

Original Article - Year 2016 - Volume 31 -
Second intention healing in the treatment of nasal basal cell carcinoma
Cicatrização por segunda intenção no tratamento de carcinoma basocelular nasal
ABSTRACT
INTRODUCTION: The search for better alternatives for the treatment of nasal basal cell carcinoma (BCC) has been reported by several authors. The complications associated with grafts and skin flaps include the risk of non-integration or necrosis, and the formation of scars that are often large or unaesthetic. In addition, these procedures require longer operative times, which implies the need for a surgical center. The simple removal of nasal BCC, followed by second intention healing and simple postoperative cosmetic care, has reemerged as a valid alternative for the treatment of these tumors.
METHODS: In this study, the authors describe their experience with the technique, and report the advantages of the method. All patients submitted to this procedure were followed-up prospectively for a period of 4 years.
RESULTS: Of 23 patients, 12 were monitored for 2 years and were included in the study. The surgical procedure was performed without difficulty in an average of 21 minutes (+6). Postoperative evolution was uncomplicated and without tumor recurrence.
CONCLUSION: This technique is a simple and safe alternative, providing excellent results for the treatment of nasal BCC.
Keywords: Basal cell carcinoma; Intention; Healing; Nose; Skin neoplasms.
RESUMO
INTRODUÇÃO: A busca por melhores alternativas para o tratamento do carcinoma basocelular (CBC) nasal é referida por diversos autores há anos. Os enxertos e os retalhos cutâneos apresentam problemas, como o risco de não integração ou de necroses; e ainda determinam a formação de cicatrizes que, muitas vezes, são extensas ou inestéticas. Além disso, eles demandam um tempo operatório maior, sendo realizados em centro cirúrgico. A exérese simples do CBC nasal, seguida da cicatrização por segunda intenção e de cuidados cosmiátricos simples no pós-operatório, ressurge como alternativa válida para o tratamento destes tumores.
MÉTODOS: Os autores vêm apresentar sua experiência com a técnica, discutindo as vantagens do método. No período de 4 anos, todos os pacientes submetidos à técnica foram acompanhados prospectivamente.
RESULTADOS: Dos 23 pacientes operados, 12 foram acompanhados por 2 anos e incluídos na avaliação. O procedimento cirúrgico teve duração média de 21 minutos (+6) e foi realizado sem dificuldades. A evolução pós-operatória se deu sem intercorrências ou recidivas tumorais.
CONCLUSÃO: A técnica empregada coloca-se como uma alternativa simples, segura e com excelentes resultados para o tratamento dos CBC nasais.
Palavras-chave: Carcinoma basocelular; Intenção; Cicatrização; Nariz; Neoplasias cutâneas.
The skin cancer with the highest incidence in Caucasians is basal cell carcinoma (BCC), accounting for approximately 70% of cases1. Chronic exposure to ultraviolet (UV) rays and genetic aspects are among the risk factors most cited in the literature2. Although it is rarely metastatic, BCC is worrying, as it is characterized by local aggressiveness that often requires mutilating and challenging treatments3. When the nose is affected, especially the tip and nasal wings, the functional and aesthetic consequences of existing treatments can be even worse4.
The choice of treatment for nasal BCC is based on different aspects, with multiple alternatives and concerns4. Among the numerous possibilities, simple removal, followed by the creation and advancement of a local skin flap, remains the option that is most performed by plastic surgeons4. Depending on the case, skin grafts are also commonly used. Less invasive alternatives such as lasers, cryosurgery, electrosurgery, curettage followed by electrosurgery, phototherapy, and chemical abrasion are also successfully employed in daily practice5.
For more than 10 years, the authors have advocated an alternative method for the treatment of nasal BCC measuring up to 1.5 cm in diameter: the simple removal of the tumor, combined with electrocoagulation and second intention healing. This technique was widely used in the past and has reemerged as an interesting therapeutic option.
This method offers important advantages when compared to other surgical options that are currently available: it is easy, safe, and quickly performed, with low operating costs and complication rates. The technique also minimizes the extent of scarring caused by the rotation of flaps and skin grafts, which further highlights the rationale for more frequent use6.
The addition of simple postoperative cosmetic treatment allows more efficient healing results, in terms of functionality and aestheticst7. The treatment of the residual circular scar restores a nasal appearance similar to that present before the occurrence of the tumor and minimizes possible sequelae resulting from the treatment, thus increasing patient satisfaction7.
OBJECTIVE
The aim of this study is to present the results of nasal BCC treatment, based on removal by simple excision, combined with electrocoagulation, second intention healing, and postoperative cosmetic treatment, and to discuss the technical alternatives and advantages of the procedure.
METHODS
All patients who underwent the treatment were prospectively evaluated in the author's private clinic, from January 2008 to January 2012.
All patients with a suspected BCC measuring up to 1.5 cm in diameter on the nasal tip or wing underwent incisional biopsy. If histopathological examination confirmed the presence of a nodular or superficial BCC, the technique described was offered to the patient. Those who chose to undergo the procedure were included in the study. Others were excluded, and underwent routine treatment with a local skin flap.
The surgical technique of simple tumor removal, combined with electrocoagulation, second intention healing, and postoperative cosmetic treatment was performed in a medical office (Figures 1 to 3). With the patient in a supine position, antisepsis was performed, followed by sterile draping.

Figure 1. Perioperative aspects. A: positioning with antisepsis. B: local anesthesia. C: marking of the area to be resected. D: resection of the tumor with a cold blade. E: electrocoagulation of the treated surface. F: dressings as described.

Figure 2. Perioperative aspects. A: positioning with antisepsis. B: marking of the area to be resected. C: local anesthesia l. D: resection of the tumor with a cold blade. E: electrocoagulation of the treated surface. F: treatment of the lesion with collagenase ointment as described.

Figure 3. Perioperative aspects. A: positioning with antisepsis. B: local anesthesia. C: resection of the tumor with a cold blade. D: electrocoagulation of the treated surface. E: surface treated after electrocoagulation. F: dressings as described.
Local anesthesia was performed with infiltration of 3-6 ml of a solution containing 2% lidocaine with 1:200,000 epinephrine. The tumor was resected with a number 15 blade; the affected tissue, including the deep dermis, was removed, with appropriate margins. When the entire tumor was removed, vigorous electrocoagulation and electrocautery of the entire open area were performed.
At the end of the procedure, the wound was covered with collagenase ointment and the patient was immediately discharged. The resected material was sent for histopathological examination to confirm the absence of positive margins.
After the procedure, all patients were instructed to apply collagenase ointment to the treated area, four times a day for the first 30 days. On the 30th day, application of a humectant lotion was added to aid in reepithelialization. This was composed of essential fatty acids, medium-chain triglycerides, vitamin A, and vitamin E; the frequent use of SPF 100 sunscreen lotion was prescribed.
On the 60th postoperative day, application of a silicone-based gel was added, to be used six times a day, combined with lesion coverage with a silicone gel plate at night. This protocol was maintained until the sixth postoperative month. After this, patients were instructed to use only sunscreen for another six months (Figure 4 and 5).

Figure 4. Postoperative. A: 15 days. B: 30 days. C: 60 days. D: 180 days. E and F: 360 days, frontal-lateral.

Figure 5. A: preoperative aspect (after biopsy). B: preoperative aspect (with marking of the margins to be resected). C: 60 days after surgery. D: 180 days after surgery.
After surgery, patients were monitored weekly for the first month and bimonthly until the eighth month. All patients were contacted by phone 24 months after surgery to schedule reevaluation. Patients who could not be reached or did not return for consultation were excluded from the study.
RESULTS
In the study period, 23 patients underwent the technique described. Eleven were excluded, as they did not return for postoperative consultation. The characteristics of the 12 patients included in the analysis are shown in Table 1.

The surgical procedure was performed in an average of 21 minutes. There was no difficulty in performing the technique, with no major bleeding or other complications. All patients were discharged immediately after the procedure and the postoperative evolution was without significant complications or tumor recurrence. Some of the patients are presented in Figures 6 to 10.

Figure 6. A: Preoperative image of patient I. B: postoperative image of patient I.
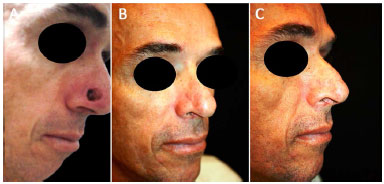
Figure 7. A: Immediate postoperative image of patient G. B: postoperative image of patient G in frontal-lateral position. C: postoperative image of patient G in lateral position.

Figure 8. A: Postoperative image of patient H in lateral position. B: postoperative image of patient H in frontal-lateral position.

Figure 9. A: Postoperative image of patient B in frontal-lateral position. B: postoperative image of patient B in frontal position.

Figure 10. A: Post-operative image of patient J in frontal-lateral position. B: post-operative image of patient J in frontal position.
DISCUSSION
Skin flaps are usually chosen to cover defects resulting from the treatment of nasal skin tumors, especially BCC7. Although these procedures are the most commonly used, the advancement of a skin flap is not a simple technique. It generally requires a secondary level hospital structure, and presents risks, difficulties, and complications inherent to a more elaborate surgical procedure8. Furthermore, the most satisfactory positioning and final quality of the scar are not always achieved9. Infection, necrosis, dehiscence, keloids, and hypertrophic scars are common, and contribute to a postoperative result that is often unsatisfactory8.
The recurring failure to achieve functional or aesthetically satisfactory results with nasal skin flaps and the need to simplify the treatment of these tumors motivated the search for fast, inexpensive, and feasible alternatives10.
Although still underestimated by some surgeons, the technique of simple circular removal of nasal tumors, combined with electrocoagulation, second intention healing, and postoperative cosmetic treatment, offers excellent results and significant advantages, when compared to other available options. The results presented showed that a dedicated and simple technique could provide satisfactory or superior results, when combined with low-cost, easy, and basic cosmetic therapy performed postoperatively by a plastic surgeon.
Circular resection of a nasal BCC is easily accomplished with a cold knife. The tumor is removed en bloc, with variable margins in the normal surrounding tissue. For the technique presented, successful outcomes depend on the careful selection of nasal tumors. Ideally, these should be nodular or superficial BCC subtypes, up to 1.5 cm in diameter, that are less likely to be aggressive and recurrent11-13.
Immediate electrocoagulation of the bleeding area allows treated surfaces to return to normal; control of bleeding and destruction of any residual tumor cells ultimately ensure low rates of recurrence14-16.
The surgical time was less than that normally required for the creation of skin flaps10. The ease of performing the procedure in a doctor's office avoids the use of the hospital, and is a technical advantage10.
The complications that commonly occur when flaps and skin grafts are used to cover defects caused by removal of BCC were not observed, thus strengthening the value of the technique10. Trapdoor deformities, dehiscence, and necrosis were not recorded in the study, and high-quality healing was the rule, even in smokers and diabetic patients17,18.
The basic mechanism underlying secondary intention healing is very similar to the process of first intention healing, as it is mainly characterized by an inflammatory response, angiogenesis, and formation of granulation tissue19. Second intention healing is slower, however, due to the action of myofibroblasts deposited in the wound; the contraction of the scar towards the center occurs slowly, reducing the dimension and approximating the edges of the lesion in 20 to 30 days. From an aesthetic and functional point of view, Zitelli10 stated that the most favorable sites for the application of this technique are the rounded prominences of the nose, as applied in this study.
Topical therapy with collagenase in the initial postoperative period ensured a clean, treated area, by enzymatically dissolving necrosis and crusts20. Moreover, it promoted the formation of good quality granulation tissue and provided rapid and normal wound reepithelialization, thus ensuring good final quality of the scar.
Therapy with a reepithelialization lotion facilitated the cell replication process and epidermal differentiation, minimizing late inflammatory and leukocytic reactions, while promoting granulation as well as rapid and complete reepithelialization of the wound21.
The addition of sunscreen prevented unwanted hyperpigmentation, which is often described in similar techniques. Sun exposure can trigger hyperpigmentation of the injury due to an intense proinflammatory effect that significantly damages the final result22.
The use of liquid silicone ointment improved local symptoms, and reduced the itching and sensitivity reported in the postoperative period23. After a few months, liquid silicone ointment also helped reduce local erythema and improved recovery of skin flexibility23.
Covering the lesion at night with a silicone gel plate increased the local tissue temperature and enhanced the action of endogenous collagenase, thus allowing the final normalization of the scar, preventing hardening and reducing the degree of retraction24.
The results in treated patients remained stable during a follow-up of more than 2 years. Tumor recurrences were not observed, thus demonstrating the safety and effectiveness of the technique.
CONCLUSION
The simple removal of areas affected by the tumor, combined with postoperative follow-up care as described, resulted in a favorable aesthetic outcome, with no complications or pathological and unaesthetic scars. The combined treatment described herein appears to be an alternative for the treatment of nasal lesions, in view of its technical simplicity and satisfactory long-term results.
COLLABORATIONS
DN Analysis and/or interpretation of the data; conception and study design; performance of the procedures and/or experiments.
MR Final approval of the manuscript; conception and study design.
FPT Analysis and/or data interpretation; conception and study design; performance of the procedures and/or experiments.
KBJ Statistical analysis and final approval of the manuscript.
DBL Statistical analysis and final approval of the manuscript.
REFERENCES
1. Telfer NR, Colver GB, Bowers PW. Guidelines for the management of basal cell carcinoma. British Association of Dermatologists. Br J Dermatol. 1999;141(3):415-23. PMID: 10583044 DOI: http://dx.doi.org/10.1046/j.1365-2133.1999.03033.x
2. Azulay RD, Azulay DR. Dermatologia. 2a ed. Rio de Janeiro: Guanabara Koogan; 1999. p.333-6.
3. MacKie RM. Long-term health risk to the skin of ultraviolet radiation. Prog Biophys Mol Biol. 2006;92(1):92-6. PMID: 16616325 DOI: http://dx.doi.org/10.1016/j.pbiomolbio.2006.02.008
4. Snow SN. Rotation flaps to reconstruct nasal tip defects following Mohs surgery. Dermatol Surg. 1997;23(10):916-9. DOI: http://dx.doi.org/10.1111/j.1524-4725.1997.tb00748.x
5. Festa-Neto C. Tumores cutâneos malignos. In: Cucé LC, Festa-Neto C. Manual de Dermatologia. São Paulo: Atheneu; 2001. p.441-57.
6. Walker P, Hill D. Surgical treatment of basal cell carcinomas using standard postoperative histological assessment. Australas J Dermatol. 2006;47(1):1-12. PMID: 16405477 DOI: http://dx.doi.org/10.1111/j.1440-0960.2006.00216.x
7. Parrett BM, Pribaz JJ. An algorithm for treatment of nasal defects. Clin Plast Surg. 2009;36(3):407-20. PMID: 19505611 DOI: http://dx.doi.org/10.1016/j.cps.2009.02.004
8. Zeikus PS, Maloney ME, Jellinek NJ. Advancement flap for the reconstruction of nasal ala and lateral nasal tip defects. J Am Acad Dermatol. 2006;55(6):1032-5. PMID: 17110218 DOI: http://dx.doi.org/10.1016/j.jaad.2006.08.049
9. Cordoro KM, Russell MA. Minimally invasive options for cutaneous defects: secondary intention healing, partial closure, and skin grafts. Facial Plast Surg Clin North Am. 2005;13(2):215-30. DOI: http://dx.doi.org/10.1016/j.fsc.2004.11.008
10. Zitelli JA. Wound healing by secondary intention. A cosmetic appraisal. J Am Acad Dermatol. 1983;9(3):407-15. DOI: http://dx.doi.org/10.1016/S0190-9622(83)70150-7
11. Cataldo PA, Stoddard PB, Reed WP. Use of frozen section analysis in the treatment of basal cell carcinoma. Am J Surg. 1990;159(6):561-3. PMID: 2349981 DOI: http://dx.doi.org/10.1016/S0002-9610(06)80066-8
12. Motley RJ, Gould DJ, Douglas WS, Simpson NB. Treatment of basal cell carcinoma by dermatologists in the United Kingdom. British Association of Dermatologists Audit Subcommittee and the British Society for Dermatological Surgery. Br J Dermatol. 1995;132(3):437-40. PMID: 7718462 DOI: http://dx.doi.org/10.1111/j.1365-2133.1995.tb08679.x
13. Kopf AW, Bart RS, Schrager D, Lazar M, Popkin GL. Curettageelectrodesiccation treatment of basal cell carcinomas. Arch Dermatol. 1977;113(4):439-43. PMID: 848972 DOI: http://dx.doi.org/10.1001/archderm.1977.01640040047006
14. Marchac D, Papadopoulos O, Duport G. Curative and aesthetic results of surgical treatment of 138 basal-cell carcinomas. J Dermatol Surg Oncol. 1982;8(5):379-87. DOI: http://dx.doi.org/10.1111/j.1524-4725.1982.tb00302.x
15. Rowe DE, Carroll RJ, Day CL Jr. Long-term recurrence rates in previously untreated (primary) basal cell carcinoma: implications for patient follow-up. J Dermatol Surg Oncol. 1989;15(3):315-28. DOI: http://dx.doi.org/10.1111/j.1524-4725.1989.tb03166.x
16. Kopf AW, Bart RS, Schrager D, Lazar M, Popkin GL. Curettage-electrodesiccation treatment of basal cell carcinomas. Arch Dermatol. 1977;113(4):439-43. PMID: 848972 DOI: http://dx.doi.org/10.1001/archderm.1977.01640040047006
17. Romaní J, Yébenes M. Repair of surgical defects of the nasal pyramid. Actas Dermosifiliogr. 2007;98(5):302-11. DOI: http://dx.doi.org/10.1016/S1578-2190(07)70453-5
18. Rohrich RJ, Griffin JR, Ansari M, Beran SJ, Potter JK. Nasal reconstruction--beyond aesthetic subunits: a 15-year review of 1334 cases. Plast Reconstr Surg. 2004;114(6):1405-16. DOI: http://dx.doi.org/10.1097/01.PRS.0000138596.57393.05
19. Knighton DR, Silver IA, Hunt TK Regulation of wound-healing angiogenesis-effect of oxygen gradients and inspired oxygen concentration. Surgery. 1981;90(2):262-70.
20. van der Eerden PA, Verdam FJ, Dennis SC, Vuyk H. Free cartilage grafts and healing by secondary intention: a viable reconstructive combination after excision of nonmelanoma skin cancer in the nasal alar region. Arch Facial Plast Surg. 2009;11(1):18-23. DOI: http://dx.doi.org/10.1001/archfacial.2008.501
21. Jung W, Winter H. Considerations for the use of clostridial collagenase in clinical practice. Clin Drug Invest. 1998;15(3):245-52. DOI: http://dx.doi.org/10.2165/00044011-199815030-00009
22. Ferreira AM, Souza BMV, Rigotti MA, Loureiro MRD. Utilização dos ácidos graxos no tratamento de feridas: uma revisão integrativa da literatura nacional. Rev Esc Enferm. USP. 2012;46(3):752-60.
23. Juchem PP, Hochberg J, Winogron A, Ardenghy M, English R. Riscos à Saúde da Radiação Ultravioleta. Rev Bras Cir Plást. 1998;13(2):31-60.
24. Radwanski HN, Correa WEM, Refosco TJ, Farrapeira Júnior A, Pitanguy I. Silicone gel em cicatrizes de cirurgia plástica: estudo clínico prospectivo. Rev Bras Cir Plást. 2010;25(3):428-33. DOI: http://dx.doi.org/10.1590/S1983-51752010000300005
Universidade Federal de Mato Grosso do Sul, Campo Grande, MS, Brazil
Clinica Particular, Campo Grande, MS, Brazil.
Corresponding author:
Daniel Nunes
Rua da Paz, 129 - Jardim dos Estados
Campo Grande, SP, Brazil Zip Code 79002-190
E-mail: dermatoplastica@gmail.com
Article received: May 10, 2015.
Article accepted: November 20, 2015.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter