

Articles - Year 2004 - Volume 19 -
Abdominoplasty Combined with Intra-abdominal Gynecologic Surgery
Abdominoplastia Associada à Cirurgia Ginecológica Cavitária
ABSTRACT
This paper desenhes the association of abdominoplasty and intra-abdominal gynecologie surgery in 51 patients, with no previous abdominal fiap undermining. The gynecologist starts the procedure with a midline infraumbilieal incision, which appropriately exposes the abdomen, and avoids trauma and contact of intra-abdominal material with the fiaps to be preserved. The fiap may be undermined in abdominoplasty by block resection or infra- or supraumbilieal undermining.
Keywords: Abdominoplasty; abdominoplasty combined with intra-abdominal surgery; abdominoplasty combined with gynecologic surgery; combined surgeries
RESUMO
Este trabalho descreve a associação de abdominoplastia com cirurgia ginecológica cavitária, em 51 pacientes, sem descolamento prévio do retalho abdominal.
O ginecologista inicia o procedimento através de incisão mediana infra-umbilical, a qual lhe propicia adequada exposição da cavidade, além de evitar o contato do material cavitário e trauma com os retalhos que permanecerão.
O descolamento do retalho na abdominoplastia poderá ser realizado por ressecção em bloco ou por descolamento infra ou supra-umbilical.
Palavras-chave: Abdominoplastia; abdominoplastia associada a cirurgia cavitária; abdominoplastia associada a cirurgia ginecológica; cirurgias associadas
Abdominoplasty associated with intra-abdominal gynecologic surgery has been an attractive combination for gynecologists given it provides a better and wider operative field(1-3), as well as for patients, because it solves their organic and aesthetic problems in a single surgical/anesthetic procedure and one postoperative period, thus reducing hospital costs; in addition, it sometimes helps justifying abdominoplasty to husbands, families and employers(1,2,4-8).
Undoubtedly, this procedure poses more risks due to longer surgical time, greater blood loss, more tissues exposed, communication between two cavities and participation of two surgical teams(8-10).
The combined surgery is initiated by gynecologists who make a midline infraumbilical incision (Figs. 1 & 2), through which the abdomen is widely exposed and intra-abdominal material is handled, with no contact and no trauma with the skin and subcutaneous tissue that will be preserved after abdominoplasty (Fig.3). The flap and the musculo-aponeurotic layer are not exposed. On conclusion of the intra-abdominal surgery, the plastic surgeons perform abdominoplasty using the incision indicated for each case. Flap undermining may be inferior, superior(11) or by block resection(3,9,12)(Fig. 4).
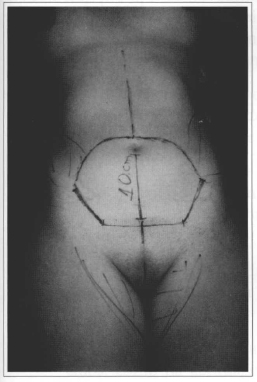
Fig. 1 - Marking the area to be excised in abdominoplasty and midline incision for gynecologic surgery.
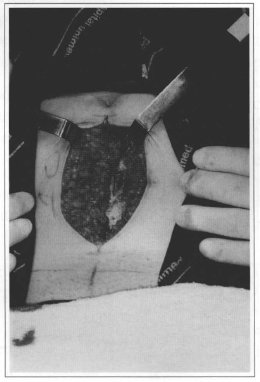
Fig. 2 - Midline incision in the abdominal wall to widely expose the area to gynecologists.
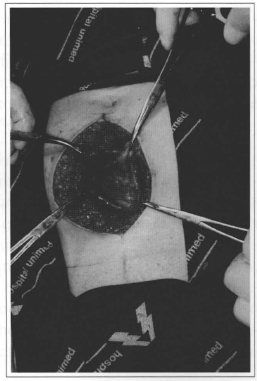
Fig. 3 - Contact with the intra-abdominal material, and skin and subcutaneous trauma, are restricted to the area to be resected.
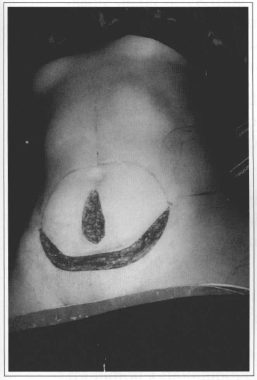
Fig. 4 - On conclusion of the gynecologic surgely, undermining is initiated by inferior or superior incision, or by block excision.
Some authors(1,2,5,7,8,12,13)favorable to this combination, provided some preoperative and transoperative care is taken, and they emphasize its advantages and the low number of complications.
Shull(8) and Voss(10) reported longer surgical time and length of stay, increased number of transfusions and complications, such as embolism, which could limit the combined procedure.
Savage(7) and Cosin(12) mentioned special care with obese patients and smokers and prophylaxis of venous thrombosis.
Castro(1,4), Gemperli(5), Perry(6) and Franco(13) described the initial approach by plastic surgeons, undermining up to the umbilicus and protecting the flaps with compresses. Next the intra-abdominal surgery begins, and is then followed by abdominoplasty.
Petrorius(3), Souza Pinto(9) and Cosin(12) described the previous block excision of skin and subcutaneous tissue, followed by intra-abdominal surgery, and posterior abdominoplasty.
Matthes(14) reported a case of endometrioma implantation in the horizontal scarring of abdominoplasty combined with hysterectomy.
PATIENTS AND METHODS
The study protocol encompassed the assessment of 51 patients submitted to abdominoplasty combined with intra-abdominal gynecologic surgery. The surgeries were performed by only one plastic surgeon and several gynecologic teams, from January 1997 to August 2002. Ages ranged from 27 to 67 years. The gynecologic procedures were hysterectomy in 36 patients (70.6%), tubal surgery in 14 (27.4%) and ovarian surgery in one patient (2.0%).
Routine preoperative tests were requested, as well as gynecologic and respiratory evaluations; patients were informed about the possibility of abdominoplasty not being performed in case of any event during gynecologic surgery.
The patients were kept in orthostatic position, and a line was previously marked in the suprapubic area, extending up to the anterior superior iliac spines, and another line connecting the latter and passing on the um bilicus, making an elliptic drawing (Fig. 1). The midline line between the umbilicus and the suprapubic area was drawn at the gynecologists' incision (Figs. 1 & 2). After exposing the abdomen and performing the appropriate treatment (Fig. 3), the wall was sutured up to the rectus abdominis muscles. At this point, any surgical material and drapes were changed and the team of plastic surgeons initiated their approach by making an incision in the inferior line (Fig.4) and undermining the flap (Fig. 5), suturing the aponeurosis with mononylon 2.0 (Fig. 6), isolating the umbilicus and completing the undermining up to the rib margin. Later, they performed plication of the rectus abdominis using mononylon 2.0; and prepared and fixed the umbilicus as reported by Juarez Avelar (15)(Fig. 7). Next, the excessive skin and subcutaneous tissue were resected, suction drainage placed in the incision, followed by skin and subcutaneous tissue suture in layers (Fig. 8).

Fig. 5 - Initiating undermining in the suprapubic line marking.
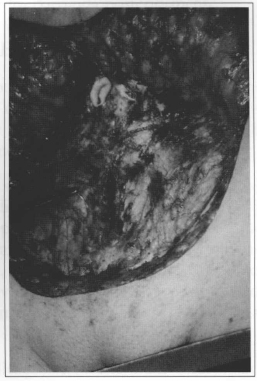
Fig. 6 - Suture of infraumbilical aponeurosis with nylon 2.0.
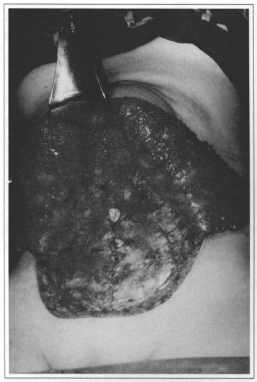
Fig. 7 - After undermining, plication of the recrus abdominis muscles and fixation of the umbilicus.
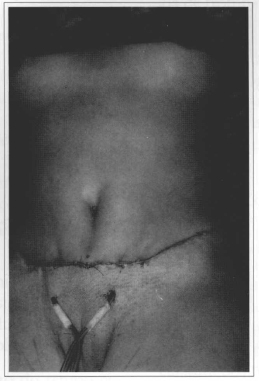
Fig. 8 - End of surgery with suction drainage placement.
Block anesthesia was performed in 43 (84.3%) patients, and general anesthesia, in 8 (15.7%). The patients ambulated within 24 to 36 hours and drainage tubes were removed within 48 hours. Forty-three (84.3%) patients were hospitalized for 48 hours and 8 (15.7%) for 72 hours. Forty (78.4%) women were prescribed antibiotic therapy by gynecologists for 24 hours, and 11 (21.6%) for longer than 24 hours. The combined surgery time was 2 to 3 hours in 16 (31.3%) patients, 3 to 4 hours in 26 (50.9%), and 4 to 5 hours in 9 (17.8%) patients.
One (1.9%) case resulted in an inverted T-scar and two (3.9%) patients had a small vertical suprapubic scar.
RESULTS
The resulting scar was horizontal in 50 (98.0%) patients. Only one woman (2.0%) presented an inverted T-scar due to a previous vertical scar.
Two (3.9%) patients had seroma, one of whom (1.9%) diabetic; she progressed with infection due to Escherichia coli, and was treated with drainage and antibiotics with satisfactory results.
Two (3.9%) patients presented epidermolysis in a small vertical suprapubic scar and two women had hematoma; one of the collections drained spontaneously through this small scar.
Only one (1.9%) patient required blood transfusion; she had a vesicovaginal fistula in the postoperative period, was submitted to another surgery one month later and recovered satisfactorily.
All 51 patients subrnitted to abdominoplasty combined with intra-abdominal gynecologic surgery were anatomically and emotionally satisfied (Figs. 9-12).
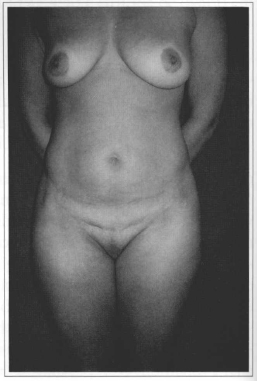
Fig. 9 - Preoperative period: abdominoplasty and hysterectomy. Frontal view.
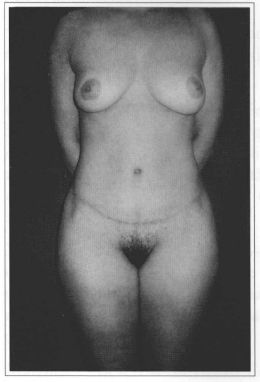
Fig. 10 - Five-month postoperative period.
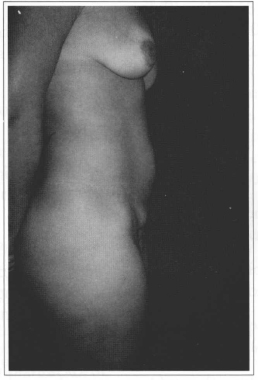
Fig. 11 - Preoperative period, lateral view.
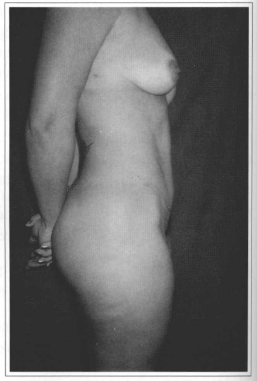
Fig. 12 - Five-month postoperative period.
COMMENTS
The association of abdominoplasty and gynecologic surgery has been required by patients for solving aesthetic and organic problems in only one surgical procedure.
Preoperative care, such as restricting smoking, gynecologic and angiologic evaluation, and respiratory physiotherapy, if necessary, are relevant to prevent complications. Patients may be informed about the possibility of not performing abdominoplasty due to any significant event during gynecologic surgery.
The separate approach performed by gynecologists using a midline infraumbilical incision has the following advantages:
• It widely exposes the abdomen, resulting in a shorter length of the gynecologic surgery.
• No incision on aponeurosis and muscles, as in the Pffannenstiel incision.
• Less likelihood of contamination and implantation of ectopic tissues in the abdominal wall, as in endometriosis, since there is no contact of the material in the abdomen with the preserved tissues.
• Less subcutaneous tissue and aponeurosis are exposed, and fluid and blood losses decrease, due to no previous flap undermining.
• Plastic surgeons may initiate undermining through an inferior or superior incision, or they may perform a block resection of the flap (Fig. 4).
• Each surgical team performs on their turn, leading to reduced costs.
• If the course of the gynecologic surgery contraindicates abdominoplasty, unnecessary undermining is avoided.
Prophylactic antibiotic therapy is prescribed in ali cases; some patients took it longer than 24 hours according to the gynecologist's recommendations. Surgical time of both procedures was in most cases (82.2%) less than four hours. Less tissues exposed and decreased fluid and blood loss, combined with strict hemostasia, prevented an increase in morbidity and need for blood transfusion.
Active and constant mobilization of limbs in the immediate postoperative period and ambulation within 24 to 36 hours was aimed at prophylaxis of deep venous thrombosis and pulmonary embolism, and led to a shorter hospital stay, that is, 48 hours in 8.3% of the cases, and 72 hours, in 15.6%.
As to complications, two patients presented seroma, and one of them was diabetic. She progressed with infection due to Escherichia coli, which solved by draining through the scar and specific antibiotic therapy. Another patient had spontaneous drainage of a hematoma through a small vertical suprapubic scar, resulting in epidermolysis of this segment, which was further re-sutured. In another case of epidermolysis, it healed by secondary intention and was later submitted to aesthetical repair.
Only one patient required blood transfusion; she developed a vesicovaginal fistula, which was later repaired.
CONCLUSIONS
The association of abdominoplasty with intra-abdominal gynecologic surgery has not led to increased morbidity or mortality rates when appropriate pre-, trans- and postoperative care is provided to patients.
The separate approach by gynecologists and plastic surgeons reduces trauma in the preserved tissues, fluid and blood loss, possible contact of the intra-abdominal material with the abdominal wall and trauma in the musculo-aponeurotic system; moreover, it avoids unnecessary flap undermining in the cases in which abdominoplasty can not be performed.
The few complications observed did not interfere in the aesthetic results or patient satisfaction.
ACKNOWLEDGEMENTS
We would like to thank Dr. Talita Franco, Head Professor of Plastic Surgery at the Universidade Federal do Rio de Janeiro, for guiding this study.
REFERENCES
1. Castro CC, Salema R, Aboudib Jr JH, Braga L. Análise da associação entre abdominoplastia e cirurgias ginecológicas. J Bras Gin. 1991; 101(10):447-9.
2. Porchat CA. Estudo comparativo da evolução pósoperatória de pacientes submetidos a abdominoplastia isolada e combinada a outras cirurgias do abdômen. Tese de Mestrado, Fac. Méd. U.F.R.J., Rio de Janeiro, 2000.
3. Pretorios RG, Matory Jr WE, LaFontaine D. Management of massive ovariun tumors. Surg Ginecol Obstet. 1989; 169(6):532-6.
4. Castro Cc. Estudo da associação cirúrgica da plástica de abdome com procedimentos ginecológicos. J Bras Gin. 1977; 83(3):137-42.
5. Gemperli R, Neves RI, Tuma P, Bonamichi GT, Manders EK. Abdominoplasty combined with other intra-abdominal procedures. Ann Plast Surg.1992; 29(1):18-22.
6. Perry AW Abdominoplasty combined with total histerectomy. Ann Plast Surg. 1986; 16(2):121-2.
7. Savage RC. Abdominoplasty combined with other surgical procedures. Plast Reconstr Surg.1982;70( 4) :437-43.
8. Shull BL, Verheyden CN. Combined plastic and ginecological surgical procedures. Ann Plast Surg. 1988; 20(6):552-7.
9. Souza Pinto EB, Almeida AEF, Reyes MFC. Abdominoplastia com cirurgia da' cavidade. Anais do Simpósio Brasileiro de Abdominoplastia.- SBCP; São Paulo, Brasil. 1982.
10. Voss SC, Sharp HC, Scott JR. Abdominoplasty combined with gynecological surgical procedures. Obstet Gynecol. 1986.; 67(2):181-5.
11. Sinder R. Cirurgia plástica do abdome. Rio de Janeiro, Brasil, 1979.
12. Cosin A, Powell JL, Donovan JT, Srueber K. The safety and efficacy of extensive abdominal panniculectomy at the time of pelvic surgery. Gyneco Oncol. 1994; 55:36-40.
13. Franco T. A associação de abdominoplastia a cirurgias intracavitárias. Rev Bras Ciro 1971; 61:5- 17.
14. Matthes G, Zabel DD, Nastala CL, Shestak KC. Endometrioma of the abdominal wall following combined abdominoplasty and histerectomy: case report and review of the literarure. Ann Plast Surg. 1998; 40(6):672-5.
15. Avelar J. Cicatriz umbilical- da sua importância e técnica de confecção nas abdominoplastias. Rev Bras Cir. 1979; 69:41-52.
I - Senior Member of the Sociedade Brasileira de Cirurgia Plástica (SBCP). Senior Member of the Colégio Brasileiro de Cirurgiões. Master's degree in Plastic Surgery - Universidade Federal do Rio de Janeiro.
II - Senior Member of the SBCP. Senior Member of the Colégio Brasileiro de Cirurgiões.
III - Member of the SBCP.
Study performed at Santa Teresa and Beneficência Portuguesa Hospitals - Petrópolis, RJ
Address for correspondence :
João Medeiros Tavares Filho, MD
R. Buenos Aires, 255 2
5610-140 - Petrópolis - RJ Brazil
Phone/fax: (55 24) 2243-8033
e-mail: jmedeiro@compuland.com.br


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter