alonso N. Protocols in cleft lip and palate treatment: systematic review. Plast Surg Int. 2012;2012:562892. DOI: http://dx.doi.org/10.1155/2012/562892
6. Leow AM, Lo LJ. Palatoplasty: evolution and controversies. Chang Gung Med J. 2008;31(4):335-45.
7. Mølsted K. Treatment outcome in cleft lip and palate: issues and perspectives. Crit Rev Oral Biol Med. 1999;10(2):225-39. DOI: http://dx.doi.org/10.1177/10454411990100020801
8. Paranaíba LM, Almeida HD, Barros LM, Martelli DR, Orsi Júnior JD, Martelli Júnior H. Current surgical techniques for cleft lip-palate in Minas Gerais, Brazil. Braz J Otorhinolaryngol. 2009;75(6):839-43. DOI: http://dx.doi.org/10.1016/S1808-8694(15)30546-2
9. Gage-White L, Mankekar C. Furlow palatoplasty-double opposing z-plasty. Indian J Otolaryngol Head Neck Surg. 1997;49(4):422-3. DOI: http://dx.doi.org/10.1007/BF02994668
10. Sommerlad BC. Surgical management of cleft palate: a review. J R Soc Med. 1989;82(11):677-8.
11. Sommerlad BC. A technique for cleft palate repair. Plast Reconstr Surg. 2003;112(6):1542-8. DOI: http://dx.doi.org/10.1097/01.PRS.0000085599.84458.D2
12. Becker M, Hansson E. Low rate of fistula formation after Sommerlad palatoplasty with or without lateral incisions: an analysis of risk factors for formation of fistulas after palatoplasty. J Plast Reconstr Aesthet Surg. 2013;66(5):697-703. DOI: http://dx.doi.org/10.1016/j.bjps.2013.01.031
13. Bicknell S, McFadden LR, Curran JB. Frequency of pharyngoplasty after primary repair of cleft palate. J Can Dent Assoc. 2002;68(11):688-92.
14. Murthy J. Descriptive study of management of palatal fistula in one hundred and ninety-four cleft individuals. Indian J Plast Surg. 2011;44(1):41-6. DOI: http://dx.doi.org/10.4103/0970-0358.81447
15. Pradel W, Senf D, Mai R, Ludicke G, Eckelt U, Lauer G. One-stage palate repair improves speech outcome and early maxillary growth in patients with cleft lip and palate. J Physiol Pharmacol. 2009;60 Suppl 8:37-41.
16. Pereira RMR, Melo EMC, Coutinho SB, Vale DM, Siqueira N, Alonso N. Avaliação do crescimento craniofacial em portadores de fissura labiopalatina submetidos a palatoplastia em tempo único. Rev Bras Cir Plást. 2011;26(4):624-30.
1. Hospital da Baleia - Fundação Benjamim Guimarães CENTRARE, Belo Horizonte, MG, Brazil
2. Sociedade Brasileira de Cirurgia Plástica, Belo Horizonte, MG, Brazil
Institution: Hospital da Baleia - Fundação Benjamim Guimarães CENTRARE, Belo Horizonte, MG, Brazil.
Corresponding author:
Hugo Leonardo de Resende Rodrigues
Rua Juramento, 1464
Belo Horizonte, MG, Brazil Zip Code 30285-000
E-mail: hugo@doutorhugorodrigues.com.br
Article received: July 29, 2013.
Article accepted: February 4, 2014.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter