

Case Report - Year 2016 - Volume 31 -
Meralgia paresthetica by compression from a modeling girdle
Meralgia parestésica por compressão de cinta modeladora
ABSTRACT
Meralgia paresthetica is characterized by pain, paresthesia or burning sensation, and reduction of tactile and pain sensitivity in the anterolateral surface of the thigh. This disability is caused by a neuropathy of the lateral femoral cutaneous nerve (LFCN). Conservative treatment is often successful at relieving the symptoms in the majority of patients. We describe the case of a 44-year-old patient who presented with these symptoms caused by postoperative use of a surgical girdle after aesthetic surgery.
Keywords: Paresthesia; Surgical girdle; Pain; Reconstructive surgical procedures; Thighs; Femoral neuropathy.
RESUMO
Meralgia parestésica é caracterizada por dor, parestesia ou queimação e diminuição da sensibilidade tátil e dolorosa na face anterolateral da coxa. Isto ocorre por uma neuropatia do nervo cutâneo femoral lateral (NCFL). O tratamento conservador é frequentemente bem-sucedido, aliviando os sintomas na maioria dos pacientes. Descrevemos o caso de uma paciente de 44 anos de idade que apresentou os sintomas descritos após uso pós-operatório de malha modeladora por cirurgia estética.
Palavras-chave: Parestesia; Malha cirúrgica; Dor; Procedimentos cirúrgicos reconstrutivos; Coxas; Neuropatia femoral.
Meralgia paresthetica (Bernhardt-Roth syndrome) was first described by a German neuropathologist, Martin Bernhardt (1844-1915), in 1878, but Wladimir Karlovich Roth (1848-1916), a Russian neurologist, coined the term meralgia paraesthetica, from the Greek words meros, for thigh, and algos, for pain1. Classically, meralgia paresthetica is described as a syndrome of dysesthesia or anesthesia in the distribution of the lateral femoral cutaneous nerve (LFCN), and is a compressive mononeuropathy (Figure 1)2.
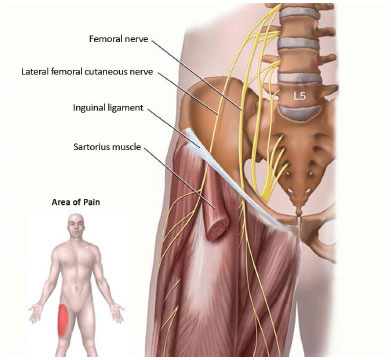
Figure 1. Anatomy of the inguinal region, lateral femoral cutaneous nerve2, Netter.
Source: Netter, F.H. Atlas de Anatomia Humana. 3ª edição Porto Alegre.
It is more common in men and is often characterized by a burning sensation in the anterolateral surface of the thigh. There is a sensation of discomfort in the affected area, but no motor and/or muscle strength abnormalities are observed. The reflexes are preserved, differentiating this condition from radiculopathies3.
This mononeuropathy can be caused by obesity, pregnancy, ascites, use of girdles, orthoses, and tight belts, direct trauma, scoliosis, differences in limb length, and muscle spasm. The LFCN can also be injured by abdominal or pelvic incisions, as during appendectomy or iliac bone graft harvesting. Compression can also occur within the pelvis, with reports of cases associated with uterine myoma, abscesses, retroperitoneal lipofibrosarcoma, and periostitis of the ilium. Laparoscopic inguinal hernia repair can also cause injury of the LFCN4.
The initial treatment of meralgia paresthetica is conservative, and patients may benefit from the use of analgesics, nonsteroidal anti-inflammatory drugs, use of loose clothing, weight loss, and the judicious use of steroids and local anesthetics. When conservative treatment fails, one must consider surgery, but there is no consensus on whether the best procedure is resection or decompression of the nerve at the lateral portion of the inguinal ligament1,3,4.
In the case reported herein, the left LFCN was compressed by a modeling girdle, with paresthesias beginning in the early postoperative period after lipoabdominoplasty and breast implantation.
CASE REPORT
A 44-year-old female underwent lipoabdominoplasty and breast implantation, and developed paresthesias and dysesthesias in the anterolateral surface of the thigh about 3 days after surgery. The patient reported that the modeling girdle was tight at the proximal bilateral thighs, but had no motor symptoms in the affected limb or cutaneous changes in the paresthesic area.
Electroneuromyographic assessment showed involvement of the left LFCN with moderate degeneration of sensory nerve fibers. There was no evidence of involvement of other peripheral nerves, myopathy, peripheral polyneuropathy, lumbosacral plexopathy, or proximal lumbosacral radiculopathy at the L2 to S1 levels bilaterally.
Nonsteroidal anti-inflammatory drugs were prescribed for 10 days, along with trimming of the modeling girdle, maintaining compression only above the anterior superior iliac crests, as well as avoiding activities involving hip extension. There was gradual improvement after 30 postoperative days. At 9 months postoperatively, the patient reported mild dysesthesias of the left side without other complaints.
DISCUSSION
Meralgia paresthetica has an estimated annual incidence of 4/10,000 people, and affects the purely sensory LFCN, which includes efferent sympathetic fibers that carry vasomotor, pilomotor, and sudomotor impulses. Its origin is variable and may be derived from several different combinations of lumbar nerves, including L2-L3, L1-L2, L2 alone, and L3 alone. The LFCN passes behind the psoas muscle, runs below the iliac fascia, and crosses the surface of the iliac muscle (Figure 12).
When the nerve approaches the anterior superior iliac spine, it penetrates the iliac fascia and emerges through a fibrous tunnel into the thigh5. Ghent6 described 4 variants in the course of the LFCN that compete for clinical presentation. In the first variant, the nerve passes through the inguinal ligament; in the second, there is a deformation of the nerve by a sharp ridge on the iliac fascia, which lies posterior to the nerve, causing compression when the patient is supine; in the third, it enters the sartorius muscle near the anterior superior iliac spine, and travels distally to the muscle before emerging beneath the fascia lata; and in the fourth variation, the LFCN penetrates the thigh, crossing the iliac crest lateral and posterior to the anterior superior iliac spine6.
Patients with meralgia paresthetica typically describe a burning, cold, shock-like, or sore sensation in the thigh, alteration in skin sensitivity, anesthesia, or local hair loss in the anterolateral thigh. The symptoms can be mild and fleeting, disappearing spontaneously, or intense, affecting the patient for years7. There may be a complaint of pain in the hip, knee, or calf, and patients modify their activities to minimize symptoms. Symptoms may worsen when the hip is extended; patients tend to avoid an upright position and report difficulty in sleeping. Sitting may alleviate the complaints in some people and worsen them in others.
In more intense cases, no position relieves the discomfort6. When it emerges superficially, the LFCN is susceptible to trauma and compression by obesity, pregnancy, ascites, girdles, orthoses, tight belts, direct trauma, scoliosis, differences in limb length, and muscle spasm. It can also be injured by abdominal or pelvic incisions, as during appendectomy or iliac bone graft harvesting. Compression can also occur within the pelvis, with reports of cases associated with uterine myoma, abscesses, retroperitoneal lipofibrosarcoma, and iliac periostitis.
Laparoscopic inguinal hernia surgery can cause injury of the LFCN4. The diagnosis is clinical, but additional tests, such as electroneuromyography, which shows reduction in speed of sensory conduction, tomography, magnetic resonance imaging, and ultrasonography, may be necessary to exclude other pathologies8.
The treatment is clinical in 90% of cases. Symptoms may regress spontaneously, but recurrence is common9. The initial treatment of meralgia paresthetica is conservative, and patients may benefit from analgesics, nonsteroidal anti-inflammatory drugs, use of loose clothing, weight loss, and the judicious use of steroids and local anesthetics. When conservative treatment fails, one must consider surgery, but there is no consensus, according to Grossman et al.10, on whether the best procedure is resection or decompression of the nerve at the lateral portion of the inguinal ligament.
CONCLUSION
The literature regarding follow-up and management is scarce1,3-7,10. In the present case, determination of the degree of inguinal compression caused by the elastic girdle was necessary. There was gradual improvement of the symptoms, with slight residual dysesthesias at 9 months postoperatively.
REFERENCES
1. Pearce JM. Meralgia paraesthetica (Bernhardt-Roth syndrome). J Neurol Neurosurg Psychiatry. 2006;77(1):84. PMID: 16361600 DOI: http://dx.doi.org/10.1136/jnnp.2005.072363
2. Meralgia parestesica: sintomi, segni, cause, diagnosi e trattamenti [Internet] [acesso 15 Fev 2016]. Disponível em: http://www.informazionimediche.com/2011/09/meralgia-parestesica-sintomisegni-cause-diagnosi-e-trattamenti.html
3. Erbay H. Meralgia paresthetica in differential diagnosis of low-back pain. Clin J Pain. 2002;18(2):132-5. DOI: http://dx.doi.org/10.1097/00002508-200203000-00010
4. Perry CP. Peripheral neuropathies and pelvic pain: diagnosis and management. Clin Obstet Gynecol. 2003;46(4):789-96. PMID: 14595220 DOI: http://dx.doi.org/10.1097/00003081-200312000-00008
5. Fabre T. Bébezis I, Bouchain J, Farlin F, Rezzouk J, Durandeau A. Meralgia Paresthetica: a rare cause of groin pain: surgical management of 119 cases between 1987 on 1999. Orthop Proc. 2004;86-B:SUPP I:40.
6. Ghent WR. Further studies on meralgia paresthetica. Can Med Assoc J. 1961;85:871-5.
7. Haim A, Pritsh T, Ben-Galim P, Dekel S. Meralgia Paresthetica: clinical experience with 79 patients. J Bone Joint Surg. 2005;87-B:SUPP III:393.
8. Sarala PK, Nishihara T, Oh SJ. Meralgia paresthetica: electrophysiologic study. Arch Phys Med Rehabil. 1979;60(1):30-1. PMID: 420568
9. Holanda MMA, Meira UM, Magalhães FNO, Silva JAG. Tratamento Cirúrgico da Meralgia Parestésica: relato de caso. Arq Neuropsiquiatr. 2003;61(2A):288-90. DOI: http://dx.doi.org/10.1590/S0004-282X2003000200026
10. Grossman MG, Ducey SA, Nadler SS, Levy AS. Meralgia paresthetica: diagnosis and treatment. J Am Acad Orthop Surg. 2001;9(5):336-44.
1. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
2. Hospital São Luiz, São Paulo, SP, Brazil
Institution: Clínica Privada de Dra. Dayana Garcia Alves, associada ao Serviço de Residência em Cirurgia Plástica Prof. Dr. Oswaldo de Castro.
Corresponding author:
Dayana Garcia Alves
Rua Vergueiro, 1353 cj 2001 - Vila Mariana
São Paulo, SP, Brazil Zip Code 04101-000
E-mail: dayana@dayanagarciaalves.com.br
Article received: August 25, 2012.
Article accepted: September 3, 2012.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter