

Original Article - Year 2016 - Volume 31 -
Breast augmentation after bariatric surgery by using complementary prosthetic support for glandular containment
Mamoplastia pós-cirurgia bariátrica usando suporte protético complementar de contenção glandular
ABSTRACT
INTRODUCTION: The skin presents structural and proteomic changes after bariatric surgery and cannot withstand the weight of the breasts, which leads to early residual flaccidity, requiring auxiliary support. The goal is to apply a nonabsorbable polypropylene-poliglecaprone absorbable auxiliary mesh support or Bustos silicone sheet, in the form of an "internal brassiere," to support the skin in order to maintain the shape and flaccidity of the breasts comparable with those of normal breasts.
METHODS: Nine patients underwent mammoplasty in inverted T with modeling of tissue implants, reduction of breast volume, and wrapping with an auxiliary support mesh.
RESULTS: Flaccidity was not observed at an early stage and the condition was acceptable for up to 4 years of follow-up. One of the patients had a seroma, which was drained with good resolution. Another 24 patients will be operated according to the protocol and observed for 2 years by using mammography, ultrasonography, and magnetic resonance imaging.
CONCLUSION: Reduction mammoplasty after bariatric surgery requires additional support for the mammary gland. The structurally altered skin could not support the weight of the breasts, resulting in early flaccidity.
Keywords: Bariatric surgery; Mammoplasty; Human mammary glands; Prostheses and implants.
RESUMO
INTRODUÇÃO: A pele de pacientes emagrecidas pós-cirurgia bariátrica apresenta alterações estruturais e proteômicas e não resiste ao peso das mamas, levando-as à flacidez residual precoce, exigindo suporte auxiliar. O objetivo é aplicar suporte auxiliar de lâmina de polipropileno não absorvível mais poliglecaprone absorvível ou lâmina de silicone de bustos, em forma de "soutien interno" como auxiliar de sustentação da pele, para manutenção da forma das mamas, e flacidez no mínimo comparável a outras pacientes sem emagrecimento pela cirurgia bariátrica.
MÉTODOS: Nove pacientes foram submetidas à mamoplastia em T invertido com modelagem dos tecidos mamários, com redução do volume e envolvidos com lâmina de sustentação auxiliar.
RESULTADOS: Não houve flacidez precoce e em observação de até 4 anos ela era aceitável. Uma delas apresentou seroma, drenado com boa resolução. Serão operadas outras 24 pacientes dentro do protocolo, acompanhadas e observadas por 2 anos com controle mamográfico, ultrassônico e ressonância magnética.
CONCLUSÃO: A mamoplastia redutora pós-cirurgia bariátrica requer suporte extra à glândula mamária. A pele estruturalmente alterada não suporta o seu peso e haverá flacidez precoce.
Palavras-chave: Cirurgia bariátrica; Mamoplastia; Glândulas mamárias humanas; Próteses e implantes.
After bariatric surgeries and major weight loss in female patients, breasts become flaccid. If we perform reduction surgery with pexy or reduction surgery alone, the results are poor in the medium and long terms. The breasts quickly present ptosis, beyond that expected in similar procedures in patients who did not undergo these surgeries, because the skin of these patients present significant structural alterations and do not withstand the weight of the breasts.
The thickness of the dermal skin layer is reduced1. Comparative proteomic analysis of the skin2 with immunohistochemical validation of proteins from samples taken from the abdomens of morbidly obese patients, morbidly obese patients who lost weight naturally, and morbidly obese patients who lost weight via bariatric surgery confirmed the existence of differences in the molecular composition of the skin of these patients.
The analysis in 113 proteins showed that reduced alpha 1 antitrypsin, collagen XIV, vinculin, periplakin, anexina A5, and haptoglobin levels and predominantly inflammatory chronic tissue injury of the skin that begins with obesity are perpetuated even with weight loss, especially after bariatric surgery. Levels of haptoglobin, an inflammatory protein in systemic diseases, is increased up to 70-fold after bariatric surgery.
The reduction in the thickness of the dermal tissue in patients thinned by surgery1 seems to be selective, indicating sui generis clinical characteristics of the skin of these patients as follows: thickness reduction, chronic inflammatory lesions, and structural and functional changes in the proteome of the cutaneous tissue responsible for the loss of quality and elasticity.
Hence, an auxiliary support for the skin is required so that both the aesthetic results of mammoplasty and residual flaccidity are adequate and durable.
Bustos3, in 1986, was the first to develop a silicon-supporting sheet in the form of an open brassiere and used it with good results in breast augmentation; this approach required incision and resection only of the periareolar skin and the breast was modeled with this sheet, between the gland and the subcutaneous skin. Other authors have used de-epidermized skin for double coverage of the breasts4-6, but long-term support is not fully maintained. Other products were used in the same way with the same purpose, some mixed (polyglactine 60% and polyester 40%), partly absorbable and non-absorbable7, even with mammographic assessment8. Fully absorbable layers have also been used9-11.
Alloplastic mesh is used primarily in the correction of inguinal or ventral hernias12-14. Some authors15,16 have studied the organic reactions produced by the presence of a non-absorbable mesh and cited it as the ideal implant, causing a natural initial inflammatory reaction in any kind of implant, including silicone implants (biological reaction to a foreign body), heading toward "definitive integration."
Periareolar mammoplasties have been discontinued. Brazilian patients and virtually all patients worldwide have come to prefer larger breasts, with reversal of treatment requests. Currently, the aesthetic demands are now breast augmentation with prostheses for breasts already subjected to periareolar reduction surgery.
However, the emergence and growth of bariatric surgeries with extensive weight loss have caused some aesthetic and functional distortions to plastic surgeries such as mammoplasty, which are difficult to resolve.
For patients who have undergone bariatric surgery with extensive weight loss, the author proposes to perform mammoplasties with skin resection and inverted T-shaped final scars to provide "anatomical" shape to the breasts, with or without resection of volume, and apply a support in the form of an "internal bra" with a non-absorbable polypropylene mesh with absorbable poliglecaprone- or polyurethane-coated silicone sheet, described by Bustos, and cover it with skin and subcutaneous tissue.
These meshes are soft and delicate, have high tensile strength, have good biological integration, are the first to become available in hospitals, are easy to handle, and are not radiopaque and allow preventive breast examinations such as mammography, ultrasonography, and magnetic resonance imaging. They may provide additional support for breasts operated after extensive weight loss after bariatric surgery.
OBJECTIVE
To demonstrate the possibility of using a nonabsorbable polypropylene mesh with an absorbable poliglecaprone or Bustos silicone sheet, in the shape of an "internal brassiere" as an aid to support the skin to maintain the shape of the breasts, with flaccidity at least comparable with that in other patients without weight loss by bariatric surgery.
METHODS
Nine patients who underwent bariatric surgery (2010-2015) and had extensive weight loss and, consequently, great flaccidity of the skin and breasts were selected from the plastic surgery clinic of the Hospital de Base of the Faculty of Medicine of São José do Rio Preto, SP.
Duly released by the Department of Bariatric Surgery, the most important inclusion parameter was large breast flaccidity, with sufficient volume to recompose the breasts or excess volume, and stabilized body weight. The technique to be performed was explained to the patients and informed consent was obtained. The excluded patients were those whose weights had not stabilized yet, who had diabetes mellitus, who had uncontrolled hypertension, who were smoking, who had autoimmune diseases and other pathologies for which surgery is contraindicated. Those who had doubts about the difference between surgery with and without the use of the mesh underwent classical surgery without the mesh.
Anatomically perfect breast shape
Three geometric figures based on the Phi (1/1.618) ratio, also called the golden or divine proportion, served as the basis for the three-dimensional view (front, side, and vertical; (Figure 1A, B, C, D, E, and F) of the anatomically perfect breast, providing proportion and beauty, and reflecting possible "aesthetic distortions" on the study of their shape17.
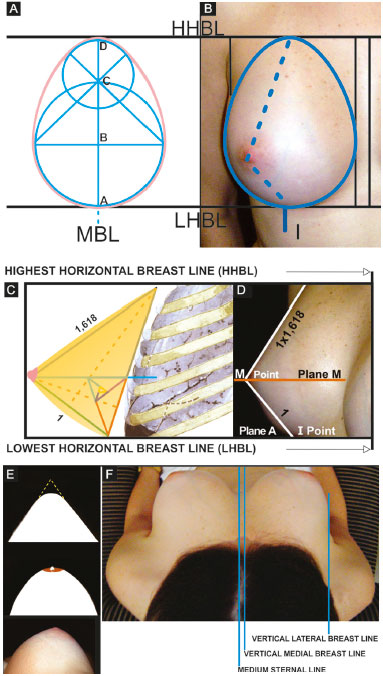
Figure 1. A and B: Frontal view of an anatomically perfect breast with the vertical breast meridian line between the horizontal breast lines; C and D: Anatomically perfect breast in side view and the proportion between the lower and upper pole, between the horizontal breast lines; E and F: Vertical view of the anatomically perfect breast between the vertical breast lines resembling a cone.
MBL: Meridian Breast Line.
Source: Rev. Bras. Cir. Plást. 2011; 26(1): 94-103.
Figure 1 (A and B) shows the front view of an ideal breast with a "golden ovoid" shape. In the projection of two partially superimposed circles on which the Phi ratio (1/1.618) applies on the vertical axes (AD is for BD as BD is for CD) to obtain the "golden ovoid" shape17. The basis of the form of the breast in the frontal view is as follows: at a ratio of 1 to 1.3 between the horizontal and vertical axes, respectively.
The ABCD axis is the breast meridian line (BML) that lies between two other horizontal lines, namely the lowest horizontal breast line (LHBL), which joins the inframammary grooves at the junction of the breast meridians (points I), and the highest horizontal breast line (HHBL), which unites the highest part of the two anterior axillary folds. The vertical measure between these two lines is unique for each patient, determining the vertical extension of the base of the breast. By applying the ratio of 1 to 1.3 on it, the lateral extension can be proportionally obtained.
The front view of the breast shows ptosis with skin flaccidity, inverted vertical and horizontal axes, increased vertical and horizontal axes, and reduced cleavage. Point I is not altered.
The side view of the ideal breast shows the "golden triangle," which is recognized throughout the history of Phi (Figure 1C and D). The bisection of the angle of the base divides the contralateral side into two parts containing the Phi ratio between them. In the side view, the normal sternum-ribcage, in the anterosuperior region, anatomically has a slope of approximately ± 15° to 18° in relation to the vertical axis of the body, depending on the ribcage and spine in the region of breast implantation (Figure 1D)17.
When the golden triangle is tilted under this angle in the vertical plane, it will resemble an ideal breast profile. A normal breast without ptosis, in side view, is above horizontal plane A (LHBL; Figure 1C). Plane A coincides with point I (intersection of the breast meridian with the inframammary fold). Another horizontal plane (M) crosses the apex of the breast cone and divides the breast into the upper and lower segments.
When it crosses the breast meridian, it determines point M, where in general, the papilla is placed (this and the areola can be ectopic, i.e., outside the apex of the cone). From the apex of the cone to point I, ideal breasts without ptosis have ideal measurements between 7 and 12 cm. These may vary among countries, eras, and fashions. Smaller measurements determine smaller breasts and vice versa, however appropriate. The upper breast segment from the apex of the cone to the HHBL measures 1.618-times greater than the measurement of the bottom segment (Figure 1C)17. It is the Phi ratio again.
The "golden cone" determines the vertical view of an ideal breast, as seen by the patient herself when looking from top to bottom (Figure 1E). Five golden triangles joined by one of its sides and apexes form a pentagon "golden pyramid" (Figure 1F). If turned on the vertical axis, they form what can be called a "golden cone." This cone, with rounded sides, resembles the breast from a vertical view. The normal and ideal breast lies between two vertical lines, namely the vertical lateral breast line, which coincides with the anterior axillary line, and the vertical medial breast line (VMBL), which is located 1 to 1.5 cm laterally to the mid-sternal line (Figure 1E).
A breast under this three-dimensional view is what we attempt to obtain with surgical modeling and maintain with the aid of a polypropylene mesh because after weight loss by bariatric surgery, the skin does not have sufficient strength to do so.
Quantification and measurement of breast ptosis
The breast, when growing during puberty, projects into the anterior space of the thorax and is be larger or smaller according to the hormonal stimulus and number of buds. It is more or less designed with the variation of the skin's resistance to the expansion of the breast. In resistant skin, the breasts tend to be GII (wide base with little projection); and in thin skin, the breasts tend to be GIII (narrow base with significant projection)17. An example of this blockade of mammary projection is skin that has suffered burns; the breast is deformed and has no projection in the areas of fibrosis, which block its anteroposterior growth.
In the initial phase of breast development, they project above the LHBL and point I (Figure 2A). Depending on the type of skin or causes that make it resistant, such as environmental exposure, sun, smoking, large variations in weight, bariatric surgery, pregnancy, aging, systemic diseases, and breast volume. The breasts progressively overtake the LHBL and point I inferiorly through their apexes (Figure 2B). The vertical diameter of the breast is reduced, its horizontal diameter increases, and the cleavage empties. The ideal breast, which is "vertical," then becomes horizontal.
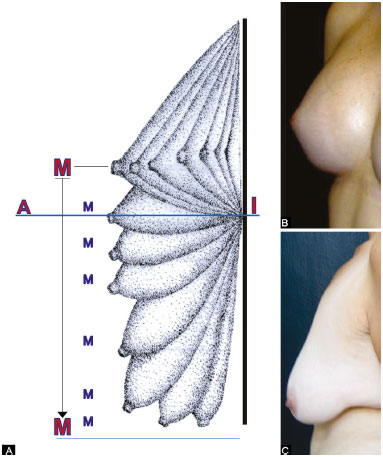
Figure 2. A: Diagram of the evolution of the breast over time and modifications of points A, M, and I in relation to the inferior horizontal breast line; B: An anatomically perfect breast; C: A flaccid breast below the LHBL.
LHBL: Lowest Horizontal Breast Line
Point I never changes with the evolution of flaccidity and, when projected on the breast with volume below the LHBL, determines point A of Pitanguy18 on its meridian (Figure 2C).
The breast cone more projected on the meridian determines point M. It does not refer to the nipple because the nipple areola complex can be ectopic in relation to the breast cone, in the downward, upward, lateral, or medial direction.
The measurement in centimeters between points A and M quantifies the extent of skin to be removed to raise the ptosed breast above the LHBL and, therefore, from point I (Figure 2C)19,20.
When the measurement between A and M is < 3 cm, it is possible to perform a vertical mammoplasty by sectioning only once a vertical skin spindle, with periareolar resections.
When the measurement of AM is between 3 and 7 cm, excess skin can be removed with a vertical hemispindle and the other lateral hemispindle, called mammoplasty in L shape19,20.
When the measurement of AM is >7 cm, the resection of excess skin is performed with vertical and horizontal spindles, called mammoplasty in inverted T shape.
We selected patients who underwent bariatric surgery and major weight loss, with AM measuring >10 cm.
Surgery
Skin marking
With the patient standing with arms raised (Figure 3A), the following marks are made:
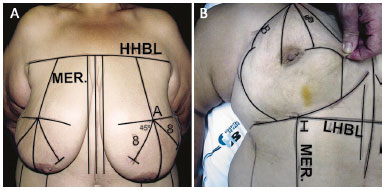
Figure 3. A: Marking of the skin resections with guidelines and points; B: Final marking.
HHBL: Highest Horizontal Breast Line; LHBL: Lowest Horizontal Breast Line; MER.: Meridian.
1. The HHBL, which unites horizontally the anterior axillary folds (HHBL);Still with the patient standing, from point A, mark two oblique descending lines, one medial and the other lateral at an angle of 90° between them (Figure 3A). The meridian of the breast divides this right angle into two others at 45°. Mark 8 inches on each side of these lines, in the lower medial oblique and lateral directions; these are points B and C18. From these marks, mark two vertical curved lines up to the submammary groove, the lateral concave to the medial concave and the medial concave to the lateral concave (Figure 3B).
2. The submammary groove;
3. The VMBL, 1 to 1.5 in on each side of the midline on the external bone, and the lateral vertical breast lines, which coincide with the anterior axillary lines;
4. The BML, which divides the breasts in half, midway between the lateral and medial vertical lines;
5. Point I (intersection of the meridian with the line of the submammary groove);
6. The LHBL (union between the two points I);
7. The projection of point I on the breasts that determine point A18, obtained by placing the tip of the index finger on point I and the end of the thumb on the breast in horizontal line;
8. Point M. These lines and points are the guides for skin resection and breast placement on the chest19,20.
Surgical procedure
With the patient in HDD arms abducted 90° position, mark the areola diameter as more or less 4 cm with skin stretched. The whole skin contained within the marking is de-epidermized (Figure 4A).
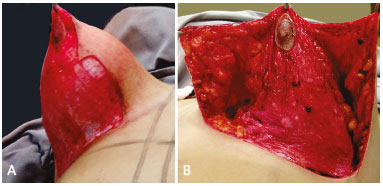
Figure 4. A: De-epithelization of the marked area; B: Raising of the upper flap. In this case, the areola stayed in the lower pedicle.
The skin between points B and C, and the vertical curved markings is incised up to the submammary groove. The skin and subcutaneous tissue are detached up toward the HHBL, starting with the thickness of the subcutaneous tissue of the patient's chest and increasing it slightly, homogenously, and gradually, taking with it the de-epidermized areolar pedicle (Figure 4A and B). The aponeurosis of the greater pectoral muscle on the side is exposed from the submammary groove to the upper part, peeling the skin and subcutaneous tissue of the mammary gland. The same procedure is carried out on the medial side.
In the lateral and medial detachments, only the thickness of the subcutaneous tissue of the chest of the patient is monitored.
The breast volume is attached to the pectoral muscle with their lower and pectoral pedicles and should be modeled. Sometimes sectioning parts of it in the lateral and medial portions of the gland (ERFON), thus reducing its laterolateral diameter. When reduction is not needed, these portions are transposed and sutured in the vertical direction to shape the breast cone. Occasionally, part of the top pole is resected if the volume still needs to be reduced. The central portion of the breast in the breast meridian is not detached from the thoracic plane from point I to the HHBL. This portion has major blood vessels that supply the breast tissue.
All this "central" tissue is modeled to provide the shape of the perfect breast, with sutures absorbable in the medium term, as needed, by using the de-epidermized skin (Figure 5A). The vertical diameter should be proportionally larger than the horizontal diameter by 1.3/1. Care must be taken not to strangle the inferior axial circulation21.
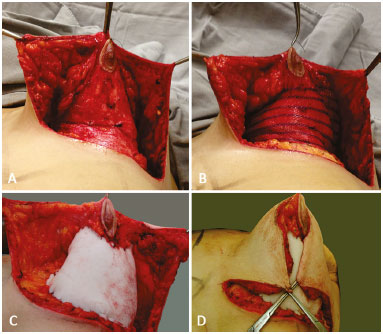
Figure 5. A: Mounting of breast tissue; B: Breast volume filling with a polypropylene-poliglecaprone mesh; C: Filling with a polyurethane-coated silicone sheet; D: Lowering of the upper flap covering of the breast shape.
Thus, with the aponeurosis of the greater pectoral muscle fixed on the BML, cone-shaped tissue implants will be covered by the polypropylene-poliglecaprone mesh in the form of an "internal brassiere" (Figure 5B) or with a Bustos silicone sheet (Figure 5C), fastened with nonabsorbable sutures to the muscle aponeuroses.
The suture begins at point I. The edge of the mesh is sutured along the groove, continuing with the lateral and medial sutures of the mesh, the medial and lateral aponeurosis of the greater pectoral muscle, followed by the vertical lateral and BMLs. The upper part of the mesh is not sutured together, leaving space for distension of the volume contained therein because of postoperative edema.
The upper flap containing the areola descends and covers the modeled cone and the mesh (Figure 5D), suturing the lateral and medial aspects of the skin between them from point A downward, until the vertical dimension of the scar adjusts to the height of the modeled cone.
Any excess skin and subcutaneous tissue are resected, following the edge of the modeled breast and completing the inverted T shape.
The areola is always away from point A (the apex of the cone), but as it undergoes a large retro-areolar emptying22, it will rise to its ideal position. If this does not occur, part of the de-epidermized skin can be incised to the side, or medially, which is more convenient, thus creating an areolar pedicle until it fits to its new position, without traction, torsion, or excessive compression. If this is not possible, free grafting of the areola and papilla is performed.
The areola should be relocated at the apex of the cone because the mesh does not allow tilting of the breast (Figure 6A and B).

Figure 6. A: Completed sutures, drainage, and aspiration, and in this case, grafting of the areola; B: Postoperative appearance after suture removal.
Drainage may be required. Subcutaneous and intradermal sutures with thin absorbable sutures and skin closure with nonabsorbable sutures complete the surgery.
Dressing is applied with adhesive tape in the form of a brassiere, which will be removed after about 8 to 9 days with the removal of sutures, which upon completion of the surgical procedure, is filled with ointment containing 30 mg/g oxytetracycline and 10 mg/g hydrocortisone. Another elastic brassiere, which has no seams, is used for 2 months on top of the tapes. During this time, the adhesive tapes are used on the scars as a containment mechanism of the skin to prevent scar enlargement.
Approval number of the CEP: CAAE 43647115.0.0000.5415.
RESULTS
Nine patients were operated on. In three of these patients, a polyurethane-coated Bustos silicone sheet was used; and in the six others, a polypropylene-poliglecaprone mesh was used. The three cases in which a silicone sheet was used were followed up for 2, 3, and 4 years. The cases where a polypropylene-poliglecaprone mesh was used were followed up for > 6 months. In the patients shown in Figures 7A-F and 8A-F, a polypropylene-poliglecaprone mesh was used; and in the patients shown in Figures 9A-F and 10A-F, a silicone sheet was used.
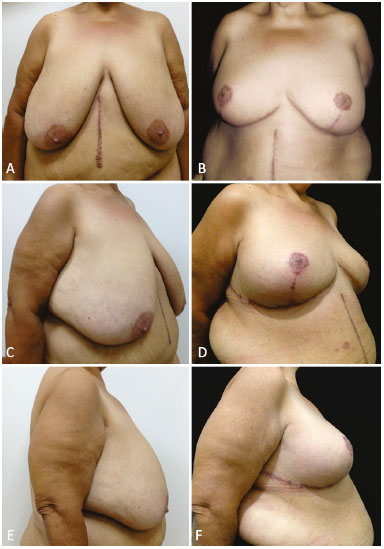
Figure 7. A, B, C, D, E and F: Preoperative and 6-month postoperative aspects of the patients in Figures 6A and B, with the use of a polypropylene-poliglecaprone mesh. Resection of 1500 g of tissue from each breast.
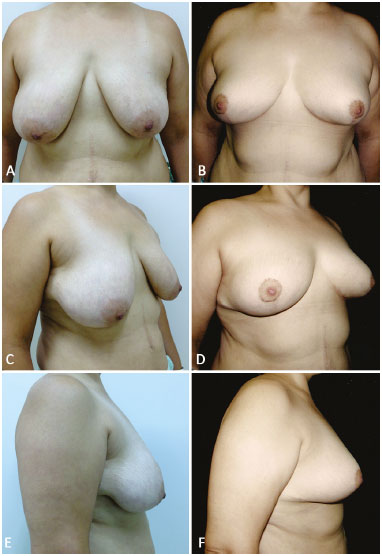
Figure 8. A, B, C, D, E and F: Preoperative and 6-month postoperative aspects with the use of a polypropylene-poliglecaprone mesh.
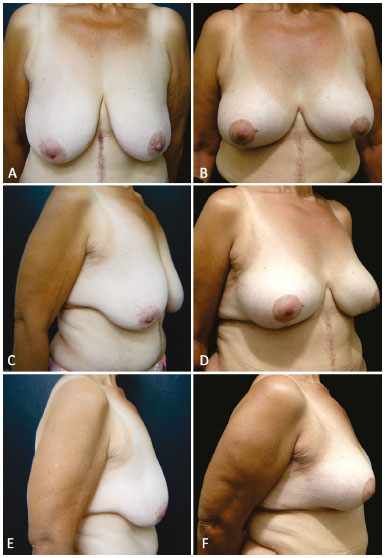
Figure 9. A, B, C, D, E and F: Preoperative and 4-year postoperative aspect with the use of a silicone sheet.
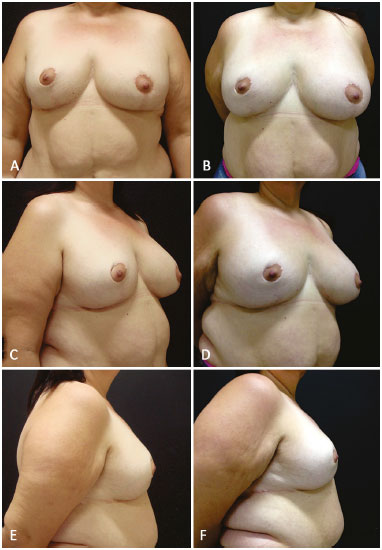
Figure 10. A, B, C, D, E and F: Postoperative aspect at 1 year and 3 years with the patient gaining 12 kg, without modification of form and flaccidity.
No intraoperative complications were observed. One of the patients had hypertension and seroma on the right breast after 2 weeks despite vacuum drainage for 4 days. Drainage was performed again, this time achieving complete resolution without adverse effect on the final result. The patient shown in Figure 10 gained 12 kg after breast surgery, but the shape of her breasts were maintained and naturally increased in volume.
DISCUSSION
The polypropylene-poliglecaprone mesh, being less elastic, seems to provide greater resistance to residual future ptosis and is used routinely in general surgery. The mesh or a silicone sheet can be used for this purpose and provides good results.
Observation of the 9 initial cases only demonstrated technical feasibility. Another 24 patients will be operated on according to the protocol of the ethics committee of the Faculty of Medicine of São José do Rio Preto, and will be observed every 3 months for 2 years for immediate postoperative and late surgical complications by using mammography, ultrasonography, and magnetic resonance imaging, as well as for preoperative and postoperative breast appearance and areola sensitivity.
The resection of the vertical skin can be extended after the modeling and application of the mesh. The upper detachment up to the HHBL facilitates the descent toward the submammary groove and the transverse tractions with best adjustment of the content-continent relationship.
At the confluence of the inverted T, the traction of the skin should not be intense in order to reduce the possibility of suture dehiscence and exposure of the mesh.
The position of the areola at its new place via a medial or lateral pedicle, or a free nipple-areola graft, and the difficulties inherent in its elevation must be assessed at the time of the procedure. Free grafting should be the last option but should always be considered. The 9 cases had 2 free grafts and 7 areola pedicles.
Only major weight loss promotes the reduction of elasticity and, consequently, the contractile strength of the skin. Mammoplasty or mastopexy in these patients attain poor medium and long-term results from the point of view of residual ptosis. Weight loss by bariatric surgery is associated with worse prognosis due to proteomic alterations of the skin, thereby requiring additional support.
Being soft tissues with intense flaccidity, breasts are difficult to model with the perfect proportions as described, but these will serve as the guide parameters in modeling the volume and proportions of the cone.
CONCLUSION
Breast augmentation in patients who had undergone bariatric surgery and weight loss requires additional breast support because the structurally altered skin could not support its weight owing to early development of residual ptosis.
COLLABORATIONS
ARB Conception and design of the study, completion of operations and/or experiments, and drafting the manuscript or critical review of its contents.
REFERENCES
1. Kaluf R, Mendes WA, Guimarães Filho W, Araújo BGO, Borges YAV, Teixeira LR. Sistematização e conduta do serviço de cirurgia plástica do hospital geral de Goiânia em mamoplastia pós perda ponderal nos últimos dez anos. Rev Bras Cir Plást. 2013;28(4):544-8.
2. Gallo JRB. Correlações clínicas do perfil proteômico da pele abdominal na obesidade mórbida e após grandes emagrecimentos. [Tese de Doutorado]. São José do Rio Preto: Faculdade de Medicina de São José do Rio Preto; 2014.
3. Bustos RA. Periareolar mammaplasty with silicone supporting lamina. Plast Reconstr Surg. 1992;89(4):646-57.
4. Góes JCS. Periareolar mammaplasty: double skin technique. Rev Soc Bras Cir Plást. 1989;4:55-63.
5. Sampaio Góes JC. Periareolar mammaplasty: double-skin technique with application of mesh support. Clin Plast Surg. 2002;29(3):349-64.
6. Rubin JP, Khachi G. Mastopexy after massive weight loss: dermal suspension and selective auto-augmentation. Clin Plast Surg. 2008;35(1):123-9.
7. Góes JC. Periareolar mammaplasty: double skin technique with application of polyglactine or mixed mesh. Plast Reconstr Surg. 1996;97(5):959-68.
8. Góes JC, Landecker A, Lyra EC, Henríquez LJ, Góes RS, Godoy PM. The application of mesh support in periareolar breast surgery: clinical and mammographic evaluation. Aesthetic Plast Surg. 2004;28(5):268-74.
9. Koo MY, Lee SK, Hur SM, Bae SY, Choi MY, Cho DH, et al. Results from over one year of follow-up for absorbable mesh insertion in partial mastectomy. Yonsei Med J. 2011;52(5):803-8.
10. Cho JS, Shin SH, Park JY, Song YJ, Yi JM, Park MH, et al. Analysis of infections occurring in breast cancer patients after breast conserving surgery using mesh. J Breast Cancer. 2011;14(4):328-32.
11. Lee A, Won Hwang H, Chang J, Lim W, Moon BI. Outcomes of breast conserving surgery with immediate vicryl-mesh insertion: is it safe and effective? Breast J. 2012;18(4):334-8.
12. Cobb WS, Kercher KW, Heniford BT. The argument for lightweight polypropylene mesh in hernia repair. Surg Innov. 2005;12(1):63-9.
13. Deeken CR, Faucher KM, Matthews BD. A review of the composition, characteristics, and effectiveness of barrier mesh prostheses utilized for laparoscopic ventral hernia repair. Surg Endosc. 2012;26(2):566-75.
14. Śmietański M, Śmietańska IA, Modrzejewski A, Simons MP, Aufenacker TJ. Systematic review and meta-analysis on heavy and lightweight polypropylene mesh in Lichtenstein inguinal hernioplasty. Hernia. 2012;16(5):519-28.
15. Patel H, Ostergard DR, Sternschuss G. Polypropylene mesh and the host response. Int Urogynecol J. 2012;23(6):669-79.
16. Medina HS, Ramalho R, Biscotto R, Chveid M. Tela de Prolene - Utilização em Reconstruções de Cabeça e Pescoço. Rev Bras Cir Plást.1997;12(1):7-16.
17. Bozola AR, Longato FM, Bozola AP. Análise geométrica da forma da beleza da mama e da forma de prótese baseado na proporção Phi: aplicação prática. Rev Bras Cir Plást. 2011;26(1):94-103.
18. Pitanguy I. Mammaplastias. Rev Latinoam Cir Plast. 1963;7:139.
19. Bozola AR. Breast reduction with short L scar. Plast Reconstr Surg. 1990;85(5):728-38.
20. Bozola AR. Reduction mammaplasty: preferred Techniques. In: Goldwyn RM. Reduction mammaplasty. Boston: Litlle Brown; 1990. p.407-37.
21. Ribeiro L. The Lozaenghe technique. In: Goldwyn RM. Reduction mammaplasty. Boston: Litlle Brown; 1990.
22. Lima JC. Breast Reduction: New Method and refinaments. In: Transactions of the Seventh International Congress of Plastic Reconstrutive Surgery; 1979 May 25-27; Rio de Janeiro, RJ. p.518-521.
Hospital de Base da Faculdade de Medicina de São José do Rio Preto, São José do Rio Preto, SP, Brazil
Institution: Hospital de Base da Faculdade de Medicina de São José do Rio Preto, SP, Brazil.
Corresponding author:
Antonio Roberto Bozola
Av. Brigadeiro Faria Lima, 5416 - São Pedro
São José do Rio Preto, SP, Brazil Zip Code 15090-000
E-mail: zeze@bozola.com.br
Article received: September 8, 2015.
Article accepted: May 12, 2016.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter