

Original Article - Year 2016 - Volume 31 -
Importance of superficial circumflex iliac artery preservation to prevent abdominal wall necrosis in patients who underwent mini-abdominoplasty: an surgical-anatomic descriptive and prospective study
Importância da preservação da artéria ilíaca circunflexa superficial do abdome na prevenção das necroses da parede abdominal em pacientes submetidas a miniabdominoplastias: estudo anatômico cirúrgico descritivo prospectivo
ABSTRACT
INTRODUCTION: Abdominoplasty is the third most performed procedure in plastic surgery. To avoid surgical complications, a study of the superficial circumflex iliac artery of the abdomen (SCIA) was carried out to investigate the importance of this artery preservation in abdominoplasties as one of the high importance factors to prevent necrosis.
METHODS: This prospective study was carried out at the Plastic Surgery Service of the Agamenon Magalhaes Hospital. We included 33 patients who underwent abdominoplasty using Pitanguy's technique where the resected surgical flaps underwent hemodynamic studies to analyze the anatomical area irrigated by SCIA.
RESULTS: A total of 82 patients underwent surgery, of them 33 met the study inclusion criteria, and 6 (18.9%) were excluded for technical reasons. Patients' age ranged from 23 and 49 years (36.6±7.5), their body mass index (BMI) ranged from 22.0 to 30.5 (24.9 ± 2.1), and weight of resected surgical specimens ranged from 450 to 1010 grams (623.1 ± 141.5). Pearson's test between BMI and weight of surgical specimens showed significant correlation r = 0.91 and r2 = 0,83. We included in the study 32 women (97%) and 1 man (3%). One patient had hypertension (3%). Of the sample, 27 patients were pardo (81.8%), 2 white (6.1%), 3 black (9.1%) and 1 native south American (3.0%). In hemodynamic studies, images and videos obtained showed that injection of iodinated contrast in SCIA were considered adequate, and consistent with the objective of this study in 25 (92%) patients and inadequate for 2 (8%) patients.
CONCLUSION: Hemodynamic results of our study indicated that preservation of SCIA of the abdomen in mini-abdominoplasties is important to prevent necrosis of abdominal wall.
Keywords: Miniabdominoplasty, Abdominoplasty, Necrosis, hemodynamic, Anatomy.
RESUMO
INTRODUÇÃO: A abdominoplastia é o terceiro procedimento mais realizado em cirurgia plástica. Na intenção de evitar complicações cirúrgicas, foi feito o estudo da artéria ilíaca circunflexa superficial do abdome (AICS), investigando a importância da sua preservação nestas cirurgias, como um dos fatores de alta importância na prevenção das necroses.
MÉTODOS: O presente estudo anatômico prospectivo foi realizado no Serviço de Cirurgia Plástica do Hospital Agamenon Magalhães. Trinta e três pacientes foram submetidos à dermolipectomia abdominal à Pitanguy, com os retalhos cirúrgicos ressecados sendo submetidos a estudos hemodinâmicos para análise do território anatômico irrigado pela AICS.
RESULTADOS: Foram operados 82 pacientes, sendo selecionados 33 que preencheram os critérios de inclusão para este estudo, seis (18,9%) foram excluídos por motivos técnicos. O grupo de pacientes em estudo apresentou faixa etária entre 23 e 49 anos (36,6 ± 7,5). O Índice de Massa Corporal variou de 22,0 a 30,5 (24,9 ± 2,1). O peso das peças cirúrgicas ressecadas variou de 450 a 1010 gramas (623,1 ± 141,5), o teste de Pearson entre IMC e peso das peças demonstrou importante correlação r = 0,91 e r2 = 0,83. Trinta e dois eram femininos (97%) e um masculino (3%). Uma paciente era portadora de hipertensão arterial sistêmica (3%). Vinte e sete eram pardos (81,8%), dois brancos (6,1%), três negros (9,1%) e um da raça indígena (3,0%). Nos estudos hemodinâmicos, as imagens e filmes obtidos demonstraram que a injeção do contraste iodado na AICS foi considerada adequada, compatível com o objetivo do trabalho em 25 (92%) pacientes e inadequada em dois (8%) pacientes.
CONCLUSÃO: Os resultados hemodinâmicos deste estudo levam à conclusão que a preservação da AICS do abdome nas miniabdominoplastias tem relevante importância na prevenção das necroses da parede abdominal.
Palavras-chave: Abdominoplastia; Necrose; Hemodinâmica; Artéria ilíaca; Retalhos cirúrgicos; Cirurgia plástica.
Abdominoplasty is the third most performed procedure in plastic surgery and its prevalence is increasing, partly because of massive weight loss of patients1,2. An improved body contour leads to increased self-esteem, increase libido and sexual satisfaction3. To achieve these goals, surgeons are reaching the safety limits of techniques. Surgical complications may cause trauma both anatomically and psychologically. These complications are becoming more frequent, particularly those related to vascular supply4.
In mini-abdominoplasty the abdominal area that is detached compromises the largest axial skin flap in length, for this reason, surgery needs meticulous and careful actions5,6. Previous abdominal incisions, particularly subcostal, can compromise healing after abdominoplasty due to impaired blood supply in the upper abdomen. Abdominal scars in the middle line are common in individuals with massive weight loss, especially in patients who underwent intra peritoneal surgeries, such as Roux Y and gastric bypass surgery that in most cases incision is made in the supra umbilical region. Overestimate should be avoided in relation to wound healing of subcostal incisions in detachment of the abdominal wall, particularly those incisions made years ago7.
In traditional abdominoplasty, detachment with elevation of the abdominal flap extends up to the edge of subcostal region. This procedure compromises the blood supply to the central portion of the abdominal flap. This was described by Matarasso8 and Huger9. Matarasso described abdominal vascular supply into three zones. Zone I is the vascular supply to the central portion of abdomen, which is supplied by branches of the deep and superficial upper epigastric artery system. Zone II provide vascular supply to the inferior epigastric artery system, which is supplied by the deep circumflex iliac artery, the superficial circumflex iliac artery (SCIA), and the superficial pudendal artery. Zone III is irrigated by the subcostal, intercostal, and lumbar segmental perforators. The Matarasso10 study describes safe and unsafe areas for elevate flaps. During abdominoplasty, the zone II is traditionally resected and discarded, therefore, it is considered irrelevant. The deepest part of the blood supply to zone I is sectioned during the elevation of the abdominal flap. Matarasso also consider the intermediate area between zone I and zone III safe for lifting flap because marginal branches of the phrenic artery remain preserved after lifting.
In mini-abdominoplasties (type IV according to Bozola's classification), the detached flap has greater axial length than the conventional technique flap type V and its distal portion is more vulnerable to blood supply deficiency11-15.
The number of plastic surgery in the abdominal wall has increased and women demand even more aesthetic details16. For this reason, plastic surgeons are challenge to seek surgical techniques that sometimes can be catastrophic when patients suffer or experience vascular injury17.
OBJECTIVE
To avoid serious complications a study of the superficial circumflex iliac artery was carried out to investigate the importance of this artery preservation in mini-abdominoplasties and minilipoabdominoplasties18 as one of the most important factors to prevent necrosis of the abdominal wall, which is the most severe and feared complication.
METHODS
This prospective anatomical study was conducted at the Plastic Surgery Department of the Hospital Agamenon Magalhães, which is accredited by the Ministry of Education and Culture (MEC), and by the Brazilian Society of Plastic Surgery (SBCP). Surgeries was carried out at hospital surgical center and catheterization laboratory from August 2014 to July 2015. All patients were users of the Unified Health System (SUS, acronym in Portuguese), The study was approved by the Hospital's Medical Board of Plastic Surgery. Procedures was with body mass index (BMI) stable for six months and controlled blood pressure levels. We excluded patients who could not perform hemodynamic study, e.g., those with thrombosis or vascular injury.
The selected patients underwent abdominoplasty using the technique described by Pitanguy, with removal of flap for hemodynamic study according to the following protocol: Patients were admitted one day before the surgery with preoperative tests: blood count, glucose, urea, creatinine, coagulation, urinalysis, stool and cardiological evaluation. Upon admission, tests were checked and surgical procedure re-explained to the patient.
Upon arriving in the surgery center an anesthesiologist evaluated patients. After authorization, skin marking was carried out with dermographic pen by the surgical team. Subsequently pre-operative care started with the placement of intermittent pneumatic compression, padding on the upper limbs and placement of urinary catheter with closed system shortly after spinal block anesthesia.
The patient was positioned in dorsal decubitus, and the skin was prepared with chlorhexidine, drapes placement.
After, marking was done with bright green over the previous mark (Figure 1) and intradermal infiltration on the marking with 200 ml of saline solution to 0.9%, adrenaline within concentration of 1:200,000. Skin incision and subcutaneous dissection were made and identification of the inferior superficial epigastric arteries, located between six to eight centimeters from the midline, and isolation of the artery and superficial circumflex iliac vein located at nine to eleven centimeters from the sagittal middle line, located below the Scarpa's fascia (Figures 2 and 3).
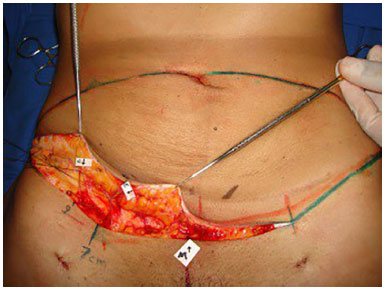
Figure 1. Surgical marking and artery isolation.
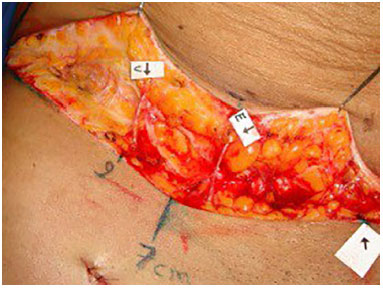
Figure 2. Superficial inferior epigastric artery isolation (E) and superficial circumflex iliac artery of the abdomen (C).
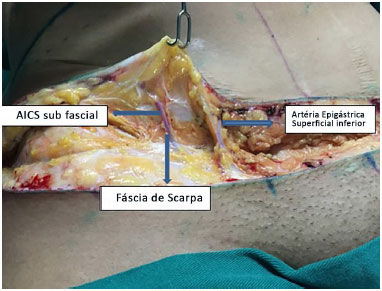
Figure 3. Subfascial topography of superficial epigastric artery. SCIA: Superficial Circumflex Iliac Artery
The artery was isolated and catheterized with Jelco® no. 22 or 24 according to the diameter that ranged between 1 and 3 millimeters. Distal stump of the vein and artery were sutured with cotton thread 30. The abdominoplasty flap was detached, sectioned and released from the upper part of the abdominal flap according to Pitanguy's technique. The superficial epigastric arteries of the upper flap were blocked to avoid extravasation of the contrast media in fluoroscopy. The flap received an heparinized solution with 100 u / ml (25,000 units:250 ml saline 0.9%) through SCIA and catheterized with Jelco® fixed using a 30 cotton thread (Figures 4 and 5).
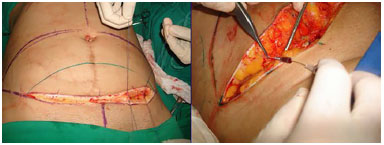
Figure 4. Dissection and isolating of superficial circumflex iliac artery and inferior epigastric artery.
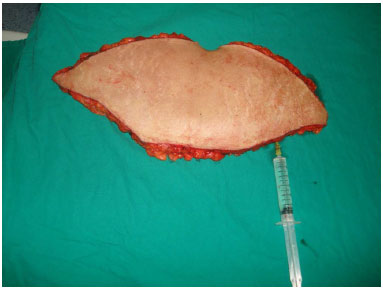
Figure 5. Graft prepared for contrast radiography in superficial circumflex iliac artery of of the abdomen.
The piece was taken to the hemodynamic laboratory to fluoroscopy. After that, the surgical team finished the surgery. The piece was placed in hemodynamic machine GE Ever View 7500 and the low osmolality iodinated contrast Optray® 350 (350mg/ml of organically bound iodine) was injected under fluoroscopy using a volume varying between 20 and 50 ml.
Hemodynamic measurements were performed only at isolated SCIA, the side with scars was excluded and the observation limit was the sagittal line of the anatomical part because the arteries are bilateral and both were preserved in the surgery.
We used a device to fill a plastic tube with contrast to limit areas corresponding to the flap of abdominoplasty and miniabdominoplasty regarding their perfusion (Figure 6).
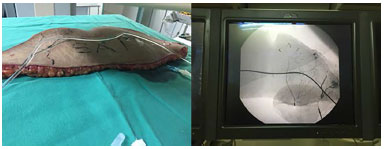
Figure 6. Device with plastic tube with contrast identifying areas 1 and 2.
Below the marked line by plastic tube with contrast is located the area (1) and above the area (2) that corresponds to the upper area of the flap preserved in miniabdominoplasty and discarded in the conventional type V abdominoplasty. The choice flap side artery to be dissected was random, but careful was taken to exclude the side with some type of surgical scar, such as appendicectomies. Images obtained were recorded as photographs and videos (Figures 7 and 8).
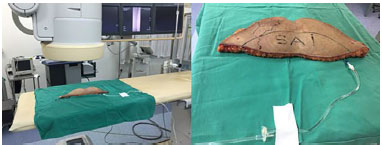
Figure 7. Images of sample submitted to fluoroscopy in hemodynamic laboratory.

Figure 8. Area 1 inferior SAI (dry) in mini-abdominoplasty.
Hemodynamic studies were evaluated by three observers. Of them, two were surgeons and one radiologist. The radiologist decided discussion in case of divergence in decision. The studies were classified as inadequate when the contrast injected into the SCIA did not fill the upper flap and area 2during fluoroscopy. They were considered adequate when filled the lower (1) and upper part (2) (Figure 9).

Figure 9. Radioscopy of areas 1 and 2.
The following variables were collected from patients: sex, race, age, weight, height, comorbidities and weight of the flap.
Parameters of quantitative variables were expressed as mean and standard deviation, and test of normality. The Pearson's test was used to verify possible linear correlation between BMI and weight of the removed flap. For statistical analyses, we used the GraphPad InStat software.
This study was approved by the Ethics and Research Committee of the Hospital Agamenon Magalhaes, CAAE number 42084815.5.0000.5197. All patients signed the informed consent.
RESULTS
During the period of the study 82 patients underwent abdominoplasty. Of these, 33 who met our study criteria were selected. We excluded 6 patients (18.9%), 4 because of arterial thrombosis in the anatomical specimen and 2 because of mechanical injury of the arterial wall caused by the catheter tip on the surgical specimen.
Patients age ranged between 23 and 49 years (36.6 ± 7.5). Their body mass index (BMI) ranged from the 22.0 to 30.5 (24.9 ± 2.1), and weight of the resected surgical specimens ranged from 450 to 1010 grams (623.1 ± 141.5). The Pearson's test between BMI and weight of the specimens was r = 0.91 and r2= 0.83. We included 32 women (97%) and 1 man (3%). One patient had stable hypertension (3%) and no patients had diabetes. Of the sample, 27 were pardo (81.8%), 2 white (6.1%), 3 black (9.1%) and 1 native south American (3.0%). There was no correlation between age and increased BMI (r = 0.35).
In hemodynamic studies, images and videos obtained showed injection of iodine contrast in SCIA initially filled the lower part of the flap (area 1) and progressively the upper part (area 2), surpassing even the midline and reaching the contralateral portion of the surgical specimen (Figures 10 and 11). They were considered adequate in 25 (92%) patients when it filled areas 1 and 2 and inadequate in 2 (8%) cases, were it did not fill area 2.
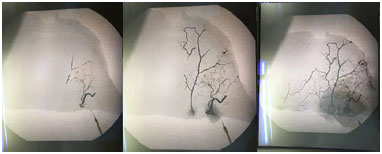
Figure 10. Contrast progressively filling areas 1 and 2.
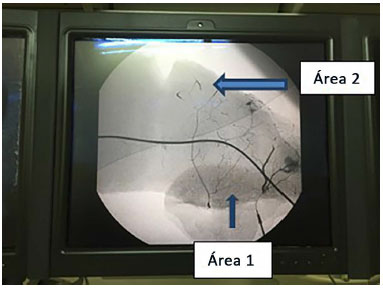
Figure 11. Areas 1 and 2 divided by contrast tube.
In figures 12 to 14 show adequate postoperative results of miniabdominoplasty and inadequate with necrosis and scarring sequelae.

Figure 12. Results of adequate postoperative.

Figure 13. Sequence of vascular failure with necrosis and inadequate result.
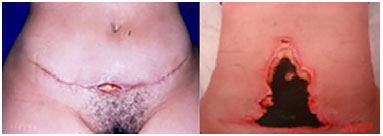
Figure 14. Sequence of small and large necrosis.
DISCUSSION
The study of the vascular pattern of the abdominal wall on abdominoplasty flap shows particular importance in patients undergoing mini-abdominoplasty and minilipoabdominoplasties, particularly because they have high expectations about the outcome of their surgery, and do not tolerate unaesthetic scars.
Hemodynamic images of the region supplied by SCIA, which corresponds to area 2 of the studied specimens, draw attention to the importance of its preservation when these surgeries are performed. To date, this vessel does not have the appropriate importance and it is often eletrocoagulated and sectioned.
This vessel supply was the focus of our study. There was a high percentage of supply in areas 1 and 2 on the surgical specimens, opening the prospect that preservation can contribute to the proper outcome of these surgeries and to avoid complications such as unsightly scarring by poor perfusion of the flap distal end (zone I by Matarasso), a fact that may cause ischemia and tissue necrosis.
Schaverien et al.19 reports that perfusion in the superficial inferior epigastric artery produces supply disabilities across the midline of the abdominal flap, a fact not observed in our study in which infusion of the contralateral areas II and IV corresponded to island of TRAM flap. Despite this finding, we must preserve the SCIA bilaterally to higher retail blood supply. This observation adds to the contemporary knowledge as a relevant contribution to the improvement of surgical techniques, as a consequence of better knowledge of the lower abdominal wall vascularity.
Saldanha et al.20, however, in the lipoabdominoplasty technique, described preservation of anatomical plane below the Scarpa's fascia which is the way of the side branches of SCIA, and before entering the subdermal abdominal flap, this may be a relevant factor in the low levels of necrosis and seromas described by authors.
By observing the percentage of exclusion of patients (18.9%) because of some limitation, we observed that some refinements in the SCIA catheterization process, with more flexible catheters and more adequate anticoagulation and a larger volume of heparin solution, along with better manipulation and mobilization of retail prior to full withdrawal of the specimen, can help reduce these sample losses in studies in the future.
Scarring of the lower abdomen is common in patients who underwent abdominoplasty, especially the Pfannenstiel21-23 which often has the problem that fact that SCIA may have been sectioned by enlarged subcutaneous dissection when compared to low extension of the incision on the skin and it can be avoided if general and gynecological surgeons have the prior knowledge that preservation of this vessel is of great importance in future plastic surgeries of the abdominal wall in which these patients could undergo in the future.
CONCLUSION
Hemodynamic findings of this study support the relevance of blood supply to abdominal wall by the preservation of superficial circumflex iliac artery in miniabdominoplasties and minilipoabdominoplasties. In addition, it indicated that bilateral preservation of these vessels can prevent necrosis of the abdominal flap.
COLLABORATIONS
CLAA Contributed to the analysis, interpretation of data, statistical analysis, approval of the final version to be published, conception and design of the study, surgeries and/or experiments, drafting the manuscript and critical review of content of the study.
LFDFV Contributed to the analysis, interpretation of data, approval of the final version to be published, conception and design of the study, surgeries and/or experiments, drafting the manuscript and critical review of content of the study.
LASL Contributed to the analysis, interpretation of data.
JAVO Contributed to the analysis, interpretation of data, surgeries and/or experiments.
RFA Contributed to surgeries and/or experiments, drafting the manuscript and critical review of content of the study.
EJBO Contributed to surgeries and/or experiments, drafting the manuscript and critical review of content of the study.
CTB Contributed to the analysis, interpretation of data, statistical analysis, approval of the final version to be published, conception and design of the study, drafting the manuscript and critical review of content of the study.
REFERENCES
1. American Society of Plastic Surgeons. 2008 report of the 2007 statistics: National Clearinghouse of Plastic Surgery Statistics [Acesso 20 Abr 2016]. Disponível em: http://www.plasticsurgery.org/Documents/news-resources/statistics/2007-Plastic-Surgery-Statistics/full-statstics-report.pdf
2. Rohrich RJ, Stuzin JM. Globalization of plastic surgery: the world of plastic and reconstructive surgery in Brazil. Plast Reconstr Surg. 2012;130(4):967-8. PMID: 23018706 DOI: http://dx.doi.org/10.1097/PRS.0b013e31826703b1
3. Nahas FX. A pragmatic way to treat abdominal deformities based on skin and subcutaneous excess. Aesthetic Plast Surg. 2001;25(5):365-71. DOI: http://dx.doi.org/10.1007/s00266-001-0025-7
4. Nahai FR. Anatomic considerations in abdominoplasty. Clin Plast Surg. 2010;37(3):407-14. DOI: http://dx.doi.org/10.1016/j.cps.2010.03.003
5. Bozola AR, Psillakis JM. Abdominoplasty: a new concept and classification for treatment. Plast Reconstr Surg. 1988;82(6):983-93. PMID: 2974166 DOI: http://dx.doi.org/10.1097/00006534-198812000-00008
6. Rieger UM, Petschke F, Djedovic G, Engelhardt TO, Biebl M, Pierer G. Abdominal wall reconstruction after extensive abdominal wall necrosis resulting from chevron incision for liver transplant and subsequent Y-shaped incision for re-transplantation-clinical experience and literature review. J Plast Reconstr Aesthet Surg. 2012;65(3):e71-3. PMID: 22115912 DOI: http://dx.doi.org/10.1016/j.bjps.2011.11.021
7. Smith LF, Smith LF Jr Safely combining abdominoplasty with aggressive abdominal liposuction based on perforator vessels: technique and a review of 300 consecutive cases. Plast Reconstr Surg. 2015;135(5):1357-66. DOI: http://dx.doi.org/10.1097/PRS.0000000000001200
8. Matarasso A. Traditional abdominoplasty. Clin Plast Surg. 2010;37(3):415-37. DOI: http://dx.doi.org/10.1016/j.cps.2010.03.006
9. Huger WE Jr. The anatomic rationale for abdominal lipectomy. Am Surg. 1979;45(9):612-7. PMID: 159651
10. Matarasso A. Abdominolipoplasty: a system of classification and treatment for combined abdominoplasty and suction-assisted lipectomy. Aesthetic Plast Surg. 1991;15(2):111-21. PMID: 2035359 DOI: http://dx.doi.org/10.1007/BF02273843
11. Bozola AR. Abdominoplasty: same classification and a new treatment concept 20 years later. Aesthetic Plast Surg. 2010;34(2):181-92. DOI: http://dx.doi.org/10.1007/s00266-009-9407-z
12. Mejia JA, Cárdenas Castellanos YA. Extended abdominoplasty: applications and a new classification system for abdominoplasty. Aesthetic Plast Surg. 2012;36(2):278-84. DOI: http://dx.doi.org/10.1007/s00266-011-9818-5
13. Pitanguy I, Salgado F, Murakami R, Radwanski HN, Mauad Junior R. Abdominoplastia: classificação e técnicas cirúrgicas. Rev Bras Cir. 1995;85(1):23-44.
14. Nahas FX. An aesthetic classification of the abdomen based on the myoaponeurotic layer. Plast Reconstr Surg. 2001;108(6):1787-95. DOI: http://dx.doi.org/10.1097/00006534-200111000-00057
15. Bozola AR, Psillakis JM. Abdominoplasty: a new concept and classification for treatment. Plast Reconstr Surg. 1988;82(6):983-93. PMID: 2974166 DOI: http://dx.doi.org/10.1097/00006534-198812000-00008
16. Graf R, de Araujo LR, Rippel R, Neto LG, Pace DT, Cruz GA. Lipoabdominoplasty: liposuction with reduced undermining and traditional abdominal skin flap resection. Aesthetic Plast Surg. 2006;30(1):1-8. DOI: http://dx.doi.org/10.1007/s00266-004-0084-7
17. Vicari Nogueira CHF. Evaluación Comparativa Pre y Postoperatoria de la Circulación cutânea de la pared abdominal por termogtafia infrarroja em Cirurgia Plástica - El efecto del Despegamiento em el Colgajo Abdominal. Barcelona: Universidad Autónoma de Barcelona, Departamento de cirurgia; 2012. 139p.
18. Uebel CO. Lipoabdominoplasty: revisiting the superior pulldown abdominal flap and new approaches. Aesthetic Plast Surg. 2009;33(3):366-76. PMID: 19296152 DOI: http://dx.doi.org/10.1007/s00266-009-9318-z
19. Schaverien M, Saint-Cyr M, Arbique G, Brown SA. Arterial and venous anatomies of the deep inferior epigastric perforator and superficial inferior epigastric artery flaps. Plast Reconstr Surg. 2008;121(6):1909-19. PMID: 18520876 DOI: http://dx.doi.org/10.1097/PRS.0b013e31817151f8
20. Saldanha OR, De Souza Pinto EB, Mattos WN Jr, Pazetti CE, Lopes Bello EM, Rojas Y, et al. Lipoabdominoplasty with selective and safe undermining. Aesthetic Plast Surg. 2003;27(4):322-7. PMID: 15058559 DOI: http://dx.doi.org/10.1007/s00266-003-3016-z
21. Park YJ, Kim EK, Yun JY, Eom JS, Lee TJ. The influence of pfannenstiel incision scarring on deep inferior epigastric perforator. Arch Plast Surg. 2014;41(5):542-7. PMID: 25276647 DOI: http://dx.doi.org/10.5999/aps.2014.41.5.542
22. Shermak MA, Mallalieu J, Chang D. Do preexisting abdominal scars threaten wound healing in abdominoplasty? Eplasty. 2010;10:e14. DOI: http://dx.doi.org/10.1097/PRS.0b013e3181ef8fa3
23. El-Khatib HA, Bener A. Abdominal dermolipectomy in an abdomen with pre-existing scars: a different concept. Plast Reconstr Surg. 2004;114(4):992-7. DOI: http://dx.doi.org/10.1097/01.PRS.0000133201.07767.5E
1. Sociedade Brasileira de Cirurgia Plástica, Recife, PE, Brazil
2. Hospital Agamenon Magalhães, Recife, PE, Brazil
3. Universidade Federal de Pernambuco, Recife, PE, Brazil
4. Hospital das Clínicas-UFPE, Recife, PE, Brazil
Institution: Hospital Agamenon Magalhães, Recife, PE, Brazil.
Corresponding author:
Carlos Lacerda Andrade Almeida
Praça Professor Fleming, 77 - Jaqueira
Recife, PE, Brazil Zip Code 52050-180
E-mail: clacerda@elogica.com.br
Article received: October 28, 2015.
Article accepted: April 10, 2016.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter