

Original Article - Year 2016 - Volume 31 -
Speech resonance and surgical complications after primary palatoplasty with intravelar veloplasty in patients with cleft lip and palate
Ressonância de fala e complicações cirúrgicas após palatoplastia primária com veloplastia intravelar em pacientes com fissura de lábio e palato
ABSTRACT
INTRODUCTION: The primary surgical correction of the palate is of fundamental importance in the rehabilitation of individuals with labiopalatine cleft and aims for local anatomical restoration and closure of the existing communication between the nasal and oral cavities, such as functional restoration of the velopharyngeal ring through repositioning of the palatine muscles. Palate closure techniques have evolved progressively over the years and increasingly involve repositioning of the muscles responsible for closing the velopharyngeal sphincter, called intravelar veloplasty. This procedure encourages the synergistic operation of the velar and pharyngeal musculature, thereby avoiding the symptoms resulting from velopharyngeal insufficiency. However, despite efforts to achieve adequate velopharyngeal function, intraoperative events and immediate postoperative and/or late complications may contribute to primary palatoplasty failure and consequently lead to hypernasality.
METHODS: Sixty patients underwent primary palatoplasty with intravelar veloplasty. Intraoperative events and immediate and late postoperative complications were investigated. The presence and location of palatal fistula or dehiscence was assessed by clinical evaluation. The patients also made an audio recording of their speech that was analyzed by three speech therapists. The intraoperative events and postoperative complications were descriptively analyzed. The association between intraoperative events and immediate and late postoperative complications with the formation of fistulae as well as that between the occurrence of fistulae and dehiscences and the presence and absence of hypernasality was analyzed using Fisher's exact test.
RESULTS: Overall, there was a 5% incidence of intraoperative events, 20% incidence of immediate complications, and 13.3% incidence of late complications. Fistulae and hypernasality were found in 16.67% and 18.6% of cases, respectively.
CONCLUSION: Palatoplasty with intravelar veloplasty is a safe and easily implemented technique that is efficient for speech and has low complication rates.
Keywords: Palate/surgery; Palatine muscles; Cleft lip; Cleft palate; Velopharyngeal insufficiency; Velopharyngeal sphincter; Postoperative complications.
RESUMO
INTRODUÇÃO: A correção cirúrgica primária do palato é de fundamental importância na reabilitação do indivíduo com fissura labiopalatina e visa tanto a restauração anatômica local, com o fechamento da comunicação existente entre a cavidade nasal e oral, como a restauração funcional do anel velofaríngeo por meio do reposicionamento dos músculos palatinos. Ao longo dos anos, as técnicas de fechamento de palato foram evoluindo progressivamente, utilizando, cada vez mais, o procedimento de reposicionamento da musculatura responsável pelo fechamento do esfíncter velofaríngeo, denominado veloplastia intravelar. Tal procedimento favorece o funcionamento sinérgico da musculatura velar e faríngea, evitando, assim, os sintomas decorrentes da insuficiência velofaríngea. No entanto, apesar de todos os esforços no sentido de conseguir o funcionamento velofaríngeo adequado, intercorrências intraoperatórias e complicações pós-operatórias imediatas e/ou tardias podem contribuir para o insucesso da palatoplastia primária e, consequentemente, levar ao aparecimento de hipernasalidade.
MÉTODOS: Sessenta pacientes submetidos à palatoplastia primária com veloplastia intravelar. Intercorrências intraoperatórias e complicações pós-operatórias imediatas e tardias foram investigadas. A presença e localização de fístula ou deiscência do palato foi feita por meio de avaliação clínica. Os pacientes foram submetidos, também, à gravação em áudio de amostra de fala, as quais foram analisadas por três fonoaudiólogas. As intercorrências intraoperatórias e as complicações pós-operatórias foram analisadas de forma descritiva. A associação entre as intercorrências intraoperatórias e complicações imediatas e tardias com a formação de fístulas, bem como a associação entre a ocorrência de fístulas e deiscências com a presença e ausência de hipernasalidade, foram analisadas por meio de Teste de Fisher.
RESULTADOS: Verificou-se 5% de intercorrências intraoperatórias, 20% de complicações imediatas e 13,3% de complicações tardias. O índice de fístulas foi de 16,67%. A proporção de hipernasalidade foi de 18,6%.
CONCLUSÃO: A palatoplastia com veloplastia intravelar utilizada no presente estudo demonstrou ser uma técnica segura, de fácil execução, eficiente para a fala e com baixos índices de complicações.
Palavras-chave: Palato/Cirurgia; Músculos palatinos; Fissura labial; Fissura palatina; Insuficiência velofaríngea; Esfíncter velofaríngeo; Complicações pós-operatórias.
The objectives of primary surgery of the palate include anatomical reconstruction of the oral and nasal cavity, muscle repositioning, and complete restoration of the velopharyngeal sphincter to provide adequate velopharyngeal closure and facilitate speech development1. Palatal closure techniques have evolved progressively over the years, and greater emphasis has been placed on repositioning the velar musculature to ensure a functional velopharyngeal sphincter with low complication rates. Studies in the literature2,3 show that "intravelar veloplasty" began to be used on a large scale. The main objective of intravelar veloplasty is to retroposition the muscles of the soft palate as posteriorly as possible to enable good mobility to the levator veli palatini and consequently improve velopharyngeal competence1,4.
Several studies have demonstrated that reconstruction of the velar musculature, conducted either conservatively or radically, as recommended by Sommerlad5 without increasing complication rates or fistulae is essential to achieve the best speech results. Dreyer and Trier6 reported improved speech results and a lower indication for secondary surgery for velopharyngeal insufficiency in patients who underwent surgery that included muscle reconstruction; Furlow7 defended his technique that involves muscular repositioning and palatal stretching with low rates of surgical complications but without the need for secondary surgery for velopharyngeal insufficiency.
Bitter et al.8 demonstrated that only 3% of patients who underwent intravelar veloplasty required a secondary surgery for velopharyngeal insufficiency. Sommerlad5 revealed that progressive improvement was obtained with an improved radical intravelar veloplasty technique with 10.2%, 4.9%, and 4.6% indication rates for velopharyngeal insufficiency surgery over the years. Andrades et al.1 demonstrated the importance of radical intravelar veloplasty, with only 6.7% of patients needing treatment for velopharyngeal insufficiency. Phua and De Chalain9 identified that 31.8% of patients had hypernasality after undergoing palatoplasty according to the techniques of Veau, Furlow, and von Langenbeck.
Jain et al.10 demonstrated that primary palatoplasty, even without the radical dissection of the levator and tensor muscles of the velum palatinum, led to speech improvements, especially in younger patients. Abdurrazaq et al.11 also argued that the von Langenbeck technique associated with intravelar veloplasty leads to good surgical results.
The most common cause of velopharyngeal insufficiency is cleft palate, the most frequent speech symptoms of which are hypernasality, the emission of nasal air, low intraoral air pressure, and compensatory articulations12-14. When the primary surgery of the palate is performed following predetermined surgical protocols, most patients achieve good speech results.
However, despite the acknowledged effort to establish adequate velopharyngeal function in primary palatoplasty, according to the literature, velopharyngeal insufficiency persists in 5-36% of individuals with cleft palate, a phenomenon that may be a result of the persistent anterior insertion of the muscle fibers as well as palatal shortening, especially when the palatal aponeurosis is absent and the levator muscles are hypoplastic or even in the presence of anatomical changes of the lateral and posterior pharyngeal walls15,16.
In such cases, the speech symptoms resulting from the velopharyngeal insufficiency can significantly impact speech intelligibility. In addition, complications such as the need for surgical revision for excessive bleeding, postoperative surgical-site or systemic infections, coughing, vomiting or fever, and others can alter the natural cicatrization process of the newly surgically manipulated palate.
A frequent complication of primary palatoplasty is the occurrence of fistula, an epithelial opening between the oral and nasal cavities that may vary in size and location and can compromise speech, causing hypernasality and nasal reflux with liquids or semisolids17. A recent survey showed that the incidence of fistula after primary correction of the palate is 2-45% and that this complication may occur with any surgical technique18. There are many surgical techniques for fistula correction; however, the recurrence rates are very high, 37-50%, and their prevention is fundamental17.
Some authors19 have reported fistula rates of 22.7% after surgery using the von Langenbeck technique, 18.2% after Furlow surgery, and 39.9% after the Bardach technique. Other studies have demonstrated a general rate of 12.8% after use of the Veau, Furlow and von Langenbeck technique9 and 29.8% after the von Langenbeck technique modified by intravelar veloplasty11. A lower rate of 7% was observed after radical intravelar veloplasty17.
Several complications may occur after primary palatoplasty, and different studies list and correlate the complications with other findings found in the early and late postoperative evolution of patient with cleft palate. In a recent study that assessed the prevalence of fistulae after primary correction of the palate, its location, and the association with the possible causative factors of the fistulae, it was observed that some factors such as initial cleft amplitude, intra- and postoperative complications, as well as surgeon skill, are statistically significant with regard to the occurrence of fistulae18.
OBJECTIVES
This study aimed to investigate the result of primary palatoplasty performed with intravelar veloplasty with regard to the rate of intraoperative events, rate of immediate and late postoperative complications, and hypernasality of speech; investigate the association between intraoperative events and immediate and late postoperative complications with the occurrence of fistulae and dehiscence; and further investigate the association between the occurrence of fistulae and dehiscence and the presence of hypernasality.
METHODS
Patients
This study was conducted at the Hospital for Rehabilitation of Craniofacial Anomalies - HRAC-USP, in Bauru, SP, between February 2012 and June 2014 and was approved by the institution's human research ethics committee (number: 207.843). A total of 60 consecutive patients (29 female, 31 male) were evaluated; of them, 35 (58.33%) had a unilateral cleft lip and palate, 16 (26.66%) had an incomplete cleft palate, five (8.33%) had a complete cleft palate, and four (6.66%) had a cleft lip and incomplete cleft palate. All patients underwent primary surgical correction of the palate between 12 and 18 months of age (mean, 13 months) performed by a single plastic surgeon. The study excluded patients with syndromes.
Surgical Technique
The primary palatoplasty was performed using the principles of the von Langenbeck technique, which features closure of the soft palate in three layers with or without a relaxing incision associated with intravelar veloplasty. In this case, broad muscle detachment of the nasal mucosa was performed with scissors and a Freer elevator with minimum detachment of the oral mucosa. The Freer elevator was subsequently used for muscle repositioning by smoothly pushing the partially adhered musculature to the oral mucosa and wide detachment from the nasal mucosa to a more posterior position (Figure 1).

Figure 1. Intravelar veloplasty procedure.
Clinical Evaluation of Plastic Surgery
Intraoperative events
The intraoperative events of each case were collected from the medical charts and recorded with the plastic surgeon or surgical team who performed the surgery. The following events were investigated: excessive bleeding, mucosal laceration, extubation, and others that were observed and recorded.
Postoperative complications
Complications such as bleeding, surgical or non-surgical infection, local trauma, cough, fever, persistent crying, and postoperative vomiting were investigated at two time points:
- Immediate postoperative complications: surgical bleeding, fever, cough, persistent crying, and vomiting recorded up to 24 hours after surgery and obtained from medical charts;
- Late postoperative complications: bleeding, surgical infection, non-surgical infection, cough, crying, and local trauma obtained from interviews with parents or caregivers that occurred after hospital discharge (in addition to the 24 hours immediately after surgery).
Clinical evaluation
The patients were evaluated by the same plastic surgeon a mean 14.8 months after surgery to investigate the presence, location, and approximate size of soft-palate fistulae. The Pittsburg20 classification was used to identify the location (Figure 2). The size was estimated as small (< 3 mm in the largest axis), medium (3-5 mm in the largest axis), or large (> 5 mm in the largest axis). During the oral inspection, the presence and location of palatal dehiscence was also investigated.
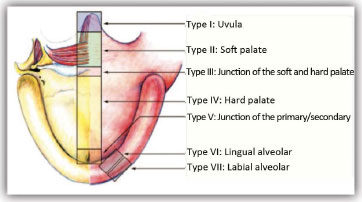
Figure 2. Pittsburg classification used to identify fistula location. Originally published in: Smith DM, Vecchione L, Jiang S, Ford M, Deleyiannis FW, Haralam MA, et al. The Pittsburgh Fistula Classification System: a standardized scheme for the description of palatal fistulas. Cleft Palate Craniofac J. 2007;44(6):590-4.
Recording of Speech Sample
All patients also made a digital audio recording of a speech sample in an acoustically treated room using the Wave Studio (Creative Labs) program with an Audigy 2 (Creative Labs) sound card and a Superlux headset microphone (model PRA-30 XLR). The mean patient age at the time of the speech recording was 3.2 years (range, 2-6 years). The speech sample consisted of spontaneous conversation, counting from 1 to 10, and the repetition of words with plosive and fricative sounds or the naming of figures containing the same words in cases in which the child did not repeat the vocalization. The speech samples were edited and analyzed by three speech therapists with experience in the speech assessment of individuals with a labiopalatine cleft. The three evaluators rated the hypernasality as missing (score 1) or present (score 2). The final score was the result of the consensus among them for each analyzed sample.
Statistical Analysis
The intraoperative events, immediate and late postoperative complications, and occurrence of fistulae and dehiscence were descriptively analyzed.
The final hypernasality score for each patient was established based on consensus among the three evaluators regarding symptom presence or absence. The intra-group agreement index was established using the Kappa coefficient according to the following interpretation: < 0, without concordance; 0-0.19, poor concordance; 0.20-0.39, fair concordance; 0.40-0.59, moderate concordance; 0.60-0.79, substantial concordance; and 0.80-1.00, almost perfect concordance21.
The association between intraoperative events and immediate and late complications and fistula formation as well as the association between the occurrence of fistulae and dehiscence and the presence or absence of hypernasality was analyzed by Fisher's exact test.
RESULTS
Clinical Evaluation of Plastic Surgery
Of the 60 patients who underwent surgery, 38 (63.33%) required a bilateral relaxing incision; in eight (13.33%), the incision was performed unilaterally; and in 14 (23.33%), it was not performed. In 22 (36.67%) patients, a mucous vomer flap was used to close the hard palate, while in 17 (28.33%), tamponade with absorbable hemostatic sutures composed of regenerated cellulose (Surgicel®) was used in the relaxing incisions and/or bloody area of the vomer.
Intraoperative events
Excessive bleeding was found in only one (1.66%) patient; in two (3.33%) patients, mucosal laceration occurred during the surgery.
Immediate postoperative complications
There were 12 complications in 11 patients. One patient presented with fever and coughing. Five (8.33%) patients presented with cough, three (5%) had fever, two (3.33%) showed persistent crying, one (1.66%) had bleeding, and one (1.66%) presented with vomiting in the first 24 hours after the surgery.
Late postoperative complications
Four (6.66%) patients presented with cough after surgery, two (3.33%) had bleeding with spontaneous remission, and two (3.33%) had an infection not related to the surgery. One of the patients presented with bleeding and coughing.
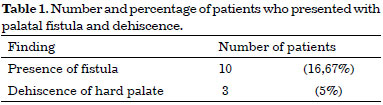
In the post-surgical clinical evaluation, fistula was noted in 10 patients (16.67%) (Table 1). According to the adopted classification, one (1.66%) patient presented with a type II fistula, four (6.66%) had type III, four (6.66%) had type IV, and one (1.66%) had type V. In seven (11.67%) patients, the fistulae were classified by the surgeon as small; in three (5%) patients, they were medium-size. Table 1 also presents the three (5%) cases of palatal dehiscence, all in the hard palate.
Analysis of Speech Hypernasality
Of the 60 speech samples analyzed, one was excluded due to the large number of phonological disorders within it, which prevented the hypernasality assessment. Thus, the speech resonance analysis was performed in 59 samples. The intra-group concordance regarding the presence or absence of hypernasality was 100%, with a Kappa coefficient of 1.00 (almost perfect concordance). The presence of hypernasality after primary palatoplasty was confirmed in 18.64% (11/59 patients) (Figure 3).
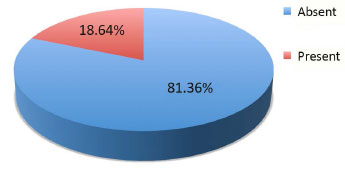
Figure 3. Percentage of patients with versus without hypernasality.
The statistical analysis showed that there was no significant association between the presence of fistulae or dehiscence with hypernasality (p = 0.237) (Figure 3).
Association between Intraoperative Events and Immediate and Late Postoperative Complications with Fistula Occurrence
To facilitate the analysis of the association between intraoperative events and immediate and late complications with fistula formation, the three cases of dehiscence were grouped with the fistulae since they are similar complications with similar repercussions. Thus, the total number of patients was 13. In addition, in this analysis, the number of patients with immediate (n = 11) and late (n = 7) complications, rather than the number of occurrences, was considered.
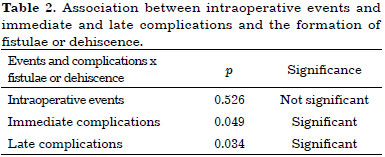
Association between Intraoperative Events and Fistula and Dehiscence Occurrence
Of the 13 patients with fistulae and dehiscences, 12 (92%) exhibited no intraoperative events and one (8%) experienced intraoperative events. On the other hand, of the 47 patients without fistula or dehiscence, two (4%) presented intraoperative events and 45 (96%) exhibited no events. According to Fisher's exact test, the association between the intraoperative events and the occurrence of fistulae was not significant (p = 0.526).
Association between Immediate Complications and Fistula and Dehiscence Occurrence
Of the 13 patients with fistulae and dehiscence, eight (62%) exhibited no immediate complications and five (38%) presented complications. On the other hand, of the 47 patients without fistula and dehiscence, six (13%) showed immediate complications and 41 (87%) had no complications. Fisher's exact test indicated that the association between immediate complications and the occurrence of fistulae or dehiscence was significant (p = 0.049).
Association between Late Complications and Fistula and Dehiscence Occurrence
Of the 13 patients with fistulae and dehiscences, nine (69%) exhibited no late complications and four (31%) presented complications. On the other hand, of the 47 patients without fistula and dehiscence, three (6%) had late complications and 44 (94%) had no complications. Fisher's exact test indicated that the association between the late complications and the formation of fistulae or dehiscence was significant (p = 0.034).
Table 2 summarizes the results of the analysis of the association between the events and complications with the formation of fistulae and dehiscence.
Association between Fistula and Dehiscence Occurrence and the Presence or Absence of Hypernasality
Of the 13 patients with fistulae and dehiscences, nine (69%) did not exhibit hypernasality and four (31%) showed hypernasality. On the other hand, of the 46 patients without fistula and dehiscence, seven (15%) presented hypernasality and 39 (85%) did not. The statistical analysis showed no significant association between the presence of fistulae or dehiscence and the presence of hypernasality (p = 0.237).
DISCUSSION
Primary palatoplasty should always be performed with the intent to reposition the velar musculature, either by more traditional techniques such as the von Langenbeck technique associated with intravelar veloplasty and the technique of Furlow, which also allows palatal elongation, or by the Sommerlad technique of radical intravelar veloplasty. In any case, it should be performed under the best possible clinical conditions, with pre-established routines, thus preventing postoperative complications that interfere with the desired results.
Here we sought to analyze the results of primary palatoplasty performed by a single plastic surgeon, whose surgical technique combined the von Langenbeck technique with intravelar veloplasty considering the event and postoperative complication rates and the speech hypernasality rate of patients as criteria for the analysis of surgical success.
In all surgeries performed, the musculature was maintained partially adhered to the oral mucosa and widely detached from the nasal mucosa to better reposition the muscles. While the learning curve of surgical palatal repair is long since it is a delicate surgery performed frequently in a limited surgical field, the modification of the maneuvers and strategies of a technique require extensive plastic surgeon experience and skill.
The previous experience of this author using the veloplasty technique with wider muscular detachment from the oral mucosa revealed a high incidence of dehiscence and even necrosis of the suture of the oral mucosa, which sometimes led to local healing by a second intention. It is well known that this more rigid healing may hinder the appropriate movement of the velopharyngeal musculature and, therefore, harm the speech outcomes.
On that basis, we performed a more conservative dissection of the oral mucosa during the intravelar veloplasty procedure and evaluated its results; this was the objective of this study. The technique performed resembles intravelar veloplasty type IIb, described in the literature in a classification proposal based on the dissection degree and velar muscle repositioning1.
Intra- and postoperative complications occurred in all surgeries according to pathology and severity. In the literature, several studies cited the complications found after palatoplasty, although they focused on different parameters of particular interest and performed very distinct statistical analyses.
The presence of fever and respiratory stridor occurred in 4.5% of patients studied7, while major complications affected 1.9% and included reintubation in one patient and the need for revision of surgical hemostasia by bleeding1. There were no reports of hematoma or surgical infection22; there was one case of bleeding 48 hours after surgery in two studies at rates of 5% and 0.76%, respectively10,11. Other authors reported three cases (1.71%) of surgical infection in their patients23; 5.77% included excessive bleeding and 4.92% featured laceration, although these authors reported a high proportion (40.06%) of general intraoperative events18. In the present study, the rate of intraoperative events was 5%: 1.66% excessive bleeding and 3.33% mucosal fraying or laceration.
These incidences of reduced intraoperative events may be related to surgeon experience and ability, nursing and anesthesiology team experience positioning the patient on the surgical table, and the mounting and positioning of the tracheal cannula to allow the placement of the mouth gag without risk of its freeing from the trachea or its compression and controlled hypotension in the intraoperative period. Infiltration of the palate with anesthetic (1% lidocaine with epinephrine) is used that, together with hypotension fostered by the general anesthesia, leads to less bleeding in the intraoperative period, greatly facilitating the planned surgical dissection and reducing the need for electrocautery, thus reducing complication rates.
With regard to the immediate postoperative complications, the following rates were found in this study: cough, 8.33%; fever, 5%; crying, 3.33%; bleeding, 1.66%; and vomiting, 1.66%. The incidence of fever, for example, is comparable to the 4.5%7 and 3.48%18 rates reported in the literature. Regarding immediate postoperative bleeding and vomiting, the rates of the present study were lower than the 7.66% and 9.76%18 observed in another study.
The late postoperative complications observed in this study were cough at 6.66%, bleeding at 3.33%, and non-surgical infections at 3.33%, which were also lower than those reported by other studies18. It is worth mentioning that no patients required a secondary surgery for surgical hemostasis. As with other authors who recommend the maintenance of the use of an antibiotic (cephalexin) for 5 days or amoxicillin + clavulanate for 7 days after surgery10,22, in the present study, the patients received cephalexin for 7 days after the surgery, which may explain the zero rate of surgical infection.
The proportion of patients with hypernasality in this study was 18.6%. In one of the few studies that also examined the presence of hypernasality after primary palatoplasty, the authors9 reported a higher proportion, 31.8%, in the general sample and observed differences in these rates when they separated patients by cleft type, observing a higher proportion in patients with cleft that affected the hard and soft palate compared to patients with cleft palate alone.
The criterion adopted in this study for assessing the presence or absence of hypernasality, based on consensus among three speech therapists experienced in assessing individuals with cleft palate, is based on international recommendations24. However, the great majority of studies in the literature evaluated the results of primary palatoplasty by the proportion of patients requiring a secondary surgery to correct the velopharyngeal insufficiency.
In the case of the Sommerlad radical intravelar veloplasty, we revealed very low rates of up to 4.6% of the cases with velopharyngeal insufficiency after palatoplasty. Andrades et al.1 and Sommerlad5 found that only 6.7% of patients had velopharyngeal insufficiency after radical intravelar veloplasty. On the other hand, these same authors reported 29% of cases with velopharyngeal insufficiency after surgery without radical intravelar veloplasty. In this case, the levator palati muscle was dissected from the palatine bone and nasal mucosa and kept fixed to the oral mucosa, creating an inverted "V" muscular belt, a technique that substantially resembles that used in the present study.
Other authors found that 26% of patients needed treatment for velopharyngeal insufficiency25, 18% of the patients underwent the Furlow technique and 29% underwent the von Langenbeck with velopharyngeal dysfunction26. It is not known yet how many of these 11 patients will require a secondary palate surgery since the children evaluated in the present study are not old enough for this surgical indication (mean age, 3 years). We speculate that, in some cases, phonotherapy may lead to the correction of articulation in addition to improving velopharyngeal function and, consequently, achieving balanced resonance.
We must consider, however, that the proportion of hypernasality found in this study is still significant. We believe we can reduce the hypernasality by performing a more extensive dissection of the muscles in the oral mucosa, which will probably provide more mobility to the musculature by favoring its posteriorization. We are already conducting this in a more judicious manner by further preserving the integrity and vascularization of the oral mucosa and using the minor salivary glands as a gauge of the oral mucosa dissection thickness. The results of this approach should be the object of future studies.
The occurrence of fistula of the soft palate is the most frequent complication in the surgical repair of the palate, with very variables rates reported in the literature of reduced proportions ranging from 0.9%1, 1.6%22, 4.5%7, of 5%25, and 7%27 to higher rates of 29.8%11 as well as 54% and 57% recorded by two groups of surgeons28. In a recent study performed in our service involving the results of several surgeons, a high post-palatoplasty fistula prevalence of 27%18 was reported.
This large variation in findings has been attributed to several factors, such as the surgical technique, age at the primary surgery, surgeon skill, cleft amplitude, cleft type, poor wound healing, patient nutritional status, suture tension, absence of closure of several layers, or even surgical-site11, 22.
In the present study, 10 patients (16.67%) developed palatal fistula, primarily in the junction of the hard and soft palate (four patients) and hard palate (four patients), followed by the soft palate and the junction between the primary and secondary palate (one patient in each case). A similar distribution, with a higher prevalence of fistulae verified at the junction between the hard and soft palate, was verified by other authors17,23.
In contrast, other authors identified a higher incidence of fistulae in the anterior palate (37.11%), followed by the medial region of the palate (32.08%), transition between the hard and soft palate (20.12%), and soft palate (5.03%)18. Regarding extension of the fistulae, in the present study, seven patients (70%) had small fistulae (< 3 mm), three (30%) had medium-sized fistulae (3-5 mm), and no patients had a large fistula. Other authors found a 41.67% incidence of small fistulae, 25% of medium-sized fistulae, and 33.33% of larger fistulae17. In another study27, fistulae considered large by the criterion adopted in this study were reported in 7% of patients at a mean 8 mm (range, 5-13 mm).
Despite the fact that the primary repair surgeries were performed in the same service and in very similar conditions to those investigated in a recent study in this hospital18, using the von Langenbeck technique, we believe that the lower incidence of fistulae verified in this study may be due to technical details of the implementation of the technique, such as the lower muscular detachment of the oral mucosa and less common use of electrocautery.
The lower detachment of the oral mucosa preserves more local vascularization, which provides better healing and reduces the likelihood of necrosis, dehiscence, or fistulae. The appropriate and precise use of electrocautery provides good hemostasis, less postoperative bleeding, and less devascularized local tissue, which also contributes to lower complication rates. Moreover, one cannot ignore the plastic surgeon's ability as one of the factors that led to the decreased incidence of fistulae observed in this study.
Of the 10 patients who developed palatal fistula, eight demonstrated nasal food reflux, an indication for surgery; one demonstrated no indication for closure; and closure was required during the alveolar bone graft surgery in another since an asymptomatic fistula was found in the transition between the primary and secondary palate and did not cause the patient any inconvenience.
In the three cases in which dehiscence occurred, the surgeries were performed with bilateral relaxing incisions, eliminating the possibility of sutures under tension as the cause. The three patients underwent successful reoperation, i.e. there was no recurrence.
In short, the palatoplasty with intravelar veloplasty technique used in this study was safe, easily implemented, and efficient for speech, and it featured low complication rates. In the future, this surgical technique is to be improved by further extending the muscle dissection to achieve the radical dissection recommended by Sommerlad.
CONCLUSION
The surgical technique employed here featured reduced rates of intraoperative events, postoperative complications, and speech hypernasality. The occurrence of fistulae and dehiscence was related to the immediate and late complications but not the presence of hypernasality.
REFERENCES
1. Andrades P, Espinosa-de-los-Monteros A, Shell DH 4th, Thurston TE, Fowler JS, Xavier ST, et al. The importance of radical intravelar veloplasty during two-flap palatoplasty. Plast Reconstr Surg. 2008;122(4):1121-30. PMID: 18827646 DOI: http://dx.doi.org/10.1097/PRS.0b013e3181845a21
2. Braithwaite F. Cleft palate repair. In: Gibson T. Modern trends in plastic surgery. Washington: Butterworth; 1964. p.35-43.
3. Kriens OB. An anatomical approach to veloplasty. Plast Reconstr Surg. 1969;43(1):29-41. PMID: 5765081 DOI: http://dx.doi.org/10.1097/00006534-196901000-00006
4. Sommerlad BC, Mehendale FV, Birch MJ, Sell D, Hattee C, Harland K. Palate re-repair revisited. Cleft Palate Craniofac J. 2002;39(3):295-307. DOI: http://dx.doi.org/10.1597/1545-1569(2002)039<0295:PRRR>2.0.CO;2
5. Sommerlad BC. A technique for cleft palate repair. Plast Reconstr Surg. 2003;112(6):1542-8. PMID: 14578783 DOI: http://dx.doi.org/10.1097/01.PRS.0000085599.84458.D2
6. Dreyer TM, Trier WC. A comparison of palatoplasty techniques. Cleft Palate J. 1984;21(4):251-3.
7. Furlow LT Jr. Cleft palate repair by double opposing Z-plasty. Plast Reconstr Surg. 1986;78(6):724-38. DOI: http://dx.doi.org/10.1097/00006534-198678060-00002
8. Bitter K, Wegener C, Gomille N. Intravelar veloplasty in cleft lip, alveolus and palate and outcome of speech and language acquisition: a prospective study. J Craniomaxillofac Surg. 2003;31(6):348-55. DOI: http://dx.doi.org/10.1016/j.jcms.2003.07.002
9. Phua YS, de Chalain T. Incidence of oronasal fistulae and velopharyngeal insufficiency after cleft palate repair: an audit of 211 children born between 1990 and 2004. Cleft Palate Craniofac J. 2008;45(2):172-8. PMID: 18333650 DOI: http://dx.doi.org/10.1597/06-205.1
10. Jain H, Rao D, Sharma S, Gupta S. Assessment of speech in primary cleft palate by two-layer closure (conservative management). J Surg Tech Case Rep. 2012;4(1):6-9. DOI: http://dx.doi.org/10.4103/2006-8808.100344
11. Abdurrazaq TO, Micheal AO, Lanre AW, Olugbenga OM, Akin LL. Surgical outcome and complications following cleft lip and palate repair in a teaching hospital in Nigeria. Afr J Paediatr Surg. 2013;10(4):345-57. DOI: http://dx.doi.org/10.4103/0189-6725.125447
12. Kummer AW. Resonance disorders and velopharyngeal dysfunction (VPD). In: Kummer AW. Cleft palate and craniofacial anomalies - effects on speech and resonance. San Diego: Singular; 2001. p.145-76.
13. Smith BE, Kuehn DP. Speech evaluation of velopharyngeal dysfunction. J Craniofac Surg. 2007;18(2):251-61. DOI: http://dx.doi.org/10.1097/SCS.0b013e31803ecf3b
14. Rudnick EF, Sie KC. Velopharyngeal insufficiency: current concepts in diagnosis and management. Curr Opin Otolaryngol Head Neck Surg. 2008;16(6):530-5. DOI: http://dx.doi.org/10.1097/MOO.0b013e328316bd68
15. Nakamura N, Ogata Y, Sasaguri M, Suzuki A, Kikuta R, Ohishi M. Aerodynamic and cephalometric analyses of velopharyngeal structure and function following re-pushback surgery for secondary correction in cleft palate. Cleft Palate Craniofac J. 2003;40(1):46-53. PMID: 12498605 DOI: http://dx.doi.org/10.1597/1545-1569(2003)040<0046:AACAOV>2.0.CO;2
16. Perry JL, Kuehn DP. Magnetic resonance imaging and computer reconstruction of the velopharyngeal mechanism. J Craniofac Surg. 2009;20 Suppl 2:1739-46. DOI: http://dx.doi.org/10.1097/SCS.0b013e3181b5cf46
17. Lu Y, Shi B, Zheng Q, Hu Q, Wang Z. Incidence of palatal fistula after palatoplasty with levator veli palatini retropositioning according to Sommerlad. Br J Oral Maxillofac Surg. 2010;48(8):637-40. DOI: http://dx.doi.org/10.1016/j.bjoms.2009.10.018
18. de Agostino Biella Passos V, de Carvalho Carrara CF, da Silva Dalben G, Costa B, Gomide MR. Prevalence, cause, and location of palatal fistula in operated complete unilateral cleft lip and palate: retrospective study. Cleft Palate Craniofac J. 2014;51(2):158-64. PMID: 23586365 DOI: http://dx.doi.org/10.1597/11-190
19. Arantes HL, Zampar AG, Oliveira Junior FC, Rosique MJF, Rosique RG, Leal WA, et al. Fístulas e deiscências em palatoplastia primária: uma experiência institucional. Rev Bras Cir Plást. 2008;23(2):112-5.
20. Smith DM, Vecchione L, Jiang S, Ford M, Deleyiannis FW, Haralam MA, et al. The Pittsburgh Fistula Classification System: a standardized scheme for the description of palatal fistulas. Cleft Palate Craniofac J. 2007;44(6):590-4. PMID: 18177198 DOI: http://dx.doi.org/10.1597/06-204.1
21. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159-74. PMID: 843571 DOI: http://dx.doi.org/10.2307/2529310
22. Losken HW, van Aalst JA, Teotia SS, Dean SB, Hultman S, Uhrich KS. Achieving low cleft palate fistula rates: surgical results and techniques. Cleft Palate Craniofac J. 2011;48(3):312-20. PMID: 20815713 DOI: http://dx.doi.org/10.1597/08-288
23. Becker M, Hansson E. Low rate of fistula formation after Sommerlad palatoplasty with or without lateral incisions: an analysis of risk factors for formation of fistulas after palatoplasty. J Plast Reconstr Aesthet Surg. 2013;66(5):697-703. PMID: 23462210 DOI: http://dx.doi.org/10.1016/j.bjps.2013.01.031
24. Lohmander A, Olsson M. Methodology for perceptual assessment of speech in patients with cleft palate: a critical review of the literature. Cleft Palate Craniofac J. 2004;41(1):64-70. PMID: 14697067 DOI: http://dx.doi.org/10.1597/02-136
25. Inman DS, Thomas P, Hodgkinson PD, Reid CA. Oro-nasal fistula development and velopharyngeal insufficiency following primary cleft palate surgery--an audit of 148 children born between 1985 and 1997. Br J Plast Surg. 2005;58(8):1051-4. DOI: http://dx.doi.org/10.1016/j.bjps.2005.05.019
26. Williams WN, Seagle MB, Pegoraro-Krook MI, Souza TV, Garla L, Silva ML, et al. Prospective clinical trial comparing outcome measures between Furlow and von Langenbeck Palatoplasties for UCLP. Ann Plast Surg. 2011;66(2):154-63. PMID: 21042188 DOI: http://dx.doi.org/10.1097/SAP.0b013e3181d60763
27. Bekerecioglu M, Isik D, Bulut O. Comparison of the rate of palatal fistulation after two-flap and four-flap palatoplasty. Scand J Plast Reconstr Surg Hand Surg. 2005;39(5):287-9. DOI: http://dx.doi.org/10.1080/02844310510006529
28. Maine RG, Hoffman WY, Palacios-Martinez JH, Corlew DS, Gregory GA. Comparison of fistula rates after palatoplasty for international and local surgeons on surgical missions in Ecuador with rates at a craniofacial center in the United States. Plast Reconstr Surg. 2012;129(2):319e-326e. DOI: http://dx.doi.org/10.1097/PRS.0b013e31823aea7e
1. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
2. Hospital de Reabilitação de Anomalias Craniofaciais, Bauru, SP, Brazil
Institution: Hospital de Reabilitação de Anomalias Craniofaciais - HRAC-USP, Bauru, São Paulo, Brazil.
Corresponding author:
Victor Zillo Bosi
Rua Silvio Marchione, 3-20 - Vila Universitária
Bauru, SP, Brazil, Zip Code 17012-900
E-mail: victorzb@terra.com.br
Article received: August 5, 2014.
Article accepted: November 17, 2014.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter