

Case Report - Year 2016 - Volume 31 -
Applicability of the pedicled anterolateral thigh flap in complex reconstructions of the abdominal wall in oncology: report of 2 cases
Aplicabilidade do retalho anterolateral da coxa pediculado nas reconstruções complexas da parede abdominal em oncologia: relato de 2 casos
ABSTRACT
INTRODUCTION: There is a strong commitment in pursuing reconstructive solutions for areas of skin or muscular loss that require covering or stable cavity filling. The anterolateral thigh flap, described in China by Song et al. (1984), is considered by many as the optimal flap in large reconstructions.
OBJECTIVE: To report the applicability of the anterolateral thigh flap, as a versatile resource in reconstructions of the abdominal wall.
METHODS: Two patients were submitted to tumoral resection of the right colon with invasion of the abdominal wall by a team of oncologic surgeons in conjunction with the plastic surgery team that was responsible for the reconstruction of the abdominal wall. In both cases, the pedicled anterolateral thigh flap was used, which was transposed to the defect after partial resection of the abdominal wall at the same surgical time. A PROCEEDTM surgical mesh was fixed between the abdominal viscera and the flap to reinforce the abdominal wall.
RESULTS: Both patients had good postoperative evolution and are in follow-up, with no signs of tumor recurrence and with a good quality of life.
CONCLUSION: The anterolateral thigh flap is a useful resource for the reconstruction of the abdominal wall due to large tumor resections in oncology.
Keywords: Oncology; Surgical flaps; Reconstructive surgical procedures; Thighs; Abdominal wall/Surgery.
RESUMO
INTRODUÇÃO: Há um grande empenho na busca por soluções reconstrutivas para as áreas de perda cutânea ou muscular que exijam cobertura ou preenchimento cavitário estável. O retalho anterolateral da coxa, descrito na China por Song et al. (1984), é considerado por muitos como o retalho ideal nas grandes reconstruções.
OBJETIVO: Relatar a aplicabilidade do retalho anterolateral da coxa como recurso versátil nas reconstruções da parede abdominal.
MÉTODOS: Dois pacientes foram selecionados para serem submetidos à ressecção tumoral de cólon direito com invasão da parede abdominal pela equipe de cirurgia oncológica em conjunto com a equipe de cirurgia plástica, que foi a responsável pela reconstrução da parede abdominal. Em ambos os casos, utilizou-se o retalho anterolateral da coxa pediculado, que foi transposto para o defeito após a ressecção parcial da parede abdominal no mesmo tempo cirúrgico. Entre as vísceras abdominais e o retalho, foi fixada tela de PROCEEDTM para reforço da parede abdominal. Resultados: Ambos os pacientes tiveram boa evolução pós-operatória e encontram-se em acompanhamento, sem sinais de recidiva tumoral e com boa qualidade de vida.
CONCLUSÃO: O retalho anterolateral da coxa mostrou-se recurso útil dentro do arsenal terapêutico reconstrutivo da parede abdominal devido a grandes ressecções tumorais em oncologia.
Palavras-chave: Oncologia; Retalhos cirúrgicos; Procedimentos cirúrgicos reconstrutivos; Coxas; Parede abdominal/Cirurgia.
There is a strong commitment in pursuing reconstructive solutions for areas of skin or muscular loss requiring covering or stable cavity filling, leading to studies with perforator flaps. One of the most important perforator flaps is the anterolateral thigh flap, described in China by Song et al. (1984)1, and considered by many as the optimal flap in large reconstructions. It has become popular in recent years due to its great versatility for reconstructions of defects in the head and neck region, the torso, and limbs2, either in the form of local or distant transfers (microsurgery)3.
In cases of complex defects of the abdominal wall, it is necessary to restore the containment function and abdominal press, avoiding convexities or herniation. The anterolateral thigh flap confers advantages from a reconstructive point of view: it fixes the flaws of the lower abdominal wall with a satisfactory volume of fascial tissue (from the thigh) and with a good rotation arc and range. The skin flap area is supplied by the septocutaneous or musculocutaneous perforator arteries of the descending branches of the lateral femoral circumflex artery. However, due to the large anatomical variety of its pedicle, it is paramount, before starting the dissection, to perform a simple sweep with unidirectional Doppler, to map perforator vessels that assists in the ideal location of the cutaneous island for better vascularization (maintain vessels mapped in the center of the island, diametrically) and the possibility of inclusion of other tissues to help in repair4.
OBJECTIVE
To report the applicability of the anterolateral thigh flap as a versatile resource in reconstructions of complex defects of the abdominal wall due to advanced tumors of the right colon - a report of two cases from the Barretos Cancer Hospital (HCB), Pius XII Foundation.
Technical considerations
The shape and dimensions of the flap were measured using a sterile absorbent paper mold. After being placed on the wound (receiving area), it became impregnated with its fluids, marking on paper the shape of the defect, which was then cut and transferred.
The repair of deep wounds in the abdominal wall was performed by fixing a PROCEEDTM surgical mesh5,6.
The superficial wound on the abdominal wall is repaired by application of the flap. After locating and demarcating the perforator vessels of the lateral femoral circumflex artery (LFCA) preoperatively, the flap can be delimited on the anterolateral surface of the thigh. The dissection is continued with the incision and elevation of the cutaneous island in the subfascial layer, up to the identification of the perforator vessels, which are followed and isolated in their septocutaneous or intramuscular trajectory up to the descendant or transverse branches of the LFCA, which in turn is individualized up to its origin in the deep femoral artery. After connecting the collateral branches, the flap is prepared for transfer, either locally or distally (microsurgery). The donor area, depending on the size, can be repaired with primary sutures or joined and complemented with skin grafts7.
CASE REPORT
Case 1 (Figures 1, 2, 3, 4 e 5)
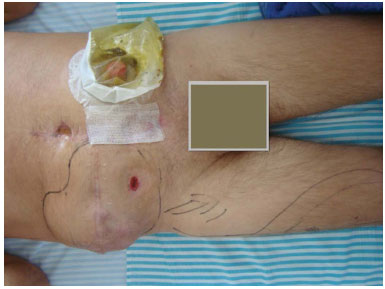
Figure 1. Case 1 (RFC): Pre-operative aspect.

Figure 2. Case 1 (RFC): Initial repair with a PROCEEDTM mesh.

Figure 3. Case 1 (RFC): Dissection of the pedicled anterolateral thigh flap.

Figure 4. Case 1 (RFC): Immediate postoperative aspect.

Figure 5. Case 1 (RFC): Late postoperative period.
RFC, white, 37-years-old man, single, born and domiciled in Alta Floresta, MT, with a history of exploratory laparotomy in the city of origin, for the treatment of acute appendicitis, which resulted in the finding of a tumor in the right colon. In the recent postoperative period, a nodule was identified on the surgical wound, and the patient was submitted for a second exploratory laparotomy with resection of the tumor and right colostomy. This evolved with intestinal obstruction, followed by a third surgical intervention, exploratory laparotomy, this time isolating the colon and performing an ileostomy in the lower left quadrant of the abdomen.
The patient was admitted to the HCB in July 2009 with complaints of abdominal pain, nausea, vomiting, diarrhea, asthenia, anorexia, weight loss, dyspnea, and chest pain upon breathing. The patient is a known smoker and drinker and has no family history of cancer or clinical and/or surgical history. A physical examination showed a midline infra supra-umbilical abdominal incision, ileostomy in the lower left quadrant, and tumor growth on the appendectomy scar in the right lower quadrant.
The patient was evaluated by a multidisciplinary team and submitted to a block resection of the tumor mass that encompassed the terminal ileum, right colon, sigmoid colon, and the entire wall of the right hemiabdomen. The abdominal cavity showed no tumor growth, and the liver was free of metastatic lesions. The transverse colon remained closed (free of intestinal transit), segmental sigmoidectomia was held with latero-lateral primary anastomosis with a double stapling technique, and the terminal ileostomy was rebuilt in the lower left quadrant of the abdomen.
A surgical complication was liver laceration, which required compression and the use of a hemostatic material (Surgicel®) to resolve. In addition, there was a partial lesion of the right femoral nerve during resection of the tumor, which required a suture of the nerve with Prolene 5.0.
The abdominal wall was reconstructed using a PROCEEDTM mesh (a thin laminated surgical mess, sterile, and flexible, which is used for the repair of hernias and other fascial lesions). The mesh is composed of a tissue of regenerated oxidized cellulose (ROC), a flexible Prolene® layer, and a layer of networked non-absorbable polypropylene that is encapsulated by a polidioxanone polymer. The surface of the polypropylene product allows the internal growth of the tissue, while the ROC side provides a bio-absorbable layer that physically separates the polypropylene network from the underlying tissue and the surface of organs during the healing period to minimize the adhesion of the tissues to the network.
A pedicled fasciocutaneous anterolateral thigh flap was overlaid on the mesh, ipsilateral to the wound, transposed with a rotating arc of > 90° and < 180°, and fixed in the abdominal wall defect with Vicryl 3-0 subdermal sutures and simple running sutures with nylon 5-0. The donor area was left open, not to prolong the surgical time. Occlusive dressing of the bloody area (right thigh) was held with Purilon ® (hydrogel) and Adaptic (non-adhesive mesh), until complete epithelialization had occurred.
The patient's immediate post-operative period was spent in the ICU, and hospital discharge occurred on the 13th day post-surgery. The patient underwent adjuvant chemotherapeutic treatment ending in January 2011. Tumor recurrence was discovered by palpation in the right abdominal flank and visualized by computed tomography in the region corresponding to the right pararenal space, with the lesion infiltrating the oblique muscles.
In May 2011, the patient was submitted for surgical treatment to resect the tumor lesion in the retroperitoneum, and, in the same surgery, the intestinal transit was rebuilt with side-to-side anastomosis in the ileal segment and the transverse colon, using a double stapling technique. The patient was discharged on postoperative day 6. Currently, outpatient follow-up shows no signs of tumor recurrence.
Case 2 (Figures 6, 7, 8, 9 e 10)

Figure 6. Case 2 (JMP): Intraoperative. Details of the dimensions of the tumor affecting the abdominal wall.
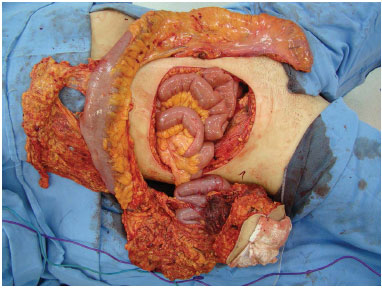
Figure 7. Case 2 (JMP): Surgical piece and the resulting defect.

Figure 8. Case 2 (JMP): Details of the fixing of the PROCEEDTM mesh and dissected flap.
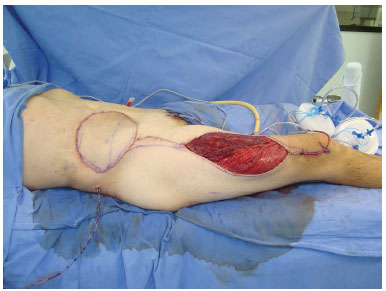
Figure 9. Case 2 (JMP): Immediate postoperative aspect.

Figure 10. Case 2 (JMP): Late postoperative aspect.
JMP, white, 48-years-old man, married, born and domiciled in Medeiros, MG, with a history of surgical treatment for acute appendicitis in October 2009, with the need for re-intervention for control of an infection at the surgical site. Colonoscopy and computed tomography of the abdomen was performed, which revealed a tumor in the right colon. When admitted to the HCB in November 2010, the patient was asymptomatic in the first consultation. The patient has no prior history of smoking, alcoholism, or other diseases and there is no prior history of cancer, or clinical and/or surgical history in the family.
An area of the surgical scar in the lower right quadrant of the abdomen with a granulomatous lesion was observed on physical examination. Submitted in December 2010 for a biopsy of this lesion, the pathology examination revealed a chronic inflammatory process with an absence of neoplastic cells. In a computed tomography examination on the same day, a bulky tumor mass of 10.1 x 6.6 cm was found, with central degeneration, located in the topography of the terminal ileum and cecum and extending to the abdominal wall up to the ulcerated area of the skin.
After the multidisciplinary evaluation, he was submitted in February 2011 for a total colectomy and a block resection of the tumor mass that encompassed the abdominal wall corresponding to the lower right quadrant. No tumor growths were present in the abdominal cavity, and the liver was free of metastatic lesions. An ileo-rectal-anastomosis was constructed using a circular stapling technique with intestinal stapler number 29. The abdominal wall was reconstructed using a PROCEEDTM mesh, and a pedicled anterolateral right thigh flap was superimposed on the mesh. The donor area was left open and treated with dressings, as in case 1. The patient's immediate postoperative period was spent in the ICU, and hospital discharge occurred on the 11th day post-surgery.
The patient underwent adjuvant chemotherapeutic treatment ending in December 2011. Currently, the patient is in outpatient care, with no signs of tumor recurrence.
DISCUSSION
According to literature, the preparation of the cutaneous territory of the flap can be wide, and a skin area of 25 cm by 18 cm can be achieved that can survive with only one perforator vessel8. Moreover, primary closure of the donor area is possible when the width is less than 9 cm. Larger defects require skin grafting, but in our cases, this procedure was not performed due to the patient's clinical condition and prolonged operative time.
If possible, multiple perforator vessels should be preserved in the flap, because although a broad area of the skin can be supplied by only one perforator vessel, they are extremely thin and thrombosis tends to occur quickly after the development of congestion9. By presenting a long pedicle, a good arc of rotation and range can be achieved, providing an excellent covering option for abdominal defects10. The transposition occurs in a simple manner, associated with the implementation of the PROCEEDTM mesh, which is required for internal reinforcement, aiding in both the containment of the abdominal viscera and avoiding herniation.
In the cases presented here, the aesthetic results were excellent, with restoration of the contour in the abdominal defective area, but were initially unsatisfactory for the donor areas. The same evolved with healing by second intention, and later acceptable with satisfactory epithelization.
CONCLUSION
The anterolateral thigh flap is a useful resource within the reconstructive therapeutic arsenal for large abdominal wall defects in oncology.
REFERENCES
1. Song YG, Chen GZ, Song YL. The free thigh flap: a new free flap concept based on the septocutaneous artery. Br J Plast Surg. 1984;37(2):149-59. PMID: 6713155 DOI: http://dx.doi.org/10.1016/0007-1226(84)90002-X
2. Chana JS, Wei FC. A review of the advantages of the anterolateral thigh flap in head and neck reconstruction. Br J Plast Surg. 2004;57(7):603-9. PMID: 15380693 DOI: http://dx.doi.org/10.1016/j.bjps.2004.05.032
3. Geddes CR, Morris SF, Neligan PC. Perforator flaps: Evolution, classification, and applications. Ann Plast Surg. 2003;50(1):90-9. PMID: 12545116 DOI: http://dx.doi.org/10.1097/00000637-200301000-00016
4. Ishida LC. Estudo anatômico do retalho perfurante ântero-lateral da coxa. [Tese de doutorado]. São Paulo: Faculdade de Medicina da Universidade de São Paulo; 2006. 86p.
5. Holste JL. Are meshes with lightweight construction strong enough? Int Surg. 2005;90(3 Suppl):S10-2. PMID: 16463941
6. Cobb WS, Kercher KW, Heniford BT. The argument for lightweight polypropylene mesh in hernia repair. Surg Innov. 2005;12(1):63-9. DOI: http://dx.doi.org/10.1177/155335060501200109
7. Bijos P, Zumiotti AV, Rocha JR, Ferreira MC. Microcirurgia Reconstrutiva. São Paulo: Atheneu; 2005. p.351-352.
8. Kimata Y, Uchiyama K, Ebihara S, Nakatsuka T, Harii K. Anatomic variations and technical problems of the anterolateral thigh flap: a report of 74 cases. Plast Reconstr Surg. 1998;102(5):1517-23. PMID: 9774005 DOI: http://dx.doi.org/10.1097/00006534-199810000-00026
9. Kimata Y, Uchiyama K, Ebihara S, Sakuraba M, Iida H, Nakatsuka T, et al. Anterolateral thigh flap donor-site complications and morbidity. Plast Reconstr Surg. 2000;106(3):584-9. PMID: 10987464 DOI: http://dx.doi.org/10.1097/00006534-200009010-00009
1. Colégio Brasileiro de Cirurgiões, Rio de Janeiro, RJ, Brazil
2. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
3. Instituto Nacional do Câncer, Rio de Janeiro, RJ, Brazil
4. International Confederation for Plastic Reconstructive and Aesthetic Surgery, Vienna, Austria
5. Hospital de Câncer de Barretos - Fundação Pio XII, Barretos, SP, Brazil
6. Universidade Estadual Paulista, São Paulo, SP, Brazil
7. Universidade Federal de São Paulo, São Paulo, SP, Brazil
8. Sociedade Brasileira de Coloproctologia, Rio de Janeiro, RJ, Brazil
9. IRCAD América Latina, Barretos, SP, Brazil
10. Universidade Federal de Goiás, Jataí, GO, Brazil
11. Hospital de Urgências de Goiânia, Goiânia, GO, Brazil
Institution: Hospital de Câncer de Barretos - Fundação Pio XII, Barretos, SP, Brazil.
Corresponding author:
Cleyton Dias Souza
Rua Alameda Holanda, 165
Barretos, SP, Brazil Zip Code 14784-001
E-mail: drcleytondias@gmail.com
Article received: August 4, 2012.
Article accepted: September 2, 2012.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter