

Ideas and Innovation - Year 2015 - Volume 30 -
Prototyping: applications in craniomaxillofacial surgery at the Brazilian National Institute of Traumatology and Orthopedics (INTO)-RJ
Prototipagem: aplicações na cirurgia crâniomaxilo- facial do Instituto Nacional de Traumatologia e Ortopedia (INTO)- RJ
ABSTRACT
Prototyping is a process of construction in order to obtain physical prototypes from 3D digital models. The introduction of prototyping in medicine is a recent event. Case 1: An 18-year-old patient with a 192 cm2 cranial defect secondary to a decompressive craniectomy. A cranioplasty was performed using a customized prosthesis manufactured by prototyping. Case 2: A 34-year-old patient with a panfacial fracture sequelae. This patient had a relevant defect in the zygomatico-orbital complex, with great zygoma dislocation. Surgical planning was performed using the prototype, which was taken to the surgery room to support the surgery. Case 3: A 29-year-old patient with a mandibular ameloblastoma from the subcondylar region to the right parasymphysis. Prototyping of the craniofacial skeleton and fibula were carried out in addition to a model surgery that was performed on the previous day. Discussion: Prototyping can be applied to craniofacial surgery in many ways, such as customized prosthesis manufacturing, surgical planning, and education of residents and patients. In case 1, a customized prosthesis had the advantage of not requiring a donor area and resulted in excellent esthetic results. In case 2, the presence of the prototype during surgery helped identify the zygoma more quickly in order to reposition it. In case 3, the model surgery helped decrease morbidity of the donor area, define fibular osteotomy and the resection margins, mold the plate, select the screws, ensure the condylar prosthesis fit in the temporomandibular joint (TMJ ), achieve the best occlusion possible, and reduce the surgical time, anesthesia, and hospital-associated costs.
Keywords: Three-dimensional printing; Craniotomy; Injuries and lesions/complications; Mandible/abnormalities.
RESUMO
A prototipagem é um processo de construção para obter protótipos físicos a partir de modelos 3D digitais. A introdução da prototipagem na medicina é recente. Caso1 - Paciente de 18 anos portador de defeito craniano de 192 cm2 secundário a uma craniotomia descompressiva. Foi feita uma cranioplastia com prótese customizada confeccionada a partir da prototipagem. Caso 2 - Paciente de 34 anos portador de sequela de fratura panfacial. Apresentava importante defeito do complexo zigomático-orbitário, com grande deslocamento do zigoma. O plano cirúrgico foi feito com o protótipo; e o protótipo foi levado à sala de cirurgia para auxiliar o ato operatório. Caso 3 - Paciente 29 anos portadora de um ameloblastoma de mandíbula da região subcondilar até parassínfise direita. Foi feita a prototipagem do esqueleto craniofacial e fíbula, e uma cirurgia de modelo 1 dia antes. Discussão: A prototipagem pode ter aplicação na cirurgia craniofacial de várias maneiras: confecção de próteses customizadas, planejamento cirúrgico e educação dos residentes e pacientes. No caso 1, a prótese customizada tem como vantagens a ausência de área doadora e o excelente resultado estético. No caso 2, a presença do protótipo na sala de cirurgia ajudou a identificar com mais rapidez o zigoma para resposicioná-lo. No caso 3, a cirurgia de modelo diminuiu a morbidade da área doadora; definiu a osteotomia da fíbula e as margens de ressecção; moldou a placa; escolheu os parafusos; encaixou a prótese de côndilo na ATM; alcançou a melhor oclusão possível; e diminuiu tempo cirúrgico, anestesia, e custo hospitalar.
Palavras-chave: Impressão tridimensional; Craniotomia; Ferimentos e lesões/complicações; Mandíbula/anormalidades.
Prototyping is a process of construction in order to obtain physical prototypes from 3D digital models. Prototyping systems were developed more than 30 years ago, and prototypes are manufactured by adding fine layers of specific materials (such as plastics, ceramics, metals, and paper)1-3. Models of virtual objects are quickly and accurately transformed into physical models of these objects4. These virtual objects may be created by design software, which are downloaded from specific sites on the internet or scanned from a pre-existing object. Prototyping was initially used in the automobile and aeronautical industries; however, currently it is used in many other areas5-7.
The introduction of prototyping in medicine is a relatively recent event. With the technological advances of radiology (computerized tomography [CT] and magnetic nuclear resonance-[MNR]), high-definition images can be generated, allowing a detailed 3D view and analysis of anatomical structures8. From these images, a digital printer can create a 3D model of the anatomical structure under study9.
More recently, the combination of scanning technology with prototyping technology became possible through smartphone applications. Thus, it is already possible to scan objects using smartphones, to send the threedimensional attachment to a 3D printer through Wi-Fi and print objects in the form of the scanned model10.
This work aimed to present examples of prototyping uses in craniomaxillofacial surgery and to discuss its benefits in surgical planning, the education of residents, clarifying patient doubts and in customized prosthesis manufacturing.
CASE SERIES
This work presents three distinct cases carried out in 2013, for which the craniomaxillofacial surgical team at the Brazilian National Institute of Traumatology and Orthopedics (INTO)-RJ decided, in their weekly clinical meeting, to use prototyping as part of the treatment for these patients. Case 1 presented with a full-thickness cranial defect and its prototyping and customized prosthesis were performed by the EincoBio® company. Cases 2 and 3 presented with panfacial fracture sequelae and a mandible tumor, respectively, and their prototypes were manufactured by the Centro de Tecnologia da Informação Renato Archer (Renato Archer Information Technology Center).
All prototypes were manufactured free of charge. EincoBio® donated the cranial prosthesis, and the CTI Renato Archer has an agreement with the patients from the Brazilian Unified Health System (SUS). The benefits and possible disadvantages of using the prototyping were observed and discussed by the team based on the literature available on the topic.
Case 1
An 18-year-old patient presented with a full-thickness 192 cm2 frontal-parietal-temporal cranial defect secondary to a decompressive craniectomy due to a motorcycle accident 1 year ago (Figure 1). We chose to perform the incision in the previous scar left by the neurosurgeon, in a hemicoronal access. After finding the bone plane peri-defect, we entered in a plane exactly supra dura-mater, fully exposing the defect and leaving a good cover of the soft parts above. Subsequently, the borders of the defect were reopened using a drill, a suspension point in the dura-mater was conducted, and the customized prosthesis fit perfectly and was fixed with a plate and screws (Figures 2 and 3). There were no complications and the patient progressed well (Figures 4 and 5). In this case, the prototyping was performed by Eincobio®, where the prototype for this defect was made, which was used for the manufacture and fitting tests of the customized prosthesis.
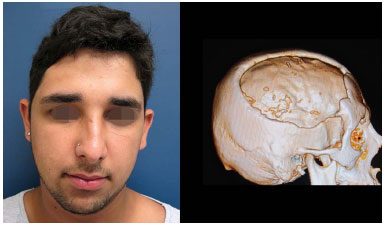
Figure 1. An 18-year-old patient with a 192 cm2 cranial defect due to decompressive craniectomy sequelae.
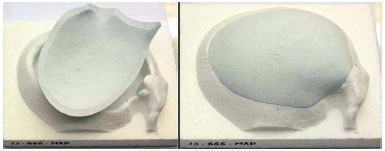
Figure 2. Prototyping of the skull and defect through CT and design of the prosthesis that perfectly fits in the defect.
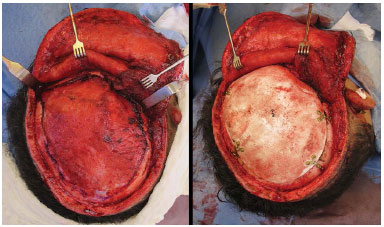
Figure 3. Defect exposed with reopened borders and prosthesis fixed in the defect.
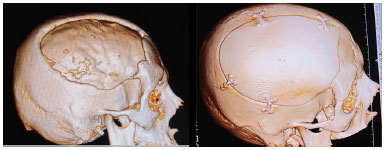
Figure 4. Pre and postoperative CT with the prosthesis reconstructing the cranial defect.

Figure 5. Preoperative and 11th month postoperative cranioplasty with prosthesis.
Case 2
A 34- year-old patient presented with a panfacial fracture sequelae due to a motorcycle accident 3 years ago (Figure 6). The patient presented with relevant dislocation of the zygomatic bone, absence of a floor, lower ridge, lateral wall, and lateral ridge of the orbit and right anophthalmic cavity. A bicoronal access was performed and the skull and middle third of the right hemiface were fully exposed. The surgical planning had already been performed with the prototype in a clinical meeting, and the prototype was taken to the surgery room to support the surgery. The zygoma was repositioned and fixed in the zygomatic arch and frontal zygomatic suture using plates and screws, and we obtained a parietal external bone graft and, with this bone, the lower and superolateral orbital borders were reconstructed (Figure 7). There were no complications and the patient progressed well (Figure 8).
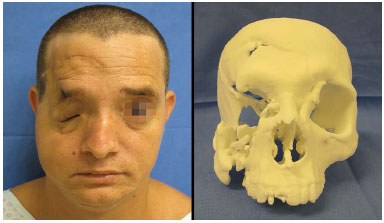
Figure 6. A 34 year-old patient with a panfacial fracture sequelae with a zygomatico-orbital deformity.
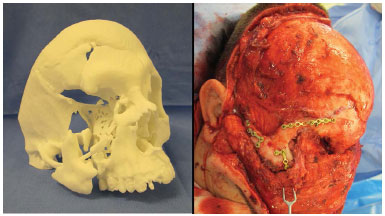
Figure 7. Prototype showing the zygoma location in the surgery room, and the zygoma repositioned and the orbit reconstructed with parietal bone in the trans-operative period

Figure 8. Preoperative and 17th month postoperative with the repositioned zygoma.
Case 3
A 29-year-old patient presented with mandibular ameloblastoma, confirmed by biopsy, which extended from the subcondylar region to the right parasymphysis (Figure 9). The surgical planning, which was decided in a clinical meeting, was tumor resection with 1 cm margins and immediate reconstruction with a fibula-free bone graft and a condylar prosthesis. For this woman, we decided to make prototypes of the craniofacial and donor fibula. One day before the surgery, we took the prototypes to the surgical center, conducted the surgery, and, with the prototypes in our hands, we made some decisions and anticipated surgical movements. We opted for a proximal resection margin to preserve the cuspid tooth. The reconstruction plate was folded, molding it to the remaining bone and maintaining the mandibular transverse diameter and the occlusion. The exact height and position of the condylar prosthesis were adjusted in the temporomandibular joint (TMJ). After deciding how much of the fibula we would need and the number of osteotomies, we performed the osteotomy and abrasion of the remaining bone so that the fibula would fit perfectly. The size of the screws was selected for each bone segment (graft and native bone). All fixation material was sterilized after the model surgery (Figures 10 to 12). On the following day, we repeated everything that had been done with the prototype without any complications, and there was a clear decrease in the surgical time when using the prototype (Figures 13 and 14). The patient developed an infection in the surgical site the 3rd week after surgery and was treated with an intravenous antibiotic, and she experienced palsy in the marginal mandibular branch, which has been successfully treated by phonoaudiology. The condylar prosthesis seems to have slightly dislocated, misaligning the occlusion a bit, but with no impact on the opening of the mouth and chewing functions (Figure 15).

Figure 9. A 29-year-old patient with a mandibular ameloblastoma from the subcondylar region to the D parasymphysis D.
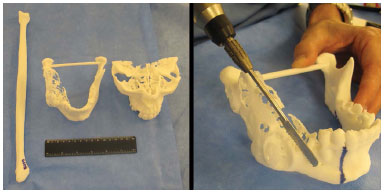
Figure 10. Prototyping of the craniofacial skeleton and fibula D, and model surgery 1 day before defining the resection margin.
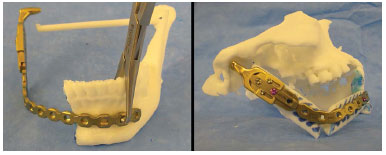
Figure 11. Resected tumor and transversal-shaped bar ensuring the transverse diameter, the fibula osteotomized and folded, the folded and fixed plate, and the prosthesis regulated and positioned in the glenoid.
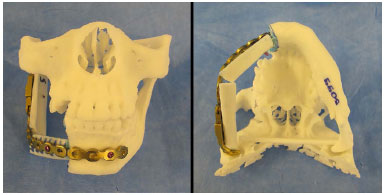
Figure 12. Abrasion of the symphysis for a better fit and screws selected. The bone contact is present with the transverse diameter maintained.
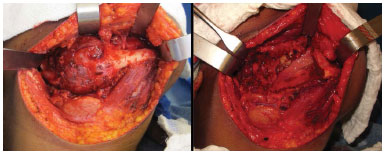
Figure 13. Subcondylar region ameloblastoma to the parasymphysis D, and remaining defect after resection.
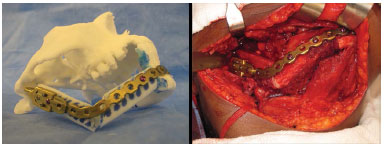
Figure 14. Similarity of the model surgery and the trans-operative period.

Figure 15. Preoperative and 8th month postoperative resection of ameloblastoma and immediate reconstruction with a fibula free graft and condylar prosthesis.
DISCUSSION
Prototyping can have applications in craniomaxillofacial surgery in many ways, including customized prosthesis manufacturing, surgical planning, and the educating of residents and patients11. In the cases presented here, we observed all these forms of application. The process of obtaining the prototype or customized prosthesis was very simple: we sent a DVD with the computerized tomography of patients to Eincobio®, in the case of the customized prosthesis, and to the Centro de Tecnologia da Informação Renato Archer, in the cases of the prototypes, and the material was available 1 to 2 weeks later.
In case 1, despite the fact that the autologous external parietal table graft is considered a gold standard in cranioplasties, we decided to use a customized prosthesis12. This decision was based on the size of the defect (> 36 cm2) and the patient's choice of this method. In cases like this one, a customized prosthesis has as its main advantages not requiring a donor area and excellent esthetic results, in that it has a part that fits perfectly in the defect. Nevertheless, there is the possibility of rejection of the alloplastic material and a greater risk of infection and extrusion than of an autologous graft13,14. An important technical detail in these cases is to ensure a good cover of the soft parts, creating a plane that accurately touches the dura-mater, and the re-opening of the borders of the defect to stimulate an integration of local tissue with the porous prosthesis.
In case 2, there was a severe panfacial fracture sequelae with practically a complete absence of the entire right zygomatico-orbital complex. It is a defect with difficult anatomical comprehension, in which we considered that prototyping would be useful to define more adequate surgical planning. The presence of the prototype in the surgery room also helped to more quickly and more accurately identify the zygoma piece that was loose between the soft parts of the patient at the level of the alveolar process of maxilla. The dislocated zygoma ascended as a free graft to its original location and reconstruction was completed using external parietal table grafts and rigid internal fixation. Having the view of the model and surgical field at the same time in the trans-operative period was a critical factor to conduct our work.
In case 3, a major surgery was conducted, with tumor resection compromising the totality of one hemi-mandible and the right TMJ, and reconstruction with microsurgical flaps, reconstruction plate, and a condylar prosthesis. The model surgery conducted one day before provided a number of benefits: decreased morbidity of the donor area (only the required amount was obtained); definition of the fibular osteotomy; definition of the resection margins; plate molding; selection of screws; maintenance of the mandibular transverse diameter; condylar prosthesis fitting in the TMJ; maintenance of the best possible occlusion; less surgical time, less anesthesia; and lower hospital costs15. An important technical detail of prototyping in this case was that we also asked for the prototyping of the skull base (containing the glenoid) and the manufacturing of a transversal-shaped bar from the medial face of one condyle to the other, which helped us in maintaining the mandibular transverse diameter and fitting the condylar prosthesis in the glenoid. We can cite as a disadvantage in this case the inability to sterilize the prototype, in particular regarding the donor fibular osteotomy. We got around this fact by covering the two model segments with sterile Tegaderm® and, thus, by placing the molds next to the obtained fibula, we could accurately reproduce the size and angle of the bevel that we had made in the previous day. There was no need to perform any adjustments to the plate fold or any other osteotomy or bone abrasion beyond that which was planned.
With regard to education, anatomical knowledge is a fundamental prerequisite to perform a surgery. Prototyping may improve the skills of surgeons in training and greatly help in clarifying patient doubts in regard to their current condition and expected results. The theoretical cost of this technology corresponds to costs associated with the three-dimensional printer, material from which the mold will be made, and software. Currently, the cost of a domestic 3D printer varies from US $500 to US $2500, and there are a great variety of not very expensive materials that can be used for the prototype, and the design software can be acquired online for free. Thus, the total cost will be determined by the type of material used, volume of material used, and prototype size. Once having acquired a printer, the cost for prototyping a complete skull may reach US $3400, including the material and electricity used11.
Even if prototyping is not part of the daily routine in many craniofacial surgery centers in Brazil, we believe that this technology has the potential to improve surgical teaching practices in some cases. With time, all these costs will probably decrease, making prototyping more accessible to everyone.
ACKNOWLEDGEMENTS
We would like to thank Eincobio® for donating the customized cranial prosthesis in case 1 and the Centro de Tecnologia da Informação Renato Archer for the prototyping in cases 2 and 3.
REFERENCES
1. Souza MA, Centeno TM, Pedrini H. Integrating 3D reconstruction of tomographic images and rapid prototyping for fabrication of medical models. Braz J Biomed Eng. 2003;19(2):103-15.
2. Bibb R, Taha Z, Brown R, Whight D. Development of a rapid prototyping design advice system. J Intell Manuf. 1999;10(3/4):331-9. DOI: http://dx.doi.org/10.1023/A:1008920512663
3. Choi JY, Choi JH, Kim NK, Kim Y, Lee JK, Kim MK, et al. Analysis of errors in medical rapid prototyping models. Int J Oral Maxillofac Surg. 2002;31(1):23-32. DOI: http://dx.doi.org/10.1054/ijom.2000.0135
4. Yeong WY, Chua CK, Leong KF, Chandrasekaran M. Rapid prototyping in tissue engineering: challenges and potential. Trends Biotechnol. 2004;22(12):643-52. DOI: http://dx.doi.org/10.1016/j.tibtech.2004.10.004
5. Grevera GJ, Udupa JK, Odhner D. An order of magnitude faster isosurface rendering in software on a PC than using dedicated, general purpose rendering hardware. IEEE Trans Vis Comput Graph. 2000;6(4):335-45. DOI: http://dx.doi.org/10.1109/2945.895878
6. Kai CC, Meng CS, Ching LS, Hoe EK, Fah LK. Rapid prototyping assisted surgery planning. Int J Adv Manuf Technol. 1998;14(9):624-30. DOI: http://dx.doi.org/10.1007/BF01192281
7. Klug C, Schicho K, Ploder O, Yerit K, Watzinger F, Ewers R, et al. Point-to-point computer-assisted navigation for precise transfer of planned zygoma osteotomies from the stereolithographic model into reality. J Oral Maxillofac Surg. 2006;64(3):550-9. PMID: 16487823 DOI: http://dx.doi.org/10.1016/j.joms.2005.11.024
8. Liu Q, Leu MC, Schmitt SM. Rapid prototyping in dentistry: technology and application. Int J Adv Manuf Technol. 2006;29(3):317-35. DOI: http://dx.doi.org/10.1007/s00170-005-2523-2
9. Rengier F, Mehndiratta A, von Tengg-Kobligk H, et al.3D printing based on imaging data: Review of medical applica-tions. Int J Comput Assist Radiol Surg. 2010;5:335-341.
10. Chim H, Schantz JT. New frontiers in calvarial reconstruction: integrating computer-assisted design and tissue engineering in cranioplasty. Plast Reconstr Surg. 2005;116(6):1726-41. PMID: 16267439 DOI: http://dx.doi.org/10.1097/01.prs.0000182386.78775.cd
11. Isaac M. Sculpteo 3-D printing app uses your mug to make a mug [Accessed: Ago 12, 2015]. Available from: http://www.wired.com/gadget-lab/2012/01/sculpteo-3d-printing-app/
12. Gerstle TL, Ibrahim AM, Kim PS, Lee BT, Lin SJ. A plastic surgery application in evolution: three-dimensional printing. Plast Reconstr Surg. 2014;133(2):446-51. PMID: 24469175
13. Hara T, Farias CASA, Costa MJM, Cruz RJL. Cranioplastia: parietal versus prótese customizada. Rev Bras Cir Plást. 2011;26(1):32-6.
14. Uygur S, Eryilmaz T, Cukurlouglu O, Ozmen S, Yavuzer R. Management of cranial bone defects: a reconstructive algorithm according to defect size. J Craniofac Surg. 2013;24(5):1606-9.
15. Reddy S, Khalifian S, Flores JM, Bellamy J, Manson PN, Rodriguez ED, et al. Clinical outcomes in cranioplasty: risk factors and choice of reconstructive material. Plast Reconstr Surg. 2014;133(4):864-73. PMID: 24675189
1. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brasil
2. Associação Brasileira de Cirurgia Crânio-Maxilo-Facial, Recife, PE, Brasil
3. Instituto Nacional de Traumatologia e Ortopedia, Rio de Janeiro, RJ, Brasil
4. Sociedade Brasileira de Neurocirurgia, Rio de Janeiro, RJ, Brasil
Institution: Instituto Nacional de Traumatologia e Ortopedia (INTO-RJ), Rio de Janeiro, RJ, Brasil.
Corresponding author:
Pablo Maricevich
Av. Engenheiro Antônio de Góes, 275, Pina
Recife, PE, Brasil CEP 51110-000
E-mail: jpmaricevich@hotmail.com
Article received: July 30, 2014.
Article accepted: April 21, 2015.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter