

Original Article - Year 2016 - Volume 31 -
Exclusive use of absorbable suture threads in cleft lip and palate
Uso exclusivo de fios absorvíveis em fendas labiopalatais
ABSTRACT
INTRODUCTION: The treatment of orofacial clefts comprises steps that may result in considerable psychological trauma for patients and their caregivers. The use of absorbable sutures may help to eliminate these uncomfortable situations. However, the exclusive use of this synthetic material is still not preferred by surgeons, particularly in the muscle planes.
METHODS: Data from patients who underwent surgery at the University Hospital of the Federal University of Rio de Janeiro from 2007 to 2014 were used. The patients underwent correction of cleft lip or palate, using only absorbable sutures (poliglecaprone 25 - Monocryl® or polyglactin 910 - Vicryl Rapide®) in all suture planes (mucosa, muscle, skin).
RESULTS: We found 360 patients who met the inclusion criteria for this study. We did not observe differences in terms of the local appearance of the wounds during the suture absorption process. The incidence of dehiscence or fistula cases was below 1%, and there were no complications regarding the objectives of the study. In the long term, the scars did not differ from those obtained with non-absorbable sutures used in other types of surgeries.
CONCLUSIONS: The exclusive use of absorbable sutures was shown to be an efficient and safe option. These resulted in good quality scars and adequate tensile strength (even in muscle planes), and we did not observe complications related to the absorption process of the material used.
Keywords: Healing; Suture threads; Cleft lip surgery; Cleft palate surgery; Psychological stress.
RESUMO
INTRODUÇÃO: O tratamento de fendas labiopalatais tem etapas que podem trazer traumas psicológicos consideráveis aos pacientes e familiares. O uso de fios absorvíveis pode eliminar um destes momentos desconfortáveis. Contudo, a utilização exclusiva deste tipo de material de síntese ainda não é a preferência de todos os cirurgiões, principalmente em planos musculares.
MÉTODOS: Levantados os dados dos pacientes operados no Hospital Universitário da Universidade Federal do Rio de Janeiro, submetidos à correção de fendas labiais ou palatais, nas quais foram utilizados somente fios absorvíveis (poliglecaprona 25 - Monocryl® ou poliglactina 910 - Vicryl Rapide®) em todos os panos de sutura (mucosa, músculo, pele). O período avaliado foi de 2007 a 2014.
RESULTADOS: Encontramos 360 pacientes que se enquadraram no estudo. Não observamos diferenças quanto ao aspecto local das feridas durante o processo de absorção dos fios. A incidência de deiscências ou fístulas se manteve abaixo de 1% e não houve complicações relacionadas ao objetivo do estudo. As cicatrizes não se mostraram, a longo prazo, diferentes das obtidas com o uso de fios inabsorvíveis, utilizados em outros tipos de cirurgias.
CONCLUSÕES: O uso exclusivo destes fios absorvíveis se mostrou uma opção eficaz e segura. Proporcionou cicatrizes de boa qualidade, força tênsil adequada (mesmo em planos musculares) e não observamos complicações relacionadas ao processo de absorção dos materiais empregados.
Palavras-chave: Cicatrização; Suturas; Fenda labial/cirurgia; Fenda palatina/cirurgia; Estresse psicológico.
Surgical trauma resulting from cleft lip or palate correction usually heals well in patients, including young children.
In contrast, the psychological trauma resulting from the procedure may lead to considerable damage to children and their caregivers. This is important to take into account, considering the long course of treatment and follow-up.
Whenever possible, we have eliminated steps or procedures that might cause this type of discomfort. Removing sutures is one of the steps we eliminated. The routine for removing sutures in some health centers in Brazil where pediatric patients undergo surgery is usually the following:
a. Holding the child, which at this point is very scared and cries, and tries to get free;
b. Sedation or general anesthesia, which requires using drugs, with the possibility of adverse events;
c. Using absorbable sutures - the method used by our team - which prevents the possible disadvantages of the previous steps.
In addition to skin and mucosa, we extended the use of absorbable sutures to the muscle plane.
Obviously, the quality of the synthetic material used directly affects the results. Absorbable sutures must have tensile strength and absorption times with characteristics that allow adequate healing in all planes, providing firm and efficient adhesion between tissues.
We present an analysis of 360 patients who underwent cleft lip or palate correction using only absorbable sutures (poliglecaprone 25 - Monocryl® or polyglactin 910 - Vicryl Rapide®) in all suture planes (the mucosa, muscle, skin).
OBJECTIVE
To demonstrate a positive outcome with the exclusive use of absorbable sutures in all suture planes for the treatment of cleft lip and palate.
METHODS
Data were collected from records of all patients who underwent surgery for cleft lip or palate correction from 2007 to 2014 at the Clementino Fraga Filho University Hospital, Federal University of Rio de Janeiro (HUCFF-UFRJ).
The ethical principles of the Helsinki Declaration revised in 2000 were followed, as well as those of Resolution 196/96 of the Brazilian National Health Council.
As inclusion criteria, we considered all patients in whom absorbable sutures were used in all suture planes, in primary or secondary surgeries.
Patients who underwent surgery in which non-absorbable sutures were used were excluded from the study.
Data were analyzed to characterize the treatments performed, particularly regarding the following factors:
1. Synthetic material used in each suture plane;
2. Local appearance during material absorption;
3. Time to absorption (disappearance) of the sutures;
4. Muscular function in the areas submitted to surgery;
5. Quality of scars;
6. Complications.
RESULTS
A total of 360 patients met the inclusion criteria. Ages ranged from 3 months to 62 years, and 52% were male.
Of all surgeries performed, 38% were cheiloplasty and 62% were palatoplasty procedures.
The minimum postoperative follow-up duration was 4 months.
The sutures used were the following:
For the cleft lip:
1. Monocryl® 5-0 in mucosa (13-mm cutting needle);
2. Monocryl® 4-0 in musculature (16-mm cutting needle);
3. Monocryl® 4-0 in the points for nasal suspension (McComb type) (6-cm straight-cutting Keith needle, to place the thread);
4. Vicryl Rapide® 6-0 in skin (11-mm cutting needle);
For the cleft palate:
1. Monocryl® 5-0 in nasal mucosa (13-mm cutting needle);
2. Monocryl® 4-0 in musculature (16-mm cutting needle);
3. Monocryl® 4-0 in oral mucosa (16-mm cutting needle).
Differences were not observed in terms of the local appearance of wounds during the suture absorption process.
The average time for the initiation of suture absorption (disappearance) when used in skin synthesis of cleft lip (Vicryl Rapide® 6-0) was 7 days. After 16 days, this type of suture was no longer visible at the site (Figure 1).
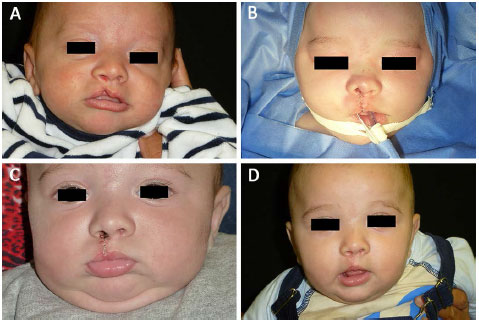
Figure 1. A: Preoperative appearance of incomplete unilateral cleft lip; B: Immediate postoperative appearance. Cutaneous synthesis with 6-0 Vicryl Rapide®. Points for nasal suspension with 4-0 Monocryl®, with the knots inside the right nostril. Discrete cutaneous retraction in the nasal dorsum; C: 9 days after surgery. Absence of nasal cutaneous retraction after accommodation of the tissues; D: 30 days after surgery. Total disappearance of Vicryl Rapide® and Monocryl®.
In the synthesis of oral mucosa for cleft palate correction, the average time for the initiation of suture absorption (disappearance) was 9 days. After 30 days, residual sutures were not usually visible.
The incidence of dehiscence or fistula was below 1%, and complications related to the objectives of this study were not observed.
In the long term, scars did not differ from those obtained with non-absorbable sutures used in other types of surgeries (Figures 2 and 3).
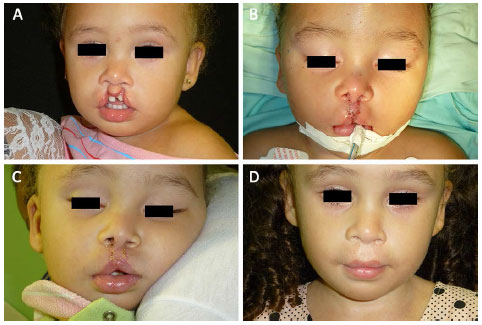
Figure 2. A: Preoperative appearance of incomplete bilateral lip with alveolar cleft; B: Immediate postoperative appearance; C: 9 days after surgery; D: Two years after surgery.

Figure 3. A: Preoperative appearance of complete left unilateral cleft lip and palate; B: Immediate postoperative appearance; C: 5 days after surgery. Using nasal reshaping. A film of Dermabond® was applied over the skin suture and the fixation strips of the reshaper; D: 6 years after surgery.
As the tensile strength and absorption time of materials were adequate for healing and resulted in a low incidence of dehiscence in the skin and mucosa, the same adequate conditions were equally maintained in the muscle synthesis. In addition, Monocryl® is one of the most resistant absorbable sutures available1. Further tests to assess muscular adhesion were not performed, but physical examination demonstrated the recovery of lip and palate function.
DISCUSSION
The treatment protocols for cleft lip and cleft palate correction usually require long-term follow-up. Adherence to these protocols is usually associated with several factors, including psychological trauma in children and their caregivers.
The efficacy of surgical treatment partly depends on the quality of synthetic materials used and the follow-up performed in surgical centers.
In 1995, Tandon et al.2 described an experiment with a "new suture" (Vicryl Rapide®) in 236 patients with skin and mucosal wounds. The authors compared the results with those for non-absorbable monofilament sutures and did not find aesthetic differences after 3 months of follow-up. They emphasized the ease of handling the material after surgery, because it did not require the removal of sutures, and the hydrolysis process that occurs through the absorption of material decreased the incidence of wound abscesses.
In 1999, Aderriotis & Sàndor3 compared Vicryl Rapide® with normal Vicryl® in 80 oral wounds and 42 scalp wounds. The authors reported favorable evolution with the use of Vicryl Rapide® as well as decreased postoperative costs, since there was no need to perform complementary procedures to remove the sutures. In addition, they observed a lower inflammatory reaction in the Vicryl Rapide® cases. In their study, this suture was completely absorbed in 12 to 14 days.
Al-Qattan4 performed a similar comparison and reported some problems with normal Vicryl®, with slow absorption. The author did not observe dehiscence in wounds sutured with Vicryl Rapide® and observed an adequate time of absorption in the pediatric population.
Some surgeons only use non-absorbable sutures in the correction of cleft lip and palate, in both the superficial plane (mucosa and skin), and deep plane (muscle). This is because of habit or concern about the strength, tension, and absorption time of absorbable sutures. This concern particularly involves sutures in the muscular plane, in which wound dehiscence may lead to inefficient surgical treatment.
However, the quality of suture materials has improved, and further research will result in sutures that will only lose their tensile strength and be absorbed after adequate healing of the wound5,6. This will provide more reliability for protocols based on exclusive use of absorbable sutures, as in the protocol we followed.
Viterbo et al.7 performed a study on mice to compare the tensile strength of different types of sutures. They reported that all the materials analyzed, including Vicryl Rapide®, had tensile strength at 30 days that was higher than that predicted by the manufacturers.
In some cases of cleft lip, we applied cyanoacrylate glue (Dermabond®) over skin sutures performed with Vicryl Rapide® 6-0 to create a protective film against contamination due to food or nasal secretions8. This was not practical, since serosanguinous fluid frequently accumulated over the film. This created an unclean wound that could only be cleaned after the spontaneous disappearance of the glue after 7 to 10 days. Even though it did not interfere with the final result, we discontinued using Dermabond® and recommended that patients wash the wound normally during a shower 24 hours after surgery.
In the points for nasal suspension (McComb type), Monocryl® 4-0 was used. With the aid of a long, straight Keith needle (previously used to put the thread in position), we entered the nasal cavity, moved outwards through the nasal dorsum, and moved inwards again through the same hole in the skin (but following a different path at the subcutaneous level). Therefore, knots remained inside the nostril; there was no need to remove the threads, and the suture strength was maintained for a longer period than usual, enabling more lasting results9. We did not observe significant inflammatory reactions that required the removal of sutures before complete absorption (Figure 4).
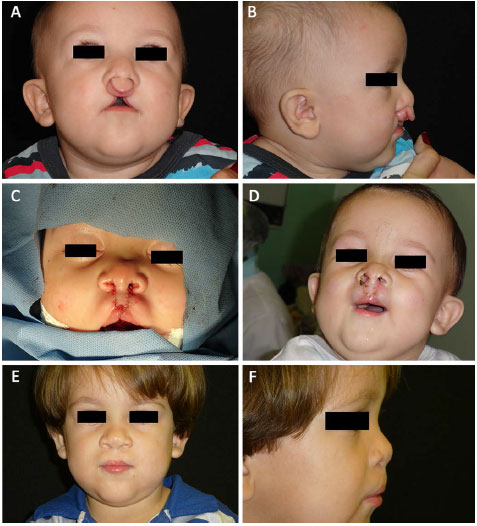
Figure 4. A: Preoperative appearance of complete bilateral cleft lip and palate; B: Postoperative appearance, profile view; C: Immediate postoperative appearance; D: 9 days after surgery. A film of Dermabond® was applied over the skin suture; E: 2 years after surgery, frontal view; F: 2 years after surgery, profile view.
In cleft palate cases, 4-0 and 5-0 Monocryl ® with 16- and 13-mm cutting needles, respectively, were used to place sutures inside the oral cavity. Another interesting option in palatoplasty, in which mucoperiosteal flaps were deployed, was the use of absorbable hemostatic materials (oxidized regenerated cellulose - Surgicel®) in the lateral raw areas, after the liberating incisions (Figure 5). These are absorbed or eliminated in the first week after surgery, and do not cause a strong, foul smell that occurs with Vaseline gauze (which requires them to be removed).

Figure 5. Immediate postoperative appearance of palatoplasty. Only absorbable sutures were used. Note the Surgicel® applied in the lateral areas (liberating incisions).
Thus, we believe that we can provide comfort for children during the postoperative follow-up, without reducing efficacy of the surgical procedure, by minimizing the possible psychological trauma of complex treatment associated with cleft lip and palate surgery.
CONCLUSION
The exclusive use of absorbable sutures was shown to be an efficient and safe option. These resulted in good quality scars, adequate tensile strength (even in the muscle planes), with no complications related to the absorption process.
COLLABORATIONS
DF Analysis and/or interpretation of data; approval of final manuscript; performing the surgeries and/or experiments; writing the manuscript or critical review of its content.
PC Analysis and/or interpretation of data; planning and design of the study.
JMTF Approval of final manuscript; planning and design of the study; writing the manuscript or critical review of its content.
TF Analysis and/or interpretation of data; approval of final manuscript; planning and design of the study; writing the manuscript or critical review of its content.
REFERENCES
1. LaBagnara J Jr. A review of absorbable suture materials in head & neck surgery and introduction of monocryl: a new absorbable suture. Ear Nose Throat J. 1995;74(6):409-15. PMID: 7628331
2. Tandon SC, Kelly J, Turtle M, Irwin ST. Irradiated polyglactin 910: a new synthetic absorbable suture. J R Coll Surg Edinb. 1995;40(3):185-7. PMID: 7616473
3. Aderriotis D, Sàndor GK. Outcomes of irradiated polyglactin 910 Vicryl Rapide fast-absorbing suture in oral and scalp wounds. J Can Dent Assoc. 1999;65(6):345-7. PMID: 10412244
4. Al-Qattan MM. Vicryl Rapide versus Vicryl suture in skin closure of the hand in children: a randomized prospective study. J Hand Surg Br. 2005;30(1):90-1. DOI: http://dx.doi.org/10.1016/j.jhsb.2004.08.005
5. Menaker GM. Wound closure materials in the new millennium. Curr Probl Dermatol. 2001;13(2):90-4. DOI: http://dx.doi.org/10.1016/S1040-0486(01)70039-7
6. Hochberg J, Meyer KM, Marion MD. Suture choice and other methods of skin closure. Surg Clin North Am. 2009;89(3):627-41. PMID: 19465201 DOI: http://dx.doi.org/10.1016/j.suc.2009.03.001
7. Viterbo F, Viterbo F, Camargo GGR, Brock RS. Força tênsil de diferentes tipos de fio de sutura. Estudo em ratos. Bol Cir Plást. mar/abr 2014 [Acesso 16 Set 2015]. Disponível em: http://boletim.med.br/boletim/artigos_ver.php?id=286
8. Knott PD, Zins JE, Banbury J, Djohan R, Yetman RJ, Papay F. A comparison of dermabond tissue adhesive and sutures in the primary repair of the congenital cleft lip. Ann Plast Surg. 2007;58(2):121-5. DOI: http://dx.doi.org/10.1097/01.sap.0000232984.68797.62
9. Franco D, Eyler AD. Cirurgia de fissurados: detalhes que facilitam. Rev Bras Cir Plast. 2003;18(1):55-69.
1. Universidade Federal do Rio de Janeiro, Rio de Janeiro, RJ, Brazil
2. Hospital Universitário Clementino Fraga Filho, Rio de Janeiro, RJ, Brazil
Institution: Hospital Universitário Clementino Fraga Filho - Universidade Federal do Rio de Janeiro, Rio de Janeiro, RJ, Brazil.
Corresponding author:
Diogo Franco
Rua Ramon Franco, 98 - Urca
Rio de Janeiro, RJ, Brazil Zip Code 22290-290
E-mail: contato@diogofranco.com
Article received: September 24, 2015.
Article accepted: May 12, 2016.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter