

Original Article - Year 2016 - Volume 31 -
Comparison between transconjunctival access with lateral canthotomy and subciliary access for the treatment of orbitozygomatic fractures
Comparação entre acesso transconjuntival com cantotomia lateral e acesso subciliar para tratamento das fraturas zigomáticoorbitárias
ABSTRACT
INTRODUCTION: Orbitozygomatic fractures most commonly occur in the midface. The main causes of fractures are traffic accidents, mainly by motorcycles, and interpersonal violence. The basic principles for the treatment of facial fractures are the reduction and fixation of the fracture site. It is fundamental that the surgical access be the most direct and broad as possible. Either the subciliary approach or transconjunctival access with lateral canthotomy can be used. The objective of this study was to evaluate and compare the complications, advantages, and disadvantages of the transconjunctival approach with lateral canthotomy and conventional subciliary access.
METHODS: We selected 15 patients in whom fractures were addressed through a subciliary incision and 15 patients in whom the fractures were addressed by using a transconjunctival incision with lateral canthotomy, and evaluated the incidence of complications with the two methods. The data were statistically analyzed by using the SPSS 20.0 software.
RESULTS: Thirty patients were operated with the subciliary access in 15 patients and the transconjunctival access in the other 15. Trauma occurred more frequently on weekends. The most frequent complications were apparent scar (26%), apparent sclera (23.3%), and ectropion (20%). Ectropion was more common in the > 60-year age group.
CONCLUSION: Both techniques were effective for the correction of fractures of the orbitozygomatic complex. The transconjunctival technique provides more esthetic and less stigmatizing scars. Hence, it is currently the author's first choice of treatment. The global incidence of complications was similar between the two techniques. Ectropion was less frequent with the transconjunctival access.
Keywords: Cranial fractures; Traffic accidents; Reconstructive surgical procedures; Orbit; Zygoma.
RESUMO
INTRODUÇÃO: Fraturas zigomático-orbitárias são as mais comuns do terço médio da face. As principais causas de fraturas são os acidentes de trânsito, principalmente por motocicletas, e a violência interpessoal. Os princípios básicos para o tratamento das fraturas faciais são a redução e a fixação do foco fraturário. É fundamental que o acesso cirúrgico seja o mais direto e amplo possível. Pode ser utilizada abordagem subciliar e transconjuntival com cantotomia lateral. O objetivo deste estudo é avaliar e comparar as complicações, vantagens e desvantagens da abordagem transconjuntival com cantotomia lateral e o acesso subciliar convencional.
MÉTODOS: Foram selecionados 15 pacientes nos quais as fraturas foram abordadas por meio de incisão subciliar e 15 pacientes nos quais as fraturas foram abordadas por incisão transconjuntival com cantotomia lateral e avaliadas a incidência de complicações com os dois métodos. Os dados foram analisados estatisticamente com o software SPSS 20.0.
RESULTADOS: Foram operados 30 pacientes, metade com acesso subciliar e metade com acesso transconjuntival. Os traumas ocorreram mais frequentemente aos finais de semana. As complicações mais frequentes foram cicatriz aparente (26%), esclera aparente (23,3%) e ectrópio (20%). Ectrópio foi mais comum no grupo acima de 60 anos.
CONCLUSÃO: Ambas as técnicas foram eficazes para correção das fraturas do complexo zigomático-orbitário. A técnica transconjuntival proporciona cicatrizes mais estéticas e menos estigmatizantes, constituindo hoje a primeira escolha do autor. A incidência global de complicações foi semelhante entre as duas técnicas. Ectrópio foi menos frequente com acesso transconjuntival.
Palavras-chave: Fraturas cranianas; Acidentes de trânsito; Procedimentos cirúrgicos reconstrutivos; Órbita; Zigoma.
Studies on the incidence of facial fractures indicate that orbitozygomatic fractures most commonly occur in the midface, representing 25% of the total cases. Most of the patients are male, with a mean age of 30 years1-3. The main causes of fractures by facial trauma are traffic accidents, mainly by motorcycles, and interpersonal violence4.
Several approaches for wider exposure of facial bone structures of the face have been proposed. The basic principles for the treatment of facial fractures are the reduction and fixation of the fracture site. Adequate exposure of the affected areas greatly facilitates the repair work. Therefore, the surgical access to the fractured bone site should be the most direct route and as broad as possible. Generally, this choice is made based on the fracture site and surgeon experience.
Besides the quality of exposure, esthetic considerations are essential with regard to the face, as an exaggerated apparent scar can become a bigger problem for the patient than the very reason for which the surgery was indicated4.
Trauma in the region of the orbitozygomatic complex can cause several esthetic deformities and functional disabilities, ranging from facial depressions to deficiencies in the movement of the eyeball.
Fractures of the orbital floor and medial wall of the orbit may clinically present as simple signs of trauma, such as edema and periorbital ecchymosis. Injury to the infraorbital nerve due to contusion or rupture and poor positioning of the eyeball that results in diplopia denotes more severe fractures.
Imaging diagnosis is performed mainly by means of computed tomography on sagittal and coronal planes5. Three-dimensional reconstruction is important in the understanding of fractures that would enable surgical planning that conforms to the characteristics of the fractures to be corrected6.
The classical approach to the treatment of this kind of fracture is the transcutaneous subciliary incision, which is well established in the literature2,4. Esthetic transconjunctival blepharoplasty was initially proposed by Bourguet7 in 1924 and improved by Tessier8 in 1973. It was disseminated by Graf in 2001, with excellent results9. The use of the transconjunctival access in lateral canthotomy for fractures of the complex orbitozygomatic maxillary occurred only in 198510. Since then, it has become a viable and esthetically acceptable option for completion of definitive treatment, with a lower index of complications such as ectropion and apparent scars.
OBJECTIVE
The objective of this study was to evaluate and compare the complications, advantages, and disadvantages of the transconjunctival approach with lateral canthotomy and those of the subciliary approach in the treatment of fractures of the orbitozygomatic complex.
The authors have no conflict of interest.
METHODS
This study included patients who underwent operation by the senior author between 2000 to 2013 in two hospitals, namely Nove de Julho and Bandeirantes, in São Paulo, SP. All the patients incurred craniomaxillofacial trauma with fractures of the orbitozygomatic maxillary complex.
Altogether, we selected 15 patients whose fractures were treated through a subciliary incision and 15 other patients whose fractures were treated by a transconjunctival incision with lateral canthotomy.
In all cases, strict physical examination was performed along with computed tomographic imaging of facial bones on sagittal and coronal planes, for better evaluation of the cases and surgical planning. Three-dimensional reconstruction was performed whenever possible, although it does not constitute an essential treatment measure.
The exclusion criteria were patients with a history of surgical manipulation of the lower eyelid region, those with conditions that could interfere with healing, and those who already had some degree of entropion or ectropion.
All the patients were reassessed at 15 days, 1 month, 3 months, 6 months, and 1 year after surgery.
Surgical access was performed according to the standard technique described as follows: Initially, infiltration was performed with xylocaine and adrenaline solution at a concentration of 1:100,000 in the incision and detachment area. Then, the skin incision was made by using a No. 15 cold blade, and lateral canthotomy was completed with curved iris scissors. Then, the transition area between the eyeball and the conjunctiva was sectioned also with scissors, and dissection was completed with cautery, from the Colorado tip up to the subperiostal plan. The dissection was performed from the lateral canthus up to 1 cm from the lacrimal punctum.
The lower eyelid was then everted, with wide exposure of the region, and the eyeball was protected during dissection. Subsequently, dissection was performed in the preseptal space until reaching the lower orbital rim. Then, blunt dissection with a Joseph elevator of the subperiostal plan was made to approach the fracture, with folding of the periosteum. The fractures of the orbital rim are fixed with miniplates and screws, and when an associated fracture was found on the orbital floor, a titanium mesh or ricinus communis bone composite was used for correction. The closure was initiated with Vicryl 4.0 sutures with separate points on the subperiostal plane. Then, the transconjunctival incision was closed with Vicryl 4.0 sutures. Finally, canthopexy was performed with colorless nylon 4.0, and the lateral canthal ligament was fixed in the periosteum of the upper orbit. Cutaneous suture was performed with nylon 6.0.
The subciliary technique was performed with an incision 1 mm below the lash lines, preserving them. A myocutaneous detachment was performed with curved iris scissors, with the opening of the lower orbital septum and dissection with electrocautery with a Colorado tip, folding the periosteum and isolating the fracture site. After the fixation of the fracture, the periosteum and skin were sutured with Vicryl 4.0 and nylon 6.0, respectively.
For postoperative care, the head was elevated and saline solution compresses were continuously cooled between 2°C and 8°C were applied. In addition, intravenous (cefazolin) and topical antibiotics (tobramycin) were prescribed. Lubricant eye drops was used in the operated eye every 3 hours during the day and a lubricating eye ointment before bedtime. The patients were examined closely in the first postoperative day to ensure that retro-orbital bleeding, ectropion, or loss of visual acuity did not occur.
Medical records were retrospectively analyzed, and the data were analyzed descriptively. Categorical variables were presented as absolute and relative frequencies; and numerical variables, as summary measures (mean, quartiles, minimum, maximum, and standard deviation).
The associations between two categorical variables was verified by using the chi-square test or, alternatively, the Fisher exact test when the number of sample cases was small, where > 20% of the cells in the contingency table had expected values of < 5 cases. Mean values were compared between the two groups by using the Student t test for independent samples, which has an assumption of normality of data. In the event that this assumption was not met, the Mann-Whitney non-parametric test was used. The normality of data was verified by using the Kolmogorov-Smirnov test.
For all statistical tests, a significance level of 5% was adopted.
The statistical analyses were performed by using the statistical software SPSS 20.0.
All the patients who agreed to participate in the study signed a free and informed consent form.
RESULTS
Data from the 30 patients were analyzed, of whom 50% underwent surgery via the transconjunctival access (Figures 1 to 4) and the other 50% underwent surgery via the subciliary approach (Figures 5 and 6). Most of the patients (73.3%) were male.

Figure 1. Fracture of the right orbit. Transconjunctival access with lateral canthotomy. Before and 30 days after operation.

Figure 2. Orbital and right maxilla fracture. Transconjunctival access with lateral canthotomy. Before and 30 days after operation.

Figure 3. Nasal fracture, zygomatic arch right, right maxilla, and the orbital floor. Transconjunctival access with inclusion of membrane for reconstruction of the orbital floor. Before and 30 after operation.

Figure 4. Fracture of the right orbit. Transconjunctival access. Before and 30 days after operation.

Figure 5. Fracture of the right orbit. Subciliary access. Before and 30 days after operation.
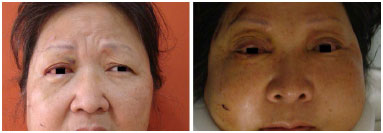
Figure 6. Fracture of the orbit, maxilla, zygomatic arch, and orbital floor. Subciliary access with the use of membrane for reconstruction of the orbital floor. Before and 30 days after operation. Discreet ectropion in the right eye.
The subciliary and transconjunctival access groups comprised of 10 (66.7%) and 12 male patients (80.0%), respectively, with no differences between these proportions (p = 0.682 - Fisher exact test).
The mean (SD) age was 48.5 (21.5) years, and the youngest patients who underwent operation with the transconjunctival and subciliary access were 21 and 23 years old, respectively, and the oldest were 82 and 91 years old, respectively. The patients in the subciliary access group had a mean (SD) age of 48.8 (25.2) years; and those in the transconjunctival group, 48.2 (18.0) years, with no difference between the mean ages (p = 0.600 with the Student t test).
Trauma occurred more frequently on weekends (Friday, Saturday, and Sunday) than in the other days of the week.
The signs resulting from trauma that are most commonly observed in our study series were palpebral hematoma, with 19 cases, followed by conjunctival ecchymosis, with 12 cases; conjunctival edema, with 10 cases; regional paresthesia, with cases; and zygomatic sinking, with 10 cases. No case of exophthalmos and palpebral ptosis were found. Eyeball injury was observed in five patients, all in the transconjunctival access group. Infraorbital step was observed in four patients, one in the subciliary access group and three in the transconjunctival access group. Diplopia occurred in five patients, one in the subciliary access group and four in the transconjunctival access group.
The most common complication was apparent scar in the early postoperative period in eight patients (26.7%), four in each group. Apparent sclera was the second most frequent complication, occurring in seven patients (23.3%), four in the subciliary access group and three in transconjunctival access group. Ectropion occurred in six patients (20%), five with the use of the subciliary access and one with the use of the transconjunctival access. Among the patients in the transconjunctival access group, only one required reoperation, a young patient that presented extrusion of sutures. The patient underwent reoperation and evolved with ectropion, which presented spontaneous resolution and good late postoperative evolution. The cases of ectropion with subciliary access were resolved with lateral canthopexy and tarsal shortening, all with good late evolution. None of the patients had entropion.
As can be seen in Table 1, no statistically significant associations were observed between the complications reported and the type of surgery adopted. Table 2 shows six cases of ectropion, or 20% of the total study sample, five in the subciliary access group and one in the transconjunctival access group, without statistical significance (Figure 7). Apparent sclera was observed in seven patients, four (26.7%) in the subciliary access group and three (20%) in the transconjunctival access group (Figure 8).
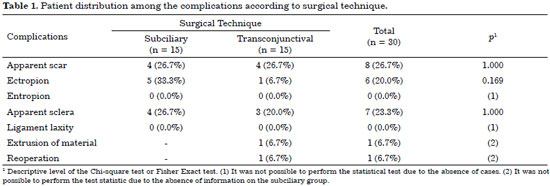
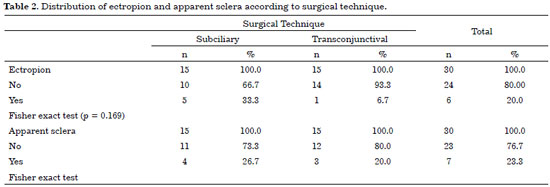
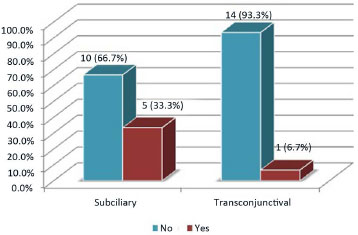
Figure 7. Patient distribution according to presence of ectropion and surgical technique.
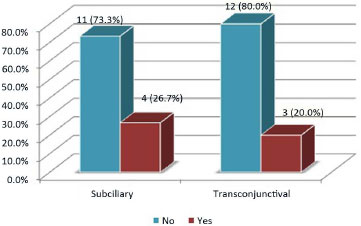
Figure 8. Patient distribution according to the presence of apparent sclera and surgical technique.
In the analysis of ectropion according to age group, the incidence was higher in the > 60-year age group. Apparent sclera was more common in the < 59-year age group.
DISCUSSION
Facial scars are a concern in modern society because they are stigmatizing and can cause great emotional discomfort to patients6.
The higher occurrence of injuries during the weekend is probably related to the greater occurrence of automobile accidents, intoxicated patients, and sporting activities.
In the treatment of fractures of the orbitozygomatic complex, the subciliary access has been largely used. However, one of its main disadvantage is the occurrence of a more apparent scar, in addition to the higher complication rate due to the manipulation of the muscles and palpebral septum1,2,4,6,11,12.
As the transconjunctival access with lateral canthotomy does not involve the orbicularis oculi muscle and orbital septum, local anatomical distortion and apparent scarring are minimized. For this reason, the technique was adopted by the author since 2011, with good results and a lower rate of complications since then.
Some factors involved in healing can be controlled by the surgeon, such as the traction of the tissues and surgical manipulation. However, some factors cannot be controlled and others are inherent to the quality of the healing of the patient, such as nutritional status and comorbidities such as diabetes mellitus and smoking11. The author believes that the transconjunctival access provides a less marked manipulation of tissues, with consideration for the orbicularis oculi muscle and orbital septum, with lower local traction. These factors justify the lower rate of complications associated with this technique, such as ectropion.
The transition area between the eyeball and the conjunctiva is generally marked by a transverse plexus of vessels that, in a variable way, covers the entire width of the fornix. The conjunctiva completely covers the internal palpebral surface. Between the muscles of the lower eyelid retractors and the septum, a potential space exists that communicates with the eyelid pads of the lower orbit. The transconjunctival access does not involve the anterior lamella. In the middle lamellar are the orbital septum and eyelid pads; and in the posterior lamella, the retractors or capsulopalpebral fascia and conjunctiva. The main vascular supply of the lower eyelid is situated in the plane of the orbicularis oculi muscle9. In the transconjunctival access, the orbital septum is intact, which minimizes the incidence of lower eyelid retraction that can be observed with the subciliary technique9,10.
One of the main advantages of the transconjunctival technique to the subciliary technique is that it does not cause denervation of the pretarsal portion of the orbicularis oculi muscle, maintaining its function, leading to a lower incidence of ectropion in the postoperative evolution13,14.
With the use of the transconjunctival access, the main complications mentioned in the literature are ectropion, apparent scar, apparent sclera, and entropion6, which were confirmed by the author, although none of the patients in this study had entropion.
Between the two techniques, the transconjunctival access was associated with a higher incidence of entropion; and the subciliary access, with a higher incidence of ectropion15. The factors associated with these complications are the time interval between the onset of trauma and the start of treatment, patient age, the severity of the trauma, the size of the mini plate used in bone fixation, and the type of access used, which is considered as the most important factor16.
The only case of ectropion in the transconjunctival group occurred in a young patient aged 21 years, after surgical correction of extrusion of the suture material. No degree of tarsal flaccidity was observed, and ectropion probably occurred owing to the intense inflammatory process, the magnitude of the trauma, and the extensive surgical manipulation. It evolved favorably and spontaneously.
Almeida et al.6, in 2011, reported a series of 24 cases surgically treated via the transconjunctival access and found three cases of apparent sclera, one case of ectropion, and one case of apparent scar. Meanwhile, in the present study, 15 cases were surgically treated, three cases had apparent sclera, one had ectropion, and four had apparent scars.
Oliva et al.17 describe an excellent result with the use of the subciliary access to treat fractures of the orbitozygomatic complex, with a technical variation in the dissection in the subcutaneous plane and muscle transfixation up to the orbital rim. However, they recognized the higher rate of complications associated with this technique, with ectropion reported in up to 42% in some series, such as those of Wary et al.18 and Holtmann et al.15, which was subjected to much criticism1.
Bähr et al.11, in their study on the subciliary access, found a lower rate of late complications when treatment was performed up to 24 hours after trauma onset. In addition, they found a higher rate of complications when the surgical interventions were performed between the second and sixth days after trauma onset.
The absence of flaccidity of the canthal ligament in the transconjunctival access group is probably associated with the routine use of lateral canthopexy, which was not observed in the subciliary access group. Ectropion was more common in the patients older than 60 years, which denotes that tarsal flaccidity, which is inherent to the process of aging, interferes greatly in the occurrence of this complication.
The occurrence of apparent sclera showed no significant difference between the two groups, which probably is justified by the immediate postoperative edema, as all cases presented spontaneous resolution in the first 3 postoperative months.
CONCLUSION
Both techniques were effective in the correction of the fractures of the orbitozygomatic complex. The transconjunctival technique provided more esthetic and less stigmatizing scars. Hence, it is currently the author's first choice of treatment. In this study, the overall incidence of late complications was similar between the two techniques, except for ectropion, which was less frequently observed with the use of the transconjunctival access. Larger studies are needed for more consistent conclusions.
REFERENCES
1. Araújo MM, Pereira CCS, Oliva MA, Costa DA. Acesso transconjuntival para fraturas do complexo zigomático orbitário: relato de caso. Rev Cir Traumatol Buco-Maxilo-Fac. 2006;6(4):39-48.
2. Timoteo CA, Chagas JFS, Rapoport A, Denardin OVP. Avaliação da abordagem palpebral subtarsal no tratamento cirúrgico das fraturas zigomático-orbitais. Rev Col Bras Cir. 2009;36(5):382-91. DOI: http://dx.doi.org/10.1590/S0100-69912009000500005
3. Horibe EK, Pereira MD, Ferreira LM, Andrade Filho EF, Nogueira A. Perfil epidemiológico de fraturas mandibulares tratadas na Universidade Federal de São Paulo - Escola Paulista de Medicina. Rev Assoc Med Bras. 2004;50(4):417-21. DOI: http://dx.doi.org/10.1590/S0104-42302004000400033
4. Timoteo CA, Chagas FS, Dedivitis RA. Avaliação da abordagem subtarsal no tratamento cirúrgico das fraturas zigomático-orbitárias. Rev Cir Traumatol Buco-Maxilo-Fac. 2009;9(4):73-80.
5. Souza EMR, Rocha RS, Silva LCF. Reconstrução orbitária com tela de titânio: relato de dois casos. Rev Cir Traumatol Buco-Maxilo-Fac. 2009;9(1):75-82.
6. Almeida ARB, Martins AO, Cavasini Neto A, Patrocínio JA, Naves MM, Patrocínio LG. Avaliação do acesso transconjuntival com cantotomia lateral no tratamento cirúrgico das fraturas zigomático-orbitárias. Rev Bras Cir Craniomaxilofac. 2011;14(2):75-9.
7. Bourguet J. Notre traitement chirurgical de "poches" sous les yeux sans cicatrice. Arch Gr Belg Chir. 1928;31:133-7.
8. Tessier P. The conjunctival approach to the orbital floor and maxilla in congenital malformation and trauma. J Maxillofac Surg. 1973;1(1):3-8. DOI: http://dx.doi.org/10.1016/S0301-0503(73)80005-0
9. Graf R, Auerswald A, Bernardes A, Damasio RC, Araujo, Graf CM. Blefaroplasia Inferior Transconjuntival. Rev Soc Bras Cir Plást. 2001;16(2):59-74.
10. Nunery WR. Lateral canthal approach to repair of trimalar fractures of the zygoma. Ophthal Plast Reconstr Surg. 1985;1(3):175-83. DOI: http://dx.doi.org/10.1097/00002341-198501030-00004
11. Bähr W, Bagambisa FB, Schlegel G, Schilli W. Comparison of transcutaneous incisions used for exposure of the infraorbital rim and orbital floor: a retrospective study. Plast Reconstr Surg. 1992;90(4):585-91. PMID: 1409993 DOI: http://dx.doi.org/10.1097/00006534-199210000-00006
12. Converse JM, Firmin F, Wood-Smith D, Friedland JA. The conjunctival approach in orbital fractures. Plast Reconstr Surg. 1973;52(6):656-7. PMID: 4759221 DOI: http://dx.doi.org/10.1097/00006534-197312000-00010
13. Zarem HA, Resnick JI. Expanded applications for transconjunctival lower lid blepharoplasty. Plast Reconstr Surg. 1991;88(2):215-20. DOI: http://dx.doi.org/10.1097/00006534-199108000-00006
14. Trelles MA, Baker SS, Ting J, Toregard BM. Carbon dioxide laser transconjunctival lower lid blepharoplasty complications. Ann Plast Surg. 1996;37(5):465-8. DOI: http://dx.doi.org/10.1097/00000637-199611000-00002
15. Holtmann B, Wray RC, Little AG. A randomized comparison of four incisions for orbital fractures. Plast Reconstr Surg. 1981;67(6):731-7. DOI: http://dx.doi.org/10.1097/00006534-198106000-00003
16. Antonyshyn O, Gruss JS, Galbraith DJ, Hurwitz JJ. Complex orbital fractures: a critical analysis of immediate bone graft reconstruction. Ann Plast Surg. 1989;22(3):220-33. DOI: http://dx.doi.org/10.1097/00000637-198903000-00009
17. Oliva MA, Pereira CCS, Jardim ECG, Okamoto R, Araujo MM. Acesso subciliar para fraturas do complexo zigomático-orbitário. Rev Bras Cir Cabeça Pescoço. 2013;42(2):106-8.
18. Wray RC, Holtmann B, Ribaudo JM, Keiter J, Weeks PM. A comparison of conjunctival and subciliary incisions for orbital fractures. Br J Plast Surg. 1977;30(2):142-5. DOI: http://dx.doi.org/10.1016/0007-1226(77)90009-1
1. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
2. Hospital dos Defeitos da Face, São Paulo, SP, Brazil
Institution: Clínica Matsunaga, São Paulo, SP, Brazil.
Corresponding author:
Wilson Yoshito Matsunaga
Rua Itapeva, 518, 15° andar - Bela Vista
São Paulo, SP, Brazil Zip Code 01332-000
E-mail: clinicadrmatsunaga@yahoo.com.br
Article received: July 28, 2014.
Article accepted: November 17, 2014.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter