

Review Article - Year 2016 - Volume 31 -
Trichilemmal carcinoma, an uncommon tumor: update on its management and prognosis
Carcinoma triquilemal, um tumor incomum: atualização sobre manejo e prognóstico
ABSTRACT
INTRODUCTION: Trichilemmal carcinoma (TC) is a rare neoplasm of skin appendages. It was first described in 1968 as tricoleptocarcinoma, and has an incidence of 0.05% in patients subjected to histopathological examination after excision of cutaneous lesions. TC has an indolent clinical course ; however, reports in the literature put in doubt this indolent behavior.
OBJECTIVES: To provide an update on the management and prognosis of TC.
METHODS:A search of the PubMed and SciELO databases by using with the MeSH terms "trichilemmal carcinoma", "tricholemmal carcinoma", "adnexal skin tumor", and "carcinoma triquilemal" was performed.
RESULTS: Owing to the rarity of TC, most studies were case reports, which essentially corroborate the indolent nature of the disease. Surgical excision is the recommended treatment, and is associated with a low risk of recurrence and low morbidity and mortality.
CONCLUSION: The behavior of the lesion and the procedure of treatment of TC are based on isolated cases or in a small series of cases. Because of its low prevalence, a multicenter collaboration of a greater number of cases can help define the best treatment recommendations, pathophysiology, and prognosis. Surgical excision remains the gold standard of treatment, and is associated with a low risk of recurrence.
Keywords: Scalp; Oncology; Skin neoplasms; Carcinoma of skin appendages; Neoplasms of adnexal and skin appendages; Prognosis.
RESUMO
INTRODUÇÃO: O carcinoma triquilemal (CT) é uma neoplasia rara dos anexos cutâneos. Foi descrito pela primeira vez em 1968, como tricoleptocarcinoma, e tem incidência de 0,05% em pacientes submetidos a exame histopatológico após excisão de lesões cutâneas. Parece ser um tumor de baixa agressividade, porém, relatos na literatura colocam em dúvida tal comportamento indolente.
OBJETIVOS: Oferecer uma atualização sobre manejo e prognóstico do CT.
MÉTODOS: Pesquisa no PubMed e SciELO com os termos MeSH "trichilemmal carcinoma", "tricholemmal carcinoma", "adnexal skin tumor", "carcinoma triquilemal".
RESULTADOS: Devido a sua raridade, a maior parte da literatura se baseia em relatos de caso, os quais na sua maioria corroboram a natureza indolente da doença. Excisão cirúrgica é o tratamento preconizado, com baixo risco de recidiva e baixa morbimortalidade.
CONCLUSÃO: O comportamento da lesão e as condutas no tratamento do CT baseiam-se em casos isolados ou de pequenas séries de casos. Devido a sua baixa prevalência, uma colaboração multicêntrica agrupando um maior número de casos pode ajudar a definir melhor recomendações de tratamento, fisiopatologia e prognóstico. Excisão cirúrgica continua a ser o padrão-ouro de tratamento, com baixo risco de recidiva.
Palavras-chave: Couro cabeludo; Oncologia; Neoplasias cutâneas; Carcinoma de apêndice cutâneo; Neoplasias de anexos e de apêndices cutâneos; Prognóstico.
Trichilemmal carcinoma (TC) is a rare neoplasm of the skin appendages, originating from the external root sheath of hair follicles. TC occurs primarily in sun-exposed skin areas such as the scalp, forehead, neck, torso and upper limbs, usually among elderly individuals, predominantly in women1.
It was first described in 1968 as tricoleptocarcinoma, and occurred in 0.05% of patients that were subjected to histopathological examination of excised cutaneous lesions2. Headington was the first to propose the term TC in 1976 to describe a "histologically invasive, cytologically atypical clear cell neoplasm of adnexal keratinocytes which is in continuity with the epidermis and/or follicular epithelium"3.
It seems to be an indolent tumor; however, reports in literature put in doubt this indolent behavior.
OBJECTIVE
The objective of this report was to provide an update on the management and prognosis of patients with TC through a literature review.
METHODS
A search was performed in the PubMed and SciELO online databases bhy using the MeSH terms "trichilemmal carcinoma", "tricholemmal carcinoma", "adnexal skin tumor", and "carcinoma triquilemal". Articles in Portuguese and English were assessed for eligibility.
DISCUSSION
TC occurs predominantly in the scalp, and shows a higher incidence in women and people of Caucasian ethnicity, generally in those between the fourth and sixth decade of life4,5. Skin areas with greater sun exposure, burns, or those subjected to previous irradiation have higher susceptibility to TC6. The lesions are usually smaller than 2 cm; however, some reported lesions reach up to 25 cm in diameter7 (Figure 1).

Figure 1. Clinical aspect of the lesion in the scalp of a 54-year-old woman, with one-year progression. Biopsy revealing a trichilemmal carcinoma.
A recent study has suggested that the description of TC in the literature as a well-characterized cutaneous neoplasia is exaggerated. This exaggeration may be due because the existence of other conditions that mimic TC are underestimated, including Bowen's disease8.
TC usually occurs as a solitary lesion9, predominantly in the head and neck regions10. Clinically, it appears approximately one year before diagnosis with a rapid growth rate11.
Differential diagnosis includes benign tricholemmal cyst, squamous cell carcinoma (Figures 2 and 3), basal cell carcinoma, keratoacanthoma, verrucous cysts, proliferative trichilemmal cysts, and pseudocarcinomatous cysts5,12.
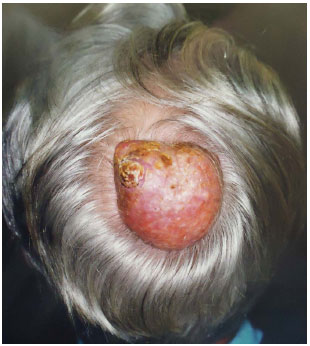
Figure 2. Friable, ulcerated lesion, of about 3 years of progression, in the scalp of a 71-year-old male patient. Histopathological analysis showing malignant proliferative trichilemmal tumor with squamous degeneration area (ulcerated area between 10 and 11 hours).
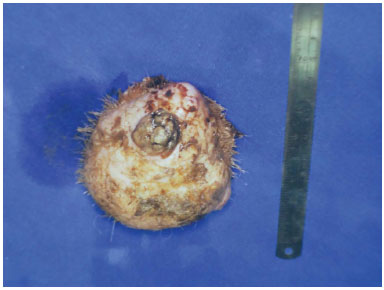
Figure 3. The surgical resection specimen of the lesion of Figure 2 (10 cm ruler for comparison).
The malignant portion of trichilemmoma seems to originate from the outer layer of the hair follicle13. Histologically, TC seems to be an intermediate- to high-grade neoplasia, and represents a lobular proliferation centered on the pilosebaceous unit and composed of clear and pale cells with atypia, containing glycogen with basilar invasion or total thickness of the interfollicular epidermis14. The growth of the tumor is lobular and infiltrative, with the lobules frequently centered and expanding the pilosebaceous unit. The initial intraepithelial impairment may extend to the reticular dermis. Actinic damage has been reported as a common feature11; nevertheless, there are reports of tumors in areas without sun exposure. No criterion for universal histopathological diagnosis has been established for TC15.
The prognosis depends on the size of the tumor and the location, the degree of differentiation, and the histological subtype. In an analysis of 615 patients with squamous cell carcinomas (with behavior similar to TC), the key prognostic factors for metastasis were increase in tumor depth (> 2 mm), immunosuppression, lesion in the ear, and increased superficial diameter (> 6 mm)16.
Despite its aggressive cytological appearance, TC represents an indolent tumor that usually evolves with a benign course and is associated with good clinical prognosis3 and nonmetastatic potential16,17.
However, there are several studies in literature reporting TCs with an aggressive course, with local lymph node invasion9,18,19, recurrence19, and even metastasis20,21, and thus, the actual behavior of the lesion is questionable. In a recent series of 26 patients, survival at 5 years was 89.5%5. There is no standardized chemotherapy treatment for TC, but in reports of patients with recurrent tumors or metastases, regimes including cisplatin, cyclophosphamide, and adriamycin (similar to the one used for patients with advanced cases of squamous cell carcinoma) have shown control of tumor growth; however, cure was not attained5,19.
Similar to information on the course of the lesion, there are discrepancies in the literature regarding the treatment of TC. Complete surgical excision with histological documentation of free margins is recommended as the standard treatment by some authors4, which can be obtained using Mohs micrographic surgery19. Others, however, recommend a wide surgical excision18.
Adjuvant radiotherapy is requested for high-risk cases, when complete resection is impossible, or in cases of recurrence or metastasis22.
CONCLUSION
We can conclude that most of the information on the behavior and approach of the treatment of TC are based on isolated cases or small series of cases. Owing to the low prevalence of these tumors, larger and prospective studies are required to delineate the actual behavior of this lesion, since the behavior differs substantially from the indolent behavior, as described by a large number of authors.
Surgical excision with 1 cm margin is safe and simple, and is associated with a low risk of recurrence. It is important to discuss and warn the patient about the possibility of recurrence and, in cases of recurrent or aggressive tumors, multidisciplinary follow-up, including close liaison with the oncologist for adjuvant treatment, is essential.
REFERENCES
1. Sau P, Graham JH, Helwig EB. Proliferating epithelial cysts. Clinicopathological analysis of 96 cases. J Cutan Pathol. 1995;22(5):394-406. DOI: http://dx.doi.org/10.1111/j.1600-0560.1995.tb00754.xhttp://dx.doi.org/10.1111/j.1600-0560.1995.tb00754.x
2. Holmes EJ. Tumors of lower hair sheath. Common histogenesis of certain so-called "sebaceous cysts," acanthomas and "sebaceous carcinomas". Cancer. 1968;21(2):234-48. PMID: 4952501 DOI: http://dx.doi.org/10.1002/1097-0142(196802)21:2<234::AID-CNCR2820210211>3.0.CO;2-J
3. Headington JT. Tumors of the hair follicle. A review. Am J Pathol. 1976;85(2):479-514.
4. Feng Z, Zhu HG, Wang LZ, Zheng JW, Chen WT, Zhang Z, et al. Tricholemmal carcinoma of the head and neck region: A report of 15 cases. Oncol Lett. 2014;7(2):423-6.
5. Zhuang SM, Zhang GH, Chen WK, Chen SW, Wang LP, Li H, et al. Survival study and clinicopathological evaluation of trichilemmal carcinoma. Mol Clin Oncol. 2013;1(3):499-502.
6. Billingsley EM, Davidowski TA, Maloney ME. Trichilemmal carcinoma. J Am Acad Dermatol. 1997;36(1):107-9. PMID: 8996274 DOI: http://dx.doi.org/10.1016/S0190-9622(97)70339-6
7. Casas JG, Woscoff A. Giant pilar tumor of the scalp. Arch Dermatol. 1980;116(12):1395. PMID: 7458368 DOI: http://dx.doi.org/10.1001/archderm.1980.01640360069021
8. Dalton SR, LeBoit PE. Squamous cell carcinoma with clear cells: how often is there evidence of tricholemmal differentiation? Am J Dermatopathol. 2008;30(4):333-9.
9. Boscaino A, Terracciano LM, Donofrio V, Ferrara G, De Rosa G. Tricholemmal carcinoma: a study of seven cases. J Cutan Pathol. 1992;19(2):94-9. DOI: http://dx.doi.org/10.1111/j.1600-0560.1992.tb01349.x
10. Stang A, Stegmaier C, Jöckel KH. Nonmelanoma skin cancer in the Federal State of Saarland, Germany, 1995-1999. Br J Cancer. 2003;89(7):1205-8. PMID: 14520447 DOI: http://dx.doi.org/10.1038/sj.bjc.6601294
11. Swanson PE, Marrogi AJ, Williams DJ, Cherwitz DL, Wick MR. Tricholemmal carcinoma: clinicopathologic study of 10 cases. J Cutan Pathol. 1992;19(2):100-9. DOI: http://dx.doi.org/10.1111/j.1600-0560.1992.tb01350.x
12. Van Zele D, Arrese JE, Heymans O, Fissette J, Piérard GE. Invasive tricholemmal carcinoma of the nose. Dermatology. 2002;204(4):315-7. PMID: 12077536 DOI: http://dx.doi.org/10.1159/000063374
13. Reis JP, Tellechea O, Cunha MF, Baptista AP. Trichilemmal carcinoma: review of 8 cases. J Cutan Pathol. 1993;20(1):44-9. DOI:http://dx.doi.org/10.1111/j.1600-0560.1993.tb01248.x
14. Elder DE, ed. Lever's histopathology of the skin. Philadelphia: Lippincott Williams & Wilkins; 2009.
15. Misago N, Toda S, Narisawa Y. Folliculocentric squamous cell carcinoma with tricholemmal differentiation: a reappraisal of tricholemmal carcinoma. Clin Exp Dermatol. 2012;37(5):484-91. DOI: http://dx.doi.org/10.1111/j.1365-2230.2012.04366.x
16. Brantsch KD, Meisner C, Schönfisch B, Trilling B, Wehner-Caroli J, Röcken M, et al. Analysis of risk factors determining prognosis of cutaneous squamous-cell carcinoma: a prospective study. Lancet Oncol. 2008;9(8):713-20. DOI: http://dx.doi.org/10.1016/S1470-2045(08)70178-5
17. Folpe AL, Reisenauer AK, Mentzel T, Rütten A, Solomon AR. Proliferating trichilemmal tumors: clinicopathologic evaluation is a guide to biologic behavior. J Cutan Pathol. 2003;30(8):492-8. DOI: http://dx.doi.org/10.1034/j.1600-0560.2003.00041.x
18. Nemetz MA, Cunha RM, Reeck P, Carreirão Neto W, Moreira MTS, Coelho MS. Carcinoma triquilemal: relato de um caso. Rev Bras Otorrinolaringol. 2004;70(6):832-5. DOI: http://dx.doi.org/10.1590/S0034-72992004000600022
19. Roismann M, Freitas RR, Ribeiro LC, Montenegro MF, Biasi LJ, Jung JE. Carcinoma triquilemal: relato de caso. An Bras Dermatol. 2011;86(5):991-4. DOI: http://dx.doi.org/10.1590/S0365-05962011000500019
20. Dailey JR, Helm KF, Goldberg SH. Tricholemmal carcinoma of the eyelid. Am J Ophthalmol. 1993;115(1):118-9. PMID: 8420367 DOI: http://dx.doi.org/10.1016/S0002-9394(14)73540-8
21. Jung J, Cho SB, Yun M, Lee KH, Chung KY. Metastatic malignant proliferating trichilemmal tumor detected by positron emission tomography. Dermatol Surg. 2003;29(8):872-4.
22. Wollina U, Bayyoud Y, Kittner T, Dürig E. Giant tricholemmal squamous cell carcinoma with cranial infiltration. J Clin Aesthet Dermatol. 2011;4(4):34-7.
1. Pontifícia Universidade Católica do Rio Grande do Sul, Porto Alegre, RS, Brazil
2. Universidade Federal do Rio Grande do Sul, Porto Alegre, RS, Brazil
Institution: Serviço de Cirurgia Plástica Hospital São Lucas da Pontifícia Universidade Católica do Rio Grande do Sul (PUCRS) Porto Alegre, RS, Brazil.
Corresponding author:
Pedro Salomão Piccinini
Avenida Ipiranga, 6690, Jardim Botânico
Porto Alegre, RS, Brazil Zip Code 90610-000
E-mail: pspiccinini@gmail.com
Article received: March 26, 2015.
Article accepted: October 8, 2015.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter