

Original Article - Year 2016 - Volume 31 -
Use of acellular dermal matrix xenograft in reconstructive plastic surgery
Uso de matriz dérmica acelular heteróloga em cirurgia plástica reparadora
ABSTRACT
INTRODUCTION: Complex wounds pose a challenge to the plastic surgeon. In these cases, the most common solution is skin grafting or the use of flaps; however, depending on the affected structure, the results may not be satisfactory. Matrices were initially developed for the treatment of burn sequelae. Since then, different varieties of matrices have been developed for application in the treatment of several diseases, including complex wounds. Only a few heterologous acellular dermal matrices (HADMs) are available in Brazil, and they are still very expensive. The objective of this study was to report the experience with the use of HADMs for the treatment of patients with a need for reconstructive plastic surgery.
METHOD: From February 2011 to July 2014, five different HADMs were used in the treatment of 24 lesions of different etiologies, including three etiologies not previously described in the literature: rhinophyma, hidradenitis suppurativa, and Lyell's syndrome (toxic epidermal necrolysis).
RESULTS: Twenty patients with lesions of different etiologies and who received treatment with HADM grafts in different anatomical regions, associated or not with autologous skin grafting, attained adequate aesthetic and functional results.
CONCLUSION: The use of HADMs can be considered an alternative in the treatment of several difficult-to-treat cases, and has its place in modern plastic surgery; however, its indication should be carefully evaluated owing to the high cost of the materials.
Keywords: Biological dressings; Surgical flaps; Wounds; Healing; Reconstructive surgical procedures/methods.
RESUMO
INTRODUÇÃO: Feridas complexas são um desafio para o cirurgião plástico. Nestes casos, a solução mais comum é a indicação de enxertia de pele ou de retalhos, no entanto, dependendo das estruturas afetadas, os resultados podem não ser satisfatórios. As matrizes foram inicialmente desenvolvidas para o tratamento de sequelas de queimaduras. Desde então, desenvolveram-se diferentes variedades, as quais são aplicadas no tratamento de diversas patologias, inclusive feridas complexas. Apenas algumas matrizes dérmicas acelulares heterólogas (MDAH) estão disponíveis no Brasil e a um custo ainda muito elevado. O objetivo desse estudo é relatar a experiência adquirida com a utilização de MDAHs para o tratamento de pacientes com necessidade de cirurgia plástica reparadora.
MÉTODO: No período de fevereiro de 2011 a julho de 2014 foram utilizadas 5 diferentes MDAHs no tratamento de 24 lesões de diferentes etiologias, inclusive para 3 etiologias não descritas na literatura: rinofima, hidrosadenite supurativa e síndrome de Lyell (necrólise epidérmica tóxica-NET).
RESULTADOS: Os 20 pacientes de diferentes etiologias e que receberam o tratamento com enxerto de MDAH em diferentes regiões anatômicas, associados ou não à enxertia de pele autóloga, alcançaram a solução de suas patologias com adequados padrões funcionais e estéticos.
CONCLUSÃO: O emprego de MDAH pode ser considerado como alternativa no tratamento de diversos casos de difícil resolução e tem seu lugar na Cirurgia Plástica moderna, porém sua indicação deve ser bem avaliada devido ao alto custo do material.
Palavras-chave: Curativos biológicos; Retalhos cirúrgicos; Feridas; Cicatrização; Procedimentos cirúrgicos reconstrutivos/métodos.
Skin healing is a dynamic process and involves cellular interaction, the extracellular matrix (ECM), and growth factors that are responsible for the tissue reconstruction or healing that follows the injury process1-3.
The ECM plays an important role in tissue regeneration and is the largest component of the dermis. It is composed of proteoglycans, hyaluronic acid, collagen, fibronectin, and elastin4. It provides structural support for cells, and some of its components stimulate growth factors, which in turn, stimulate cell proliferation and migration during the processes of tissue repair2,3,5. In chronic lesions, inflammatory substances increase the levels of proteases, which degrade components of the ECM, stimulating the release of growth factors, proteins, and receptors that are essential for wound healing2,3,5.
The recognition of the importance of the ECM in the healing process and tissue repair has led the pharmaceutical industry to develop biomaterials that could stimulate or replace the ECM. These biomaterials, resulting from tissue engineering, mimic the structural and the functional characteristics of the natural ECM6.
Skin substitutes are a heterogeneous group of materials7. Most recently, biomaterials that can be used as wound bed covers, which function to replace the skin temporarily or permanently depending on the characteristics of the product, have been developed. These biological substitutes have an intact ECM structure that can be used definitively in the skin, retrieving its functional and aesthetic characteristics.
Biological skin substitutes should enable the formation of a new dermis and allow the reepithelialization steps to occur in a correct manner and concomitantly with the maintenance of the basal membrane. Synthetic skin substitutes have shown advantages in allowing a better control of the dosage of patch components.
Skin tissue engineering seeks to develop an ideal skin substitute that promotes the appropriate repair of wounds without the formation of scars8,9.
The loss of the total thickness of the skin has a tendency to transform complex lesions into chronic wounds with difficult healing, thus increasing the time of recovery of the patient without proper treatment. Moreover, some diseases or special conditions partially or fully affect the anatomical structures of the skin. Therefore, the objective of this study was to report the experience with the use of heterologous acellular dermal matrices (HADMs) to correct these conditions in patients requiring reconstructive plastic surgery.
METHODS
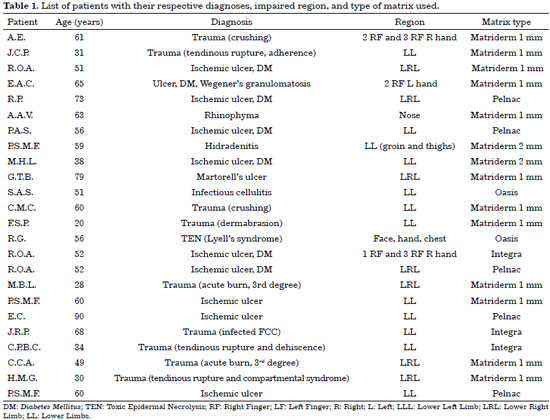
After the approval of the Council of Ethics and Research (register in the Plataforma Brasil: CAAE 37536614.6.0000.5455) and signing of the informed consent form, 20 patients (a total of 24 lesions) with different pathologies or ulcers affecting the skin in total or partial thickness, as well as other adjacent tissues, were treated. This study was carried out at the Hospital 9 de Julho, São Paulo, SP, from February 2011 to July 2014. Seventeen of the patients were men and three were women, with age between 20 and 90 years (mean, 53.5 years) (Figure 1). The lesions had different etiologies.

Figure 1. Infected ischemic ulcer with bone exposition - osteomelitis. A: Preoperative; B: Intraoperative with HADMs; C: 7 days after surgery; D: 20 days after surgery.
The largest sample comprised 10 patients with vascular problems. In this group, six patients had insulin-dependent diabetes mellitus (DM) (three had DM type I and three had DM type II), and one patient with DM type I also had chronic renal disease and was undergoing hemodialysis sessions three times per week. One additional patient had a diagnosis of associated rheumatologic disease (psoriatic arthritis) during treatment.
The etiology with the second largest proportion of patients was traumatic, with eight patients. There were also three cases of dermatological diseases (rhinophyma, hidradenitis suppurativa, and toxic epidermal necrolysis [TEN]), one case of infection (cellulitis), and one case of type II DM associated with Wegener's granulomatosis.
In relation to the location of the lesions, 16 patients had lesions in the foot and ankle, three had lesions in the thigh and leg, three had lesions in the fingers, and two had lesions on the face. In the patient with TEN (Lyell's syndrome), the eyelids, nose, forehead, hand, and the nipples were involved.
A total of 18 patients presented exposure of the tendon (17 patients), vessels (9 patients), nerves (6 patients), and bones (5 patients). Of this group, four patients had concomitant exposure of those four noble structures.
Table 1 presents the diagnosis of each patient, the specific location of the lesion, and the type of matrix used for each case.
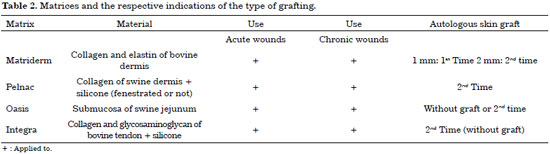
In our study, we used five types of HADM: Matriderm 1 mm, Matriderm 2 mm, Pelnac, Oasis, and Integra.
The specific characteristics of each HADM are presented in Table 2.
To be eligible for grafting with HADM, patients need to present a receptor bed with good perfusion, free of necrotic tissues and without infection or colonization.
In this case series, concomitant therapies were administered to reach this appropriate condition. All patients first received empirical antibiotic therapy; subsequently, with appropriate culture and antibiogram, 21 patients underwent sessions of hyperbaric oxygen therapy (HOT), 21 received nutritional supplementation, and 18 received dressings with negative pressure therapy (NPT).
In three cases, immediate application of the HADM (Matriderm 1 mm) was performed followed by grafting of concomitant autologous partial skin. In five cases, two previous surgeries were performed for the preparation of the receiver bed. In 15 cases, three or more interventions were necessary before the receiving area became adequate for grafting. Three of these cases with open wounds or dehiscence from a previous surgery were referred by other specialty teams.
After the HADM graft, the same material must be integrated to the receptor bed through the same processes of integration of an autologous graft: imbibition, inosculation, neoangiogenesis, and cell migration followed by remodeling2,3.
The only HADM that allows autologous skin grafting at the first surgical time is Matriderm 1 mm, owing to its reduced thickness. Therefore, in the other cases, it was necessary to wait for the integration of the HADM before performing the grafting, when scheduled.
Thus, surgical procedures were performed after the grafting of the HADM for both observing the evolution of the lesion and performing autologous skin grafting, for debridement, and for changing the dressings of NPT. Only one patient did not require surgery after the HADM graft. In five cases, one intervention was performed; in three cases, two interventions were needed; and in 11 cases, three or more interventions were done after the HADM graft. All rules of ethics in medical research were followed.
RESULTS
Five cases presented with complications: two patients had infection of the graft, two patients had trauma on the graft, and one patient presented with hemorrhage in the graft bed during tracheal extubation.
In the cases with infection, the grafts were debrided, samples were collected, and the surgical area was washed with chlorhexidine solution; thereafter, antibiotic therapy was adjusted when necessary. NPT was associated with dressings with silver, and dressing changes were performed every 2-3 days.
In the cases with trauma, one patient experienced a total loss of the grafts, and debridement and regrafting were required; in the other trauma case, the loss was partial and new grafting was also performed.
In the case with hemorrhage, the patient was immediately anesthetized and reintubated, and some fixing points of the autologous skin grafts were removed. Blood drain was maintained together with washing of the HADM with 0.9% solution of silk fibroin with epinephrine. The sutures and dressing were redone, and the patient was extubated in a more secure and slow manner.
In the cases with trauma, there was total loss of grafting in one case and loss of 50% of the area in the other case; in the two cases with infection, there was partial loss of < 10% of the grafted area; and in the case of hemorrhage, there was no loss of graft.
DISCUSSION
Advances in medicine have broadened the applications of plastic surgery. Many patients who until a few years ago would have had no therapeutic possibilities currently can benefit from new technologies and biomaterials such as the HADMs.
With the association of different therapies such as NPT10, nutritional supplementation, antibiotic therapy, and HOT, it is already possible to achieve functionally good and aesthetically acceptable results for many cases11.
In this series, we draw attention to the group of diabetic patients with vascular problems and who present lesions with exposure of vessels, tendon, bones, and nerves, for which there was no possibility of any type of safe coverage with skin grafts (because of the exposed structures), flaps, or even microsurgery (owing to diabetic angiopathy).
In one case in this group of diabetic patients, the patient was undergoing dialysis and had developed necrosis in the fingertips due to needle punctures for glycemia checks. After the grafting of HADM (in this case, Integra) associated with silicone dressing impregnated with silver (Mepilex Ag) under compression, even without the association of autologous partial skin graft in a second surgical moment, the patient presented excellent evolution of the lesion, with far superior functional and aesthetic quality than expected. This suggests the possibility of the existence of other factors in HADMs that stimulate the growth of tissues (Figure 2).

Figure 2. Post-puncture injury to perform glycemic index test. A: Preoperative; B: Intraoperative; C: 30 days after surgery.
In patients with trauma involving the vessels, joints, tendons, nerves, and bones, it was possible, with less invasive procedures, to obtain equal or better functional and aesthetic outcomes than those achieved with flaps of any nature.
It must also be taken into account that the morbidity of the donor areas of cutaneous, muscular, and myocutaneous flaps, most of the times, is much greater than that of the donor area of partial skin grafts, both from the aesthetic and functional viewpoints.
In reconstructions of the foot and ankle, flaps often result in a large increase in the volume of the area, which entails locomotion problems in addition to need for special footwear owing to the resulting deformities.
In the case with rhinophyma, the results thus far indicate that the use of HADM was a definitive treatment, as the altered tissue was totally removed and replaced by the HADM (Matriderm 1 mm) associated with skin grafts at the same surgical time, preserving the aesthetic subunits of the nose and reaching very favorable functional and aesthetic results that are closest to normality than those presented by the current methods12. The patient of this case has been followed for 3 years, with preserved results and without recurrence (Figure 3).

Figure 3. Rhinophyma - before and after intervention. A: Preoperative; B: 60 days after surgery.
In the case with hidradenitis, the reconstruction with HADM associated with autologous partial skin grafting in mesh form had no precedent in the literature for this pathology, although there have been reports on its application for the sequelae of burn injury in the upper thighs. This method was indicated for the patient who had aseptic necrosis of the femoral head and who was unsuitable for orthopedic treatment with hip prosthesis because of constant infections in the groin and upper thighs. The patient also had a history of severe obesity and smoking (> 60 cigarettes/day).
Because of the extension of the areas, there was no possibility of using local flaps; moreover, microsurgical procedures were also risky owing to the patient's smoking habit. The use of grafts without HADM could lead to scar retraction in the groin and upper thighs. Owing to the extension, the patient had insufficient donor area for total skin graft.
Sheets of HADM (Matriderm 2 mm) were used, associated with autologous partial skin graft expanded at a ratio of 1:2. Dressing with NPT was completed. The patient is being followed since December 2011, continues to smoke, and by the end of July 2014, presented no recurrence of hidradenitis in the area, only small ulcerations that healed when the number of cigarettes was reduced. Moreover, no cicatricial retraction was noted on palpation during physical examination (Figure 4).

Figure 4. Hidradenitis - before and after intervention. A: Preoperative; B: Intraoperative after resection; C: HADMs; D to F: Bandage; G: Bandage opening; H: 7 days after surgery; I: 30 days after surgery.
There is no similar report in the literature for the application of HADM (Oasis) in the case with Lyell's syndrome or TEN; however the pathophysiology of this disease and the histological characteristic of lesions indicated the use of the matrix without the association of autologous skin graft, resulting in the rapid recovery of the epithelium of the eyelids, fingers, nose, forehead, and nipples. The stimulus of epithelization prevented hypergranulation, minimizing the risk of functional and aesthetic sequelae in these regions. In this case, low-intensity diode laser treatments were administered in the intraoperative period together with sessions of HOT, which also contributed to a good outcome in less time than usual for the healing of wounds of this thickness (Figure 5).

Figure 5. Lyell's syndrome. A: Intraoperative with HADMs; B: 45 days after surgery.
CONCLUSION
In unprecedented cases, the results obtained were very satisfactory; however, it will be necessary to carry out studies with larger samples to prove the efficacy and reproducibility of the treatment.
In reconstructions, a multicenter trial will define the precise indications for the use of each type of HADM depending on the characteristics of each lesion or pathology.
In Brazil, only few costly HADMs are available. Nevertheless, the use of these materials is far simpler and more feasible than the development of a center or the training of a team for microsurgeries.
Furthermore, the method is technically simpler and the surgery has a lower morbidity, in addition to the absence of morbidity at the donor area of grafts, than flaps.
We believe that greater commercial competition will emerge in the Brazilian market, allowing the lowering of prices in the coming years, thus providing greater access to this material. Thereby, it will be possible for more number of surgeons to acquire experience in using this resource, benefiting all patients with injuries that may need this therapy, as well as patients with complex lesions and those who are admitted to centers without the possibility of performing microsurgeries.
ACKNOWLEDGMENTS
I would like to thank God for having blessed me and guiding me in all moments of my life. To my patients, who placed their trust and hope in the treatment. Together, we overcame adversities and reached the goal. To Vania Declair, my wife, for her dedication, love, and patience for me. To Denise, my secretary, for her promptness with my needs.
REFERENCES
1. Clark RA, Ghosh K, Tonnesen MG. Tissue engineering for cutaneous wounds. J Invest Dermatol. 2007;127(5):1018-29.
2. Clark RA. Basics of cutaneous wound repair. J Dermatol Surg Oncol. 1993;19(8):693-706.
3. Young A, McNaught CE. The physiology of wound healing. Surgery. 2011;29(10):475-9.
4. Schultz GS, Wysocki A. Interactions between extracellular matrix and growth factors in wound healing. Wound Repair Regen. 2009;17(2):153-62.
5. Gibson D, Cullen B, Legerstee R, Harding KG, Schultz G. MMPs Made Easy. Wounds International. 2009;1(1):1-6. [Acesso 15 Dez 2015]. Disponível em: http://www.woundsinternational.com/media/issues/61/files/content_21.pdf
6. Calne S, ed. International Consensus. Acellular matrices for the treatment of wounds. An expert working group review. London; Wounds International, 2010.
7. Ferreira MC, Paggiaro AO, Isaac C, Teixeira Neto N, Santos GB. Substitutos cutâneos: conceitos atuais e proposta de classificação. Rev Bras Cir Plást. 2011;26(4):696-702.
8. Mashreky SR, Bari S, Sen SL, Rahman A, Khan TF, Rahman F. Managing burn patients in a fire disaster: Experience from a burn unit in Bangladesh. Indian J Plast Surg. 2010;43(Suppl):S131-5.
9. Nicoletti G, Brenta F, Bleve M, Pellegatta T, Malovini A, Faga A, et al. Long-term in vivo assessment of bioengineered skin substitutes: a clinical study. J Tissue Eng Regen Med. 2015;9(4):460-8.
10. Aldunate JLCB, Vana LPM, Fontana C, Ferreira MC. Use of dermal matrix and negative pressure dressings for the treatment of contractures in burn patients. Rev Bras Cir Plást. 2012;27(3):369-73.
11. Santos AC, Menezes JA, Pimenta PS, Fabrini H, Sobreira JP, Ruback MC. Nova abordagem no tratamento de feridas complexas. Rev Bras Cir Plást. 2013:28(supl):1-10.
12. Costa TC, Firme WAA, Brito LMR, Vieira MBG, Leite LAS. Rinofima: opções cirúrgicas utilizadas no Serviço de Cirurgia Plástica do Hospital Agamenon Magalhães - PE. Rev Bras Cir Plást. 2010;25(4):633-6.
1. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
2. American Society of Plastic Surgeons, Arlington Heights, IL, USA
3. European Wound Management Association, Frederiksberg, Denmark
4. Universidade de São Paulo, São Paulo, SP, Brazil
5. Hospital 9 de Julho, São Paulo, SP, Brazil
Institution: Consultório Particular Hospital Nove de Julho, São Paulo, SP, Brazil.
Corresponding author:
Luiz Gustavo Balaguer Cruz
Rua Mendonca Furtado, 665
Cotia, SP, Brazil Zip Code 06706-135
E-mail: cirplastica@hotmail.com.br
Article received: August 6, 2014.
Article accepted: November 17, 2014.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter