

Original Article - Year 2016 - Volume 31 -
Strategies in complex reconstructions of the scalp and forehead: a series of 22 cases
Estratégias em reconstruções complexas do couro cabeludo e da fronte: uma série de 22 casos
ABSTRACT
INTRODUCTION: The cephalic region is exposed to various insults from the environment. Extensive lesions in the scalp are a great challenge for plastic surgeons, because the low mobility of the skin in this region hampers its closure. A great variety of techniques have been used to close defects on the scalp and forehead. Ideally, scalp closure should provide a better functional and aesthetic outcome, as well as low morbidity at the donor site.
METHODS: From January 2006 to December 2014, we performed a retrospective clinical study involving a series of 22 patients with advanced tumors of the scalp or forehead, or with extensive post-trauma skin loss.
RESULTS: Reconstructive surgeries with 11 local scalp flaps (bi- or tri-pedicled), three coronal forehead flaps, and eight free flaps were performed. One patient experienced late partial loss of a free flap after radiotherapy.
CONCLUSION: Various techniques can be used to reconstruct the scalp and forehead; each case should be assessed individually. The present study indicated that flaps are safe and that they confer low morbidity at the donor area. These results were satisfactory and in agreement with the literature analyzed.
Keywords: Scalp/surgery; Microsurgery; Surgical flaps; Head and neck tumors; Reconstructive surgical procedures.
RESUMO
INTRODUÇÃO: A região cefálica está exposta a insultos de ordem variada por parte do meio ambiente. As lesões extensas no couro cabeludo representam um grande desafio ao cirurgião plástico devido à pouca mobilidade da pele nesta região, o que dificulta o seu fechamento. Uma grande variedade de técnicas tem sido utilizada para o fechamento de defeitos no couro cabeludo e na fronte. A técnica ideal deve visar o melhor resultado funcional, estético e baixa morbidade do sítio doador.
MÉTODOS: Foi realizado um estudo clínico retrospectivo no período de janeiro de 2006 a dezembro de 2014, de uma série de 22 casos com tumores avançados do couro cabeludo e da fronte e perda cutânea extensa pós-trauma.
RESULTADOS: Foram realizados 11 retalhos locais de couro cabeludo (bi ou tripediculados), três retalhos coronais da fronte e oito retalhos livres. Houve um caso de perda parcial tardia de um retalho livre pós-radioterapia.
CONCLUSÃO: Diferentes técnicas para a reconstrução do couro cabeludo e da fronte são possíveis, cada caso deve ser avaliado individualmente. Os retalhos apresentados foram considerados seguros e com pouca morbidade da área doadora. Os resultados obtidos foram satisfatórios e estão de acordo com a literatura analisada.
Palavras-chave: Couro cabeludo/cirurgia; Microcirurgia; Retalhos cirúrgicos; Neoplasias de cabeça e pescoço; Procedimentos cirúrgicos reconstrutivos.
Because they comprise the uppermost part of the body, the head and neck are exposed to various insults from the environment. Extensive lesions of the scalp are a great challenge for plastic surgeons, because the low mobility and extensibility of the skin in this region hinders the closure of moderate to large lesions1-4.
With regard to etiology, most traumatic lesions on the face arise from car accidents; many more are caused by dog bites, mainly in children. In addition, the incidence of skin tumors has increased worldwide, and most of these are located on the face. Severe lesions of the scalp, on the other hand, are caused by electrical burns, dog bites, industrial machinery accidents, and resection of extensive tumors, among other causes. In any case, lesions of the face or scalp constitute a serious situation, and they are often associated with important sequelae5.
A large variety of techniques has been used to close defects on the scalp and forehead. Ideally, reconstruction depends on careful assessment of the following factors in each case: age, etiology, location, comorbidity, lesion extension, and the number of anatomic planes involved1,4. The reconstruction technique chosen should provide the best functional and aesthetic result possible, with minimal donor site morbidity5,6.
OBJECTIVE
The objective of this study was to present a series of techniques for reconstructing extensive defects in the scalp and forehead, as well as to report the results of several reconstructions carried out after resection of malignant tumors, or following trauma.
METHODS
This retrospective clinical study was performed at the Walter Cantídio University Hospital, Fortaleza, Brazil, from January 2006 to December 2014; the study involved a series of 22 consecutive patients diagnosed with advanced tumors of the scalp or forehead, or with extensive post-trauma skin loss.
All patients included had extensive injuries or loss of periosteum requiring repair using local flaps or microsurgical patches. The following parameters were studied: sex, age, diagnosis, lesion location, repair strategy, complications, and current clinical state. This study was approved by the Ethics Committee of the Walter Cantídio University Hospital, under protocol Nº. 041.04.15.
RESULTS
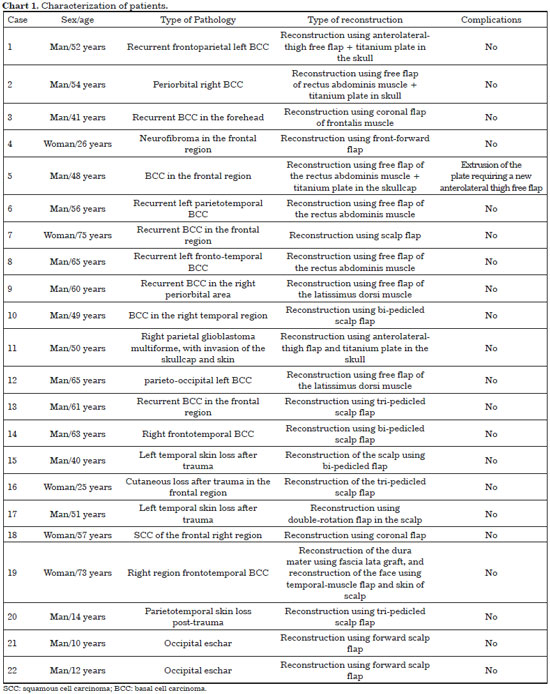
The sample comprised 22 patients (17 men; 77.2%), with ages ranging from 10 to 75 years (mean: 47.5 years). In the case series studied, the most prevalent type of tumor was basal cell carcinoma (81.2% of tumor cases); among the cases of post-trauma skin loss, motorcycle accident was the most common cause (66.6% of trauma case) (Chart 1).
Initially, reconstructive surgeries were performed with 11 flaps of the scalp (bi- or tri-pedicled), three coronal flaps, two free flaps of the latissimus dorsi muscle, two anterolateral thigh free flaps, and four free flaps of the rectus abdominis muscle.
In all cases, the extensive defects of the scalp and forehead were effectively covered. One patient experienced late loss of a free flap of the rectus abdominis muscle, with extrusion of the titanium plate; a new anterolateral-thigh free flap was constructed to cover the defect. The postoperative recovery period ranged from 20 to 60 days. Regarding the functional and aesthetic aspects, all patients presented good results, with minimal morbidity at the donor area.
DISCUSSION
The cephalic segment is covered by distinct anatomical structures that can be broadly divided into soft parts (the scalp and by the forehead and their respective layers), and bone tissue (the skullcap)6-8. The forehead is the anterior region of the skull, extending from the eyebrows to the point where hair grows. This region is subject to trauma, as well as to sun exposure, which increases the risk skin tumors.
The scalp is unlike the forehead in that there are more hair follicles; furthermore, the dermis is thicker and it is irrigated by vascular pedicles, which are formed by the superficial temporal, supraorbital, supratrochlear, posterior, and occipital auricular vessels. The skullcap is formed by the frontal, parietal temporal, and occipital bones, and covers the brain6,9-12.
The cephalic region is constantly exposed to various insults, from traumas of various types to solar exposure; this predisposes it to skin tumors and infection. The lesions caused by such insults cause huge functional and aesthetic damage in this region of the body, particularly since it is a highly visible area5,6,10-12. Because of the socioeconomic situation of the Brazilian population, advanced tumors of the head and neck constitute a serious reality. Most are tumors of skin origin, mainly caused by the tropical climate and by the ethnic variability in Brazil. Basal cell carcinoma is the most common type of skin cancer, followed by squamous cell carcinoma4-6. In our case series, 80% of the tumors of the scalp and forehead were basal cell carcinomas; this corroborates the literature analyzed.
Loss of tissue in the scalp is difficult to resolve, because scalp tissue has a low extensibility. However, with recent advances in flaps, grafts, and microsurgery techniques, surgeons can now achieve excellent results: not only can they cover the noble structures, they can also preserve the form and contours, thus ensuring aesthetics and improving the quality of life of the patient4,6.
Many different lesions can occur on the scalp and forehead, and various techniques, with different degrees of complexity, can be used to treat such lesions. Specifically, small lesions that do not expose the noble structures can be effectively resolved using flaps or local grafts; however, extensive lesions-or those that expose such structures as the skullcap, vessels, or dura mater-require repair using a more elaborate or distal flap4,5.
For minor defects less than three centimeters in diameter, primary closure is the best option. In such cases, skin grafting provides a quick and effective means of closure; although this approach requires a properly vascularized bed. Tissue expansion followed by flap rotation provides ample tissue, while preserving the sensitivity of the scalp, as well as color, thickness, and hair. However, this requires multiple surgical procedures.
Local flaps are indicated in the reconstruction of small-to-medium defects; these can be random when they do not have a defined or axial pedicle, in which there is a defined vascular pedicle. In cases of large flaps, the donor area is covered using a skin graft4-6. In the present study, 11 local flaps of the scalp (50% of cases) were performed to treat skin loss in this region (Figure 1); three local coronal flaps (13.6% of cases) were also performed to treat closure of defects on the forehead (Figures 2 and 3). In all cases, there was a good coverage of the receptor bed and there were no complications.

Figure 1. Skin loss in parietotemporal scalp region after trauma, reconstruction using double-rotation flap.

Figure 2. Recurrent BCC in frontotemporal region, resection and reconstruction using coronal-rotational flap.

Figure 3. Neurofibromatosis in the frontal region, resection and reconstruction using forward coronal flap.
Using free flaps, defects that cover more than 50% of the scalp can be closed in a single procedure; free flaps also provide the best results and healing in areas of prior radiation, or in cases of infection4-6. There are numerous donor sites for free flaps: the parascapular area, large dorsal, abdominis rectus, omental sites, etc. Flaps from the abdominis rectus muscle, as well as those from the latissimus dorsi muscle, present certain advantages: they provide a large amount of tissue, have a long, good-caliber pedicle, and possess great versatility (they can be used in a variety of situations). Total or partial necrosis of the flap is one of the most important complications of this type of procedure5,6.
In the series studied, eight free flaps (36.3%) were carried out to cover the scalp and forehead; no immediate complications occurred, such as partial or total loss of flaps (Figures 4-6). However, in one patient who had undergone reconstruction of the forehead using a free flap of the abdominis rectus muscle, the cranioplasty plate used to reconstruct the frontal bone became exposed. The patient required a salvage reconstruction using a free anterolateral thigh flap (Figure 7).

Figure 4. Resection of intracranial glioblastoma, frontotemporal reconstruction using synthetic dura mater, cranioplasty plate and microsurgical anterolateral-thigh flap.

Figure 5. Basal cell carcinoma in frontal bone and right orbit, resection and reconstruction of the skull using a synthetic dura-mater graft and cranioplasty plate, reconstruction using microsurgical flap of the abdominis rectus muscle and skin graft.

Figure 6. Recurrent BCC in frontotemporal left region, resection and reconstruction of the skull using synthetic dura mater, cranioplasty plate, free flap of the abdominis rectus muscle, and skin graft.

Figure 7. Frontal BCC and in the right orbit, resection and reconstruction of the frontal bone using a cranioplasty plate and free flap of the rectus abdominis muscle, with posterior skin grafting. Extrusion of the cranioplasty plate developed after radiotherapy, and the lesion was again reconstructed using a microsurgical anterolateral-thigh flap.
CONCLUSION
Many different techniques can be used to cover the scalp and forehead; surgeons must use the simplest possible reconstruction in each case. That is, each patient should be assessed individually, and the best reconstruction must be decided, taking into account morbidity, available resources, and acceptable aesthetic results.
The transposition of free muscle flaps to reconstruct large lesions is quite effective, and an excellent treatment choice. The present study indicated that flaps are safe, and there was low morbidity at the donor area; therefore, free muscle flaps are effective in the reconstruction of large defects of the scalp and forehead. The results obtained were satisfactory and corroborate the literature analyzed.
COLLABORATIONS
CAM Analysis and/or data interpretation; statistical analysis; final approval of the manuscript; conception and design of the study; completion of operations and/or experiments; writing of the manuscript or critical review of its contents.
SGPP Conception and design of the study; critical review of study contents.
BBGPP Conception and design of the study; critical review of study contents.
REFERENCES
1. Bazzi K, Formighieri B, Tissiani LAL, Rocco M, Ferreira MM, Vilella L. Reconstruções complexas do couro cabeludo: um desafio ao cirurgião plástico. Rev Bras Cir Plást. 2010;25(3 Supl 1):28.
2. Maia Neto JD, Carvalho FAM, Nogueira RP, Haad NS, Teixeira JAL, Heli E. Experiência do IJF na Reconstrução de lesões graves em couro cabeludo. Rev Bras Cir Plást. 2013;28(3 Supl 1):20.
3. Dos Santos LF, Amorim Junior MAP, Batista OB, Leite LAS. Retalho de nuca para reconstrução de lesões de couro cabeludo. Cir Plást Iberolatinoam. 2010;36(3):263-72.
4. Anbar RA, Almeida KG, Nukariya PY, Anbar RA, Coutinho BBA. Métodos de reconstrução do couro cabeludo. Rev Bras Cir Plást. 2012;27(1):156-9. DOI: http://dx.doi.org/10.1590/S1983-51752012000100026
5. Franciosi LFN, Weber ES, Righesso R, Pizzoni VRS, Molon MP, Piccoli MC. Reparação do escalpo por retalhos livres microcirúrgicos. Rev Bras Cir Plást. 2010;25(4):624-9. DOI: http://dx.doi.org/10.1590/S1983-51752010000400010
6. Souza CD. Reconstrução de grandes defeitos de couro cabeludo e fronte em oncologia: tática pessoal e experiência - análise de 25 casos. Rev Bras Cir Plást. 2012;27(2):227-37. DOI: http://dx.doi.org/10.1590/S1983-51752012000200011
7. Iribarren BO. Reconstrucción de cuero cabeludo. Cuad Cir. 2000;14(1):80-9.
8. Sakai S, Soeda S, Terayama I. Subcutaneous pedicle flaps for scalp defects. Br J Plast Surg. 1988;41(3):255-61. DOI: http://dx.doi.org/10.1016/0007-1226(88)90109-9
9. Lutz BS, Wei FC, Chen HC, Lin CH, Wei CY. Reconstruction of scalp defects with free flaps in 30 cases. Br J Plast Surg. 1998;51(3):186-90. PMID: 9664876 DOI: http://dx.doi.org/10.1054/bjps.1997.0182
10. Temple CL, Ross DC. Scalp and forehead reconstruction. Clin Plast Surg. 2005;32(3):377-90. DOI: http://dx.doi.org/10.1016/j.cps.2005.02.002
11. Seitz IA, Gottlieb LJ. Reconstruction of scalp and forehead defects. Clin Plast Surg. 2009;36(3):355-77. PMID: 19505608 DOI: http://dx.doi.org/10.1016/j.cps.2009.02.001
12. Angelos PC, Downs BW. Options for the management of forehead and scalp defects. Facial Plast Surg Clin North Am. 2009;17(3):379-93. DOI: http://dx.doi.org/10.1016/j.fsc.2009.05.001
1. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
2. Hospital Universitário Walter Cantídio da Universidade Federal do Ceará, Fortaleza, CE, Brazil
Institution: Universidade Federal do Ceará, Fortaleza, CE, Brazil.
Corresponding author:
Caio Alcobaça Marcondes
Rua Luiza Amélia Brandão, 916 - São Cristóvão
Teresina, PI, Brazil Zip Code 64056-170
E-mail: caio_alcobaca@hotmail.com
Article received: April 17, 2015.
Article accepted: May 11, 2016.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter