

Original Article - Year 2015 - Volume 30 - Issue 4
Hair transplant of follicular units: a 15-case experience
Transplante capilar de unidades foliculares: experiência de 15 casos
ABSTRACT
INTRODUCTION: The transplant of follicular units (FUs) for hair restoration yields the most natural results. The implantation of 20-25 FU/cm2 has a low risk of follicular damage and yields satisfactory results within two sessions. A density greater than 30-35 FU/cm2 yields the same results within a single session but increases the risk of follicular damage and hair growth loss. We report our experience with 15 cases of hair transplantation, with an implantation density of > 30 FU/cm2 and with incisions made previously using a surgical instrument modified to facilitate implantation.
METHOD: A retrospective study of 15 patients who consecutively underwent 17 surgeries between July 2008 and June 2012 and were followed up for 1 year.
RESULTS: A mean of 1433.3 FUs and 3019.8 hairs were implanted per surgery. The mean surgical duration was 10 hours and 23 minutes. Satisfactory hair growth occurred, and results were visible at 6 months onward with few complications. Of the 15 patients, two required a second session.
CONCLUSIONS: The technique used here enabled delicate manipulation of the FUs and high-density implantation that achieved good results within one session but required an above-average execution time and should be restricted to small areas requiring greater density.
Keywords: Hair follicle; Transplantation; Alopecia; Hair transplantation.
RESUMO
INTRODUÇÃO: O transplante capilar de unidades foliculares (UFs) é a técnica que permite a obtenção dos resultados mais naturais. A implantação de 20 a 25 UF/cm2 possui baixo risco de dano aos folículos e tem resultado satisfatório com duas sessões. Densidade superior a 30-35 UF/cm2 permite resultado com uma única sessão, mas aumenta os riscos de dano ao folículo e perda de crescimento dos fios. O objetivo do estudo foi relatar a experiência de 15 casos de transplante capilar com implantação de 30 ou mais UF/cm2, com incisões previamente realizadas e utilizando um instrumento cirúrgico modificado para facilitar a implantação.
MÉTODO: Foi realizado estudo retrospectivo de 15 pacientes submetidos em sequência a um total de 17 cirurgias, no período de julho de 2008 a junho de 2012, com tempo de seguimento de 1 ano.
RESULTADOS: Foi implantada uma quantidade média de 1433,3 UF e 3019,8 fios por cirurgia. O tempo médio de duração das cirurgias foi de 10 horas e 23 minutos. Ocorreu crescimento satisfatório dos fios com resultado visível a partir de 6 meses, com poucas complicações. Dos 15 pacientes, dois necessitaram de uma segunda sessão.
CONCLUSÕES: A técnica empregada possibilitou manipulação delicada das UFs e permitiu implantação com alta densidade, obtendo bom resultado com uma sessão, mas requer tempo de execução acima da média, devendo ter uso restrito a áreas pequenas com necessidade de maior densidade.
Palavras-chave: Folículo piloso/Transplante; Alopecia; Cabelo/ Transplante.
Androgenetic alopecia is characterized by progressive miniaturization of the hair follicle with increasingly less length and thickness growth in each growth cycle, causing a shortening of the anagen stage, which in turn leads to hair follicle atrophy and alopecia. Miniaturization is due to the effect of dihydrotestosterone on the androgen receptors that are present within the follicles1. If miniaturization is mild or moderate, the progression of alopecia with clinical treatment can be slowed down with finasteride and minoxidil1. At the advanced stage of follicle atrophy, surgical treatment is necessary.
In men, androgenetic alopecia can affect the frontal, parietal, and vertex regions of the scalp owing to the higher concentration of androgen receptors at these sites2, while no effect is seen on the occipital and temporal regions. Follicles moved from the posterior regions to those affected by alopecia grow normally. This phenomenon was discovered by Orentreich in the 1950s3, which paved the way for hair transplantation. The first hair transplant surgery consisted of graft punches removed from the occipital region and implanted into the balding area. Since then, hair transplant surgery has been modified and improved, showing better and more natural results. Currently, transplant of follicular units (FUs) is performed, as it offers the most natural results and better usage of the donor area follicles4-7.
The FUs are the natural pattern of hair presentation because the hairs emerge from the scalp follicles in groups of one to five hairs, the majority (80%)8 including two to three hairs; all follicles include a sebaceous gland, arrector pili muscles, and one to five (usually one to three) hairs surrounded by a connective tissue sheath called the perifolliculum8. The implantation of 20-25 FU/cm2 has a low risk of follicular damage and high satisfaction results regarding density as well as a natural appearance within two sessions6. An implantation density > 30-35 FU/cm2 enables good results in a single session but increases the risk of follicular damage and hair growth loss6,9.
OBJECTIVE
The objective of the study is to report the initial experience of 15 cases of FU hair transplantation with an implantation density > 30 FU/cm2 in selected areas using incisions previously made with a modified surgical instrument for facilitating graft implantation with minor trauma.
METHOD
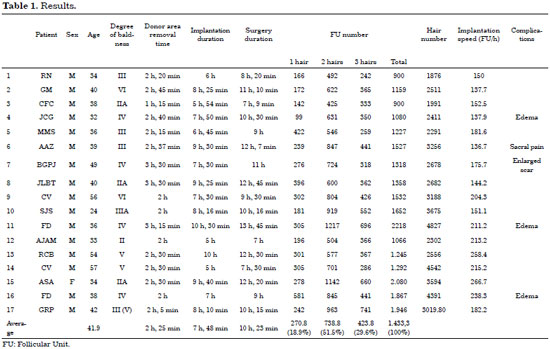
This is a retrospective study of 15 patients (mean age, 41.9 years) who underwent 17 surgeries between July 2008 and June 2012. The 14 male patients had Hamilton/Norwood androgenetic alopecia degrees of IIVI (Table 1). The one female patient had a high forehead that resulted from a previous coronal rhytidectomy. One of the patients had controlled light systemic arterial hypertension, whereas the others had no associated diseases. The surgeries were performed under local anesthesia with sedation by an anesthesiologist. The follow-up period was 1-2 years.
Surgical technique
With the patient in the prone position, a portion of skin approximately 1-cm wide was removed from the occipital region and extended to the temporal region. Hair scraping was not performed. After antisepsis, the dermis was infiltrated with a solution containing lidocaine, bupivacaine, and epinephrine 1:100,000, followed by tumescent infiltration with saline solution to remove the follicles and neurovascular bundles and facilitate dissection. From start to finish, the surgery was performed using a magnifying glass with a magnification of 3.5×. The dermis was incised around the hair without delving into the subcutaneous tissue using a #15 scalpel. Gentle traction was created by two simple hooks in the incision edges to remove and separate the follicles present on each edge and avoid their transection.
With the follicles removed, the dissection was continued on the plane below the bulbs with the aim of preserving the subcutaneous tissue layer on the galea and avoiding injury of the sensory and vascular branches until the skin strip was completely removed. Electrocautery was not used to avoid follicular damage. The incision was closed without tension with little to no detachment of the edges using a trichophytic suture, which removes a 1-2-mm strip of the dermal edge of the cranial edge of the scalp, and the following edge flow margin was sutured over the de-epidermized edge with continuous stitches using 3-0 nylon sutures. The follicles present in the de-epidermized edge grow through the scar tissue to cover the scar with hair. Using a stereoscopic microscope, dissection of the skin strip was performed by extracting transverse slices with a width corresponding to the FU layer in a procedure called slivering. These skin slices were subsequently split with FU separation, which were kept in containers with cold saline solution. The hairs present in the FUs were at least 2 cm long.
After donor area closure, the patient was placed in a supine position, with back and head elevation, and antisepsis was performed, followed by infiltration of the receiving area with an anesthetic solution. The incisions were then made in the recipient areas: 21G (25 × 8) hypodermic needles were used to create the incisions that would receive grafts of one or two hairs, whereas 19G (25 × 10) hypodermic needles were used to create incisions in the areas that would receive three or four hairs.
Before the incisions were made, a tumescent saline infiltration of was performed below the dermis to enlarge the area of the exposed surface and increase the distance to the galea and vascular branches present in the subcutaneous tissue. The objective was to distribute 25-35 incisions/cm2 at the outermost track of areas receiving an FU graft of one to two hairs; 35-40 incisions/cm2 in a 2-cm strip immediately after intended to 2-hair slips; 30-35 incisions/cm2 at the central area for receiving a FU containing three hairs; and 15-25 incisions/cm2 in peripheral areas in cases of more advanced alopecia. The needle insertion angle matched that of the hair, even atrophic, on site, or nearby.
To assist the FU implantation, the tip of the fat grafting cannula was modified to a 1.2-mm outside diameter by removing a segment of approximately 50% of the cross-wall section, obtaining a blunt tip, and creating a lateral opening (Figure 1). To implant the graft, the surgeon used the left hand to open the chosen hole and expand it with the cannula and used the right hand to insert the graft with microsurgery tweezers between the opening of the cannula and the edge of the incision, sliding to the bottom. At the end of the surgery, the scalp was covered with a surgical cap without the need for healing. The stitches were removed after 10-14 days.

Figure 1. A, modified cannula. B, surgical appearance. C, one-, two-, and three-hair follicle units. D, scar at six months. FU: Follicular Unit.
RESULTS
At the beginning of the series, nine to ten 1-cm strips of skin were removed. The dimensions increased to 30 × 1 cm at the end. The number of FUs was 900-2218, totaling 1876-4827 hairs (mean 1433.3 FUs and 3019.8 hairs). More than half of the FUs (51.5%) had two hairs, followed by FUs with three hairs (29.6%) and those with one hair (18.9%). The areas had a mean 2.1 wires. The mean surgical duration was 10 hours and 23 minutes, the average donor area removal time was 2 hours and 25 minutes, and the mean implantation time was 7 hours and 48 minutes. The average implantation speed plus time to perform the preliminary incisions and implantation time was 182.3 FUs/hour (Table 1).
Hair growth occurred between the end of the second and during the third postoperative month. Increased thickness and growth were noted in the fourth to sixth postoperative months. Results were first visible at 6 months and growth was complete within 1 year. Good density and hair distribution with a natural integration with the neighboring hair was obtained with a single surgery session (Figures 2-6). In two cases, a second session was required.

Figure 2. A 39-year-old man with grade III alopecia underwent a single hair transplant session of 1527 follicle units. A, before transplant. B, 3 days after transplant. C, 7 months after transplant. D, 1 year after transplant. FU: Follicular Unit.

Figure 3. A 38-year-old man with alopecia of degree IIA underwent a single hair transplant session of 900 follicle units. A and B, before transplant. C and D, 1 year after transplant. FU: Follicular Unit.

Figure 4. Male patient, 38 years old, with degree IIA alopecia underwent a single hair transplant session of 900 follicle units. A and B, before transplant. C and D, 1 year after transplant. FU: Follicular Unit.
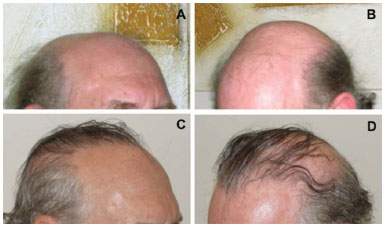
Figure 5. A 56-year-old man with degree VI alopecia underwent two hair transplant sessions of a total of 2824 follicle units. A and B, before transplant. C and D, 9 months after transplant (after the second session). FU: Follicular Unit.
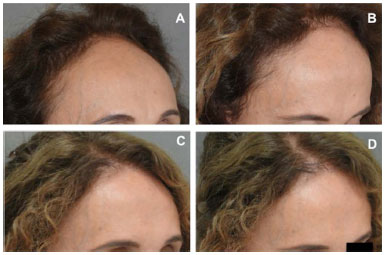
Figure 6. A 54-year-old woman with a high forehead after coronal rhytidectomy underwent a single hair transplant session of 2080 follicle units. A and B, preoperative. C and D, 1 year postoperative. FU: Follicular Unit.
Regarding surgical complications, three cases of intense frontal edema occurred on the second postsurgical day and completely regressed with cold compresses until the seventh postoperative day. In another case, there was pain in the sacral region due to prolonged bed positioning that improved with analgesics and massage and improved completely after the first postsurgical week. The addition of an egg box foam mattress prevented the recurrence of this problem. Three patients with oily hair had mild seborrheic dermatitis within 1-2 weeks after the postoperative period, which improved with the use of shampoo for oily hair. Small cysts (milia) and folliculitis were seen in patients with oily hair, but they improved with puncture and drainage. One patient had enlargement of one side of the lateral edge of the scar from the donor area after the second session. The others showed no scar enlargement or hypertrophy. There were no cases of reduction or loss of skin sensitivity.
DISCUSSION
The average FU density in Caucasian men is estimated at 100 FU/cm2 or 200 hairs/cm2 (130-280 hairs/cm2)6,10. In non-Caucasians, the density is lower6. There would be no need for hair transplant if > 50% of the natural density is maintained6,7, as density loss is not apparent even when there is a reduction of up to 50% of the natural density9. Thus, hair transplantation in a Caucasian man requires approximately 33 FUs of three hairs or 50 FUs of two hairs to reach a normal density of 100 hairs/cm2. A density of 20-25 FU/cm2 is considered safe since the graft survives even when used in large areas and achieves good results in two sessions6. Density greater > 30-35 FU/cm2 is considered high (dense packing9) and is not recommended for routine use in large areas6.
Surgery using a combination of dense packing in selected areas and conventional density of 20-25 FU/cm2 in the remaining areas achieves satisfactory appearance and density results in one session, reducing the need for a second session. It is important that surgeons save any extra follicles from the donor area because every time a skin strip is removed, some follicles are transected and fibrosis in later surgery will increase the chances of transection6; moreover, when the best result is achieved in a single session, the rate of patient dissatisfaction decreases6.
In this study, in the less extensive alopecia of grade II-III, high-density FUs were used throughout the implanted areas. In the case of the most extensive alopecia, the grafts were distributed according to the recommendation of prioritizing higher densities in the central region of the forehead and in 2-3-cm strips posterior to the area 1-1.5 cm from the beginning of the forehead7.
The use of densities > 20-25 FU/cm2 requires incisions shorter than 1.2 mm6 to prevent compromising of the vascularity of the receiving area as well as careful handling of the graft during implantation to prevent injury by transecting the follicle or crushing the hair bulb by compression4,6,11,12. These risks are even greater in dense packing9. One way to implement dense packing is to infiltrate the receiving area with saline, which causes swelling and surface expansion to allow for a greater number of incisions. When the edema disappears, there is an increased density of incisions/cm2; at densities > 30-35 FU/cm2, the incisions should not be larger than those performed using a 19G needle (1.0-mm diameter)6,11. Previously made incisions have another advantage: reduced bleeding during graft implantation, as at that time, the incisions will already have coagulated, allowing for good incision visibility and a cleaner field6; there is also a lower chance of expelling a contiguous graft from the incision.
Regarding implantation, the recommended way to handle the FU graft is by the deepest part of the connective or subcutaneous tissue around the bulb without touching the bulb; however, if there is little tissue around the bulb, the bulb should be held loosely12. The graft, secured by the tweezers, is then "pulled" by the tip of the forceps into the incision. Holding the FU by the most superficial part is not recommended, as it will be "pushed" into the incision and, due to its flexibility, can undergo torsion and compression against the wall of the tunnel created by the incision12.
During the surgery, however, FU grafts with two to three hairs often do not have sufficient firm tissue around all of the present bulbs, leading to one or two twisted bulbs during implantation that may require direct bulb holding, causing its compression. Bleeding upon reaching a blood vessel during incision or implantation is common; it severely reduces visibility; these conditions increase the chances of compressing or twisting the follicle during implantation attempts. Traumatic manipulation may occur in a significant amount of grafts, which reduces their survival and growth. This led us to search for alternatives to reduce the trauma associated with graft introductions during implantation.
One technique facilitates the placement of grafts on previously made incisions. This is based on reopening the incision with a blunt-tip needle with one's non-dominant hand, creating space for the passage of the graft, which is placed with the other hand under less pressure and strength11. These needles were not commercially available in Brazil, so a 1-mm fat grafting cannula with a 1.2-mm outside diameter equivalent to an 18G needle was used to reopen the incisions. The modification creating the lateral opening in the tip of the cannula that provided access to the lumen of the cannula added extra space for the passage of the grafts, making it possible in this study to position FU grafts of two to three hairs into incisions created with 21G and 19G needles, respectively, more easily than directly through the incision. It was also possible to hold the dermis by less bulky grafts away from the bulb and slip through the interior of the cannula without risking graft twisting while minimizing trauma applied to the graft.
Another important factor of FU graft survival is the time the grafts remain outside the body since the removal of donor area to implantation on the receiving area should be limited to 6 hours12,13, beyond which FU graft viability can decreased. In one study, the survival rate of the grafts was 92% in 6 hours, with loss of 1% from each hour after that (90% in 8 hours)4,12. In this study, the mean graft implantation time of 7 hours and 48 minutes was almost 2 hours beyond the 6-hour limit. There were factors that increased the surgical time, such as the use of high-density grafts, which require more implantation time9,14, and the use of UF with long wires, which increases both donor area removal time and implantation time13. The late results of surgery, compared with the immediate result observed with long strands, suggested no apparent or significant impairment in hair growth (Figure 2).
Of the 15 cases, one requested a second session to enlarge the implantation coverage area; another presented with alopecia progression and miniaturization of hair in the middle of the previous graft as well as density loss for which a second session was conducted to increase density. The rest were satisfied with single-session treatment and given the option of a second session but preferred to postpone it to when the alopecia progressed, if at all. The complications that occurred were moderate and corrected with local care, except for the localized scar enlargement that required with an outpatient surgery. The observed average of 2.1 hairs per FU, with most of the FUs containing two hairs, is quite close to the 2.2-2.3 hairs/FU reported in the literature6,8. It was also observed that there was an increase of about 75% in the implantation speed of the initial cases (150 FU/h and 137.7 FU/h in procedures 1 and 2) compared to the final ones (266.7 FU/h and 238.3 FU/h in procedures 16 and 17), showing the learning curve of the technique.
An FU hair transplant is laborious and time consuming4 and requires specific training. One author claimed that approximately 18 months of constant supervised practice was necessary to train an assistant to implant FUs with a high density in a clinic that specialized in hair transplantations14. Regarding the number of required members, one author stated that it took 6-7 hours to deploy 1500-2000 FUs with a team of 8-10 assistants15 (not counting the surgeon); inexperienced surgeons commonly require 8-10 hours12. In this study, the surgical team consisted of a surgeon (the author) and four assistants for the graft dissections. A large staff and greater number of performed surgeries contribute to reduced operating time.
CONCLUSIONS
FU hair transplant using the technique described in this study increase the finesse in handling the FUs, allowing high-density implantation and reducing the likelihood of follicle twisting or compression with satisfactory results for up to 1 year. However, the surgery time was considered high as it exceeded the recommended limit of 6 hours for FU dissection and implantation. These findings may indicate that restricted or small areas require higher FU density while wider areas require other techniques.
REFERENCES
1. Haber RS. Pathogenesis and medical therapy of male and female pattern hair loss. In: Haber RS, Stough DB, eds. Hair Transplantation. Philadelphia: Elsevier Saunders; 2006. p.1-7.
2. Hibberts NA, Howell AE, Randall VA. Balding hair follicle dermal papilla cells contain higher levels of androgen receptors than those from non-balding scalp. J Endocrinol. 1998;156(1):59-65. PMID: 9496234 DOI: http://dx.doi.org/10.1677/joe.0.1560059
3. Unger W. The history of hair transplantation. Dermatol Surg. 2000;26(3):181-9. DOI: http://dx.doi.org/10.1046/j.1524-4725.2000.00503.x
4. Limmer BL. The history of the follicular unit micrografting technique: a personal view. In: Unger WP, Shapiro R, eds. Hair Transplantation. 4th ed. New York: Marcel Dekker; 2004. p.383-88.
5. Bernstein RM, Rassman WR. The rationale for follicular unit transplantation. In: Unger WP, Shapiro R, eds. Hair Transplantation. 4th ed. New York: Marcel Dekker; 2004. p.388-407.
6. Bernstein RM, Rassman WR. Follicular unit transplantation: 2005. Dermatol Clin. 2005;23(3):393-414. DOI: http://dx.doi.org/10.1016/j.det.2005.04.002
7. Shapiro R. Follicular units transplantation alone or follicular units with multi-FU grafts: why, when and how? In: Unger WP, Shapiro R, eds. Hair Transplantation. 4th ed. New York: Marcel Dekker; 2004. p.415-68.
8. Jimenez F, Poblet E. Gross and microscopic anatomy of the follicular unit. In: Haber RS, Stough DB, eds. Hair Transplantation. Amsterdam: Elsevier Saunders; 2006. p.35-42.
9. Dense packing techniques. Seager D. In: Haber RS, Stough DB, eds. Hair Transplantation. Philadelphia: Elsevier Saunders; 2006. p.127-31.
10. Marritt E. The death of the density debate. Dermatol Surg. 1999;25(8):654-60. DOI: http://dx.doi.org/10.1046/j.1524-4725.1999.99067.x
11. Cooley J. Achieving optimal growth. In: Haber RS, Stough DB, eds. Hair Transplantation. Philadelphia: Elsevier Saunders; 2006. p.111-6.
12. Shapiro R. Graft insertion and placement. In: Unger WP, Shapiro R, eds. Hair Transplantation. 4th ed. New York: Marcel Dekker; 2004. p.533-9.
13. Crisóstomo MR, Lopes AAO, Crisóstomo MGR, Cavalcanti DC, Benevides AN. Comparação entre a técnica clássica de transplante de unidades foliculares e o transplante de fios longos (preview long hair). Rev Bras Cir Plást. 2010;25(1):117-26.
14. Seager DJ. Pitfalls of follicular unit hair transplantation and how to avoid them. In: Unger WP, Shapiro R, eds. Hair Transplantation. 4th ed. New York: Marcel Dekker; 2004. p.408-18.
15. Unger W. Why "mixed" grafting follicular units and multi-follicular unit grafts. In: Unger WP, Shapiro R, eds. Hair Transplantation. 4th ed. New York: Marcel Dekker; 2004. p.475-418-503.
Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
Institution: Clínica Fabio Carramaschi, São Paulo, SP, Brazil.
Corresponding author:
Lúcio Issamu Nakayama
Rua Dr. Eduardo de Souza Aranha, 387, Jd. Paulista
São Paulo, SP, Brazil Zip Code 04543-121
E-mail: lucionakayama@uol.com.br
Article received: July 31, 2013.
Article accepted: February 4, 2014.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter