

Original Article - Year 2016 - Volume 31 -
Comparison of anatomic and round implants using periareolar access in primary breast augmentation
Comparação entre implantes anatômicos e redondos por via periareolar em aumentos mamários primários
ABSTRACT
INTRODUCTION: Breast augmentation requires planning with objective and rigorous criteria, which were standardized by the High Five system of Tebbetts. There are a many possible combinations based on access route, implant plane, and type of implant, enabling the best outcome for each patient.
METHOD: Of 100 patients studied, 30 received anatomic implants and 70 received round implants in the retromuscular or subglandular position, with or without round block technique. All cases used periareolar access. Preoperative evaluation was performed according to the High Five system.
RESULTS: The round block technique was used more often with anatomic implants (43%). The subglandular plane was most commonly used (76.6%). Of 30 anatomic implants, 86.7% were placed in the subglandular plane. Of 70 round implants, 71.4% were placed in the subglandular plane. There were 4 cases of grade III and IV capsular contracture, which is more common with the use of round implants. The rate of rotation among anatomic implants was 10%, with 3 cases.
CONCLUSION: There was a low complication rate, in accordance with published data. Periareolar access provided good results in all cases. The patient should be informed about the possibility of rotation with use of anatomic implants.
Keywords: Breast implant; Mammoplasty; Contracture; Round block; Breast.
RESUMO
INTRODUÇÃO: Aumentos mamários exigem planejamento com critérios objetivos e rigorosos, que foram padronizados pelo sistema High Five, de Tebbetts. Existe um grande número de combinações possíveis, entre via de acesso, plano e tipo de implante, o que permite proporcionar o melhor resultado para cada paciente.
MÉTODO: 100 pacientes operadas, 30 com implantes anatômicos e 70 com redondos, por via retromuscular ou subglandular, com a realização de roundblock ou não. Todos os casos foram operados pela via periareolar. A avaliação pré-operatória foi realizada conforme a sistematização High Five.
RESULTADOS: Roundblock foi mais utilizado no grupo de implantes anatômicos, representando 43% da amostra neste caso. O plano subglandular foi o mais utilizado, representando 76,6% da amostra total. Com relação ao implante anatômico, 86,7% dos implantes foram colocados no plano subglandular. Dos anatômicos, 71,4% foram colocados no plano subglandular. Ocorreram quatro casos de contratura capsular graus III e IV, mais comum com o uso de implante redondo. O índice de rotação do implante anatômico foi de 10%, com três casos no total.
CONCLUSÃO: Ocorreu baixo índice de complicações, em conformidade com a incidência da literatura. O acesso periareolar proporcionou bons resultados em todos os casos. O paciente deve ser informado sobre a possibilidade da rotação do implante anatômico.
Palavras-chave: Implante mamário; Mamoplastia; Contratura; Roundblock; Mama.
According to data from the International Society of Aesthetic Plastic Surgery (ISAPS), breast augmentation was the second most common intervention in Brazil in 2015 after liposuction, representing approximately 13% of all surgical procedures performed; breast augmentation continues to be one of the most requested plastic surgeries by Brazilian women1.
This high incidence is also observed in worldwide statistics. The procedure has been performed for 40 years, since the invention of silicone breast implants, and continues to gain popularity among patients who seek to enhance the size and shape of the breasts2.
The use of highly cohesive gel represented a major advance in the quality of breast implants. Both the round and anatomic format are available, with different volumes, projections, and texturizations. Polyurethane coated implants are also available. This huge range of implant types allows individualized results appropriate to each patient, although even the most experienced plastic surgeon may be uncertain of the best choice2.
The planning of breast augmentation with silicone implants involves important variables and options that determine the course of the patient in the short, medium, and long term. Preoperative decisions as to the type of implant, access route, and positioning above or below the pectoralis major should be individualized to achieve the best outcome for each patient3.
Taking into account the 3 variables outlined above, more than 50 combinations are possible, demonstrating how complicated breast augmentation can be4.
Although breast augmentation is historically characterized as a surgical procedure that places a breast implant within a space, it is known that there are more factors involved than just the surgical procedure. In fact, the non-surgical aspects of breast augmentation are probably more important than the procedure itself4.
Many authors have considered these variables, based on their clinical experience, and have attempted to systematize algorithms for the choice of implants and evaluation of patients. For example, Tebbetts and Adams3 developed the Tissue Characteristics of the Breast (T), Envelope (E), Parenchyma (P), Implant (I) and Dynamics (D) (TEPID)4 system. Its successor, the High Five system, transforms subjective into objective variables using precise measurements. This systematic approach is aimed at reducing a rate of postoperative interventions that has remained between 15 and 24% at 2 to 3 years, according to the largest study available4.
OBJECTIVE
The objective of this study is to compare the incidence of complications associated with round and anatomic implants using periareolar access in primary breast augmentation, based on the objective High Five criteria of Tebbetts and Adams3 for preoperative planning.
METHODS
The study followed the principles of the Declaration of Helsinki and all patients signed a Free and Informed Consent Form. Patients who underwent primary breast augmentation using the periareolar technique in a private clinic and the Plastic Surgery service at the Hospital dos Defeitos da Face, in São Paulo, SP, were evaluated by the author from 2008 to 2013. The patients were divided into 2 groups: 30 patients received anatomic implants and 70 received round implants. The High Five system recommended by Tebbetts and Adams3, which considers objective criteria, was used for procedure planning.
The variables evaluated, in order of priority, were: coverage of soft tissue and location of the surgical pocket; volume of the implant; type of implant, size and dimensions; and the ideal location of the inframammary fold.
All cases in the study underwent surgery based on these 4 factors; although not included in the initial assessment, the access route was defined as periareolar in all cases.
The preoperative evaluation required on average one hour, and the emphasis was on patient education4 regarding the procedure.
Four primary measurements were performed.
1. The thickness of clamped skin at the upper pole (Figure 1), which must be greater than or equal to 3 cm for subglandular or subfascial implants.
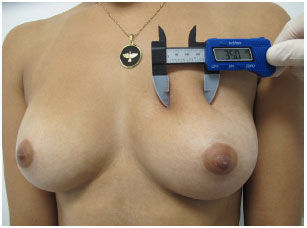
Figure 1. Measurement of skin fold at upper pole.
Clamping of the lower pole evaluates the thickness along the mammary groove; if this value is less than 5 mm, one should consider avoiding division of the lower origin of the pectoralis major (dual plane type 1)5; the implant should be placed in the retromuscular space to maximize covering of the implant5-10.
2. Width of the breast base (BM): This is the most important measurement in choosing the volume of the implant. It is measured from the parasternal edge at the origin of the pectoralis major, transversely to the more lateral portion of the breast (Figure 2); use of a caliper allows linear measurement without distortion5-10.

Figure 2. Measurement of the breast base.
3. Skin elasticity (EP): this is the second most important measurement in choosing the volume of the implant. This is performed by clamping the medial border of the areola and pulling it anteriorly to its maximum elasticity and measuring the anteroposterior extent of stretch with a caliper. (Figure 3). A measurement of 2 to 3 cm is considered normal, less than 2 cm is fair, and 3 to 4 cm is considered flaccid. Measurements greater than 4 cm are considered inappropriate for breast augmentation without an additional procedure for skin removal5-10.
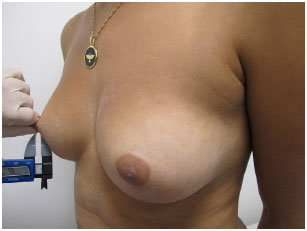
Figure 3. Measurement of skin elasticity.
4. The nipple-inframammary fold distance (M-SIM) is measured under tension with a tape measure, from the mid-point of the nipple to the groove (Figure 4). This measurement was performed in all cases, and the new position of the inframammary fold was set according to the dimensions of the implant of choice.
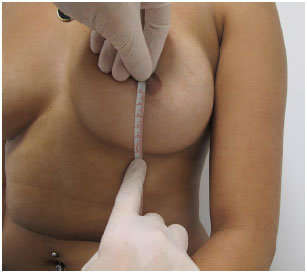
Figure 4. Measurement of the nipple- inframammary fold distance.
The choice of implant shape was based on the protocol described by Baptista et al.7, which divides the breast into vertical and horizontal axes; the relationship between these axes determines the choice of a round implant when they are proportionate, and an oval implant when the vertical dimension is greater than the horizontal dimension (Figures 5 and 6).

Figure 5. Vertical axis of the breast.

Figure 6. Measurement of the horizontal axis of the breast.
The vertical axis is the distance from the inframammary groove to the apex of the axillary fossa. The horizontal axis is defined by the distance from the anterior axillary line to 2 cm from the midsternal line. Round implants were chosen for patients with a round breast base and anatomic implants for those with an oval breast base.
All patients signed a Free and Informed Consent Form, as recommended by the Brazilian Society of Plastic Surgery (SBPC).
Antisepsis with chlorhexidine gluconate in soap is routinely performed in the surgical field, followed by antisepsis with chlorhexidine alcohol solution.
A periareolar incision was performed in cases of breast augmentation in which measured skin elasticity was less than or equal to 4 cm and the breast had a round base. A periareolar incision was also performed in cases in which measured skin elasticity was greater than 4 cm, using the round block technique, as described by Benelli8, with nylon 2.0 in 2 opposing planes to maintain the size of the areola. The limit of periareolar skin resection is 6 cm, exceeded only in those cases in which the areola extends beyond these dimensions. The resulting size of the areola was established at 4 cm.
The irrigation of the implant pocket and washing of surgical gloves and implants is performed as recommended by Adams et al.9, using available antibiotics.
The protocol adopted for washing uses a combination of cefazolin 1 g and garamycin 80 mg diluted in 250 ml of physiological saline.
After the pocket is opened, gauze moistened with saline solution at 2-8°C is applied for 10 min using manual compression. The compress is then removed and need for additional hemostasis is evaluated.
Repeat antisepsis is performed around the incision using chlorhexidine alcohol. The surgical gloves are changed and washed with an antibiotic solution.
Plastic film insulation is placed on the skin as a contact barrier, preventing contact of the implant with the skin and nipple; Steri-Drape was routinely used (Figure 7).

Figure 7. Skin barrier for inclusion of the implant.
The author has routinely prescribed oral montelukast 10 mg for 3 months together with vitamin E at a daily dose of 800 IU, as a protocol for the prevention of capsular contracture.
Manual lymphatic drainage commences on the fifth postoperative day, and is performed 2 to 3 times per week, for a month on average.
The use of a compression bra is started in the immediate postoperative period and maintained for 30 days.
Descriptive data were initially analyzed. Absolute and relative frequencies were calculated for categorical variables, and summary measures (mean, median, minimum, maximum, and standard deviation [SD]) were used for numeric variables.
Associations between 2 categorical variables were assessed using the chi-square test, or Fisher's exact test in cases with small samples. The comparison of means between 2 groups and more than 2 groups was performed using Student's t-test for independent samples and analysis of variance (ANOVA), respectively. An assumption of these 2 tests is normality of the data, which was verified with the Kolmogorov-Smirnov test.
For all statistical tests, a significance level of 5% was used.
Statistical analyses were performed using SPSS 20.0 statistical software.
RESULTS
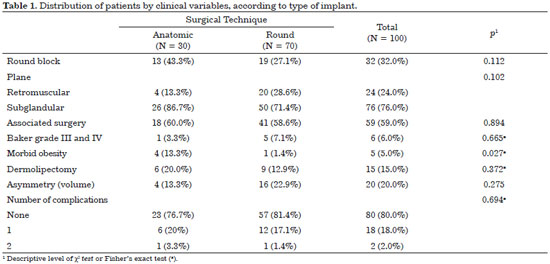
Data from 100 women were analyzed; 30 received anatomic implants and 70 received round implants. The mean age was 31.8 years (SD = 9.1 years), with a minimum age of 18 years and maximum of 65 years (Figures 8 to 18).
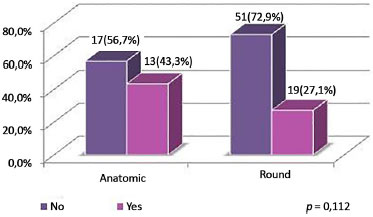
Figure 8. Distribution of patients by round block technique, according to type of implant.
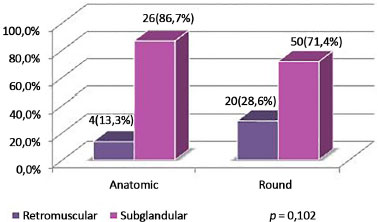
Figure 9. Distribution of patients by implant plane, according to type of implant.
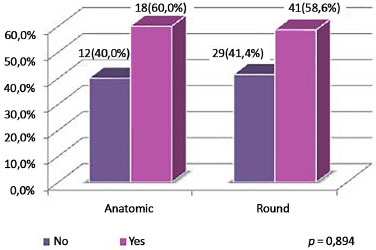
Figure 10. Distribution of patients by associated surgery, according to type of implant.
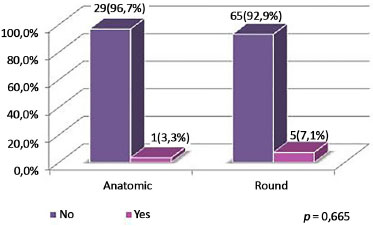
Figure 11. Distribution of patients by Baker grade III and IV capsular contracture, according to type of implant.
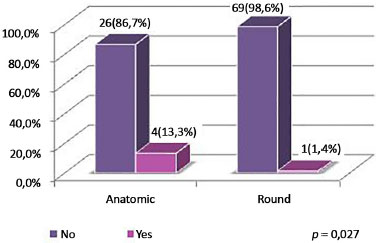
Figure 12. Distribution of patients by morbid obesity according to type of implant.
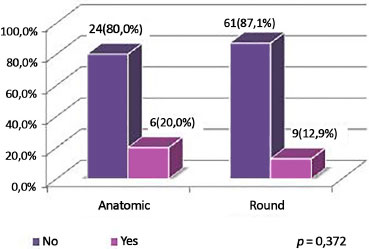
Figure 13. Distribution of patients with associated dermolipectomy, according to type of implant.
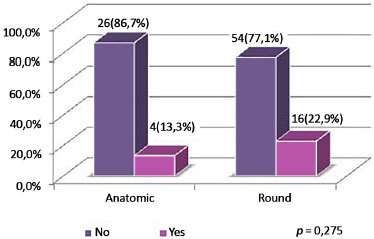
Figure 14. Distribution of patients by asymmetry (difference in the volume of the right and left implant), according to type of implant.
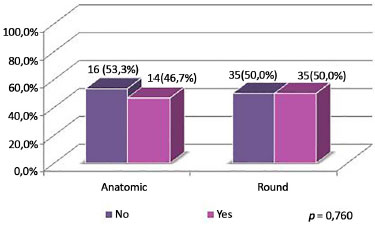
Figure 15. Distribution of patients by associated liposuction, according to type of implant.
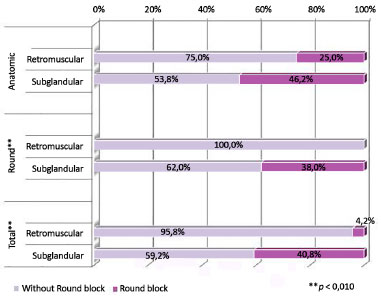
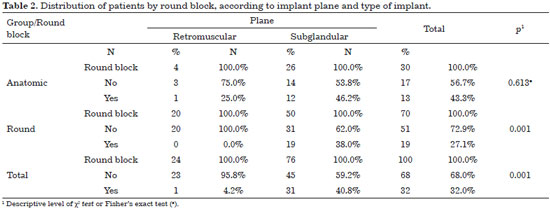
Figure 16. Distribution of patients by round block technique, according to implant plane and type of implant.
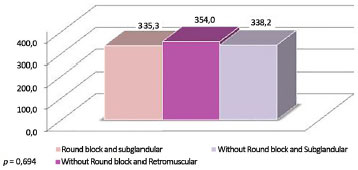
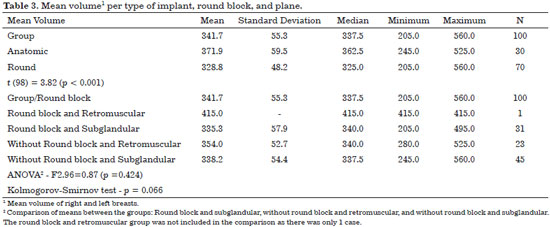
Figure 17. Mean volume per type of implant, round block, and plane.
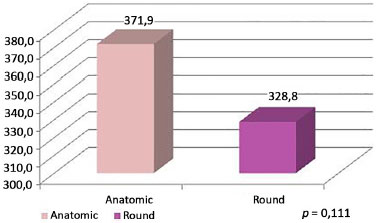
Figure 18. Mean volume per type of implant, round block, and plane.
The group receiving anatomic implants had a mean age of 34.1 years (SD = 9.7 years) and the group receiving round implants had a mean age of 30.9 years (SD = 8.8 years), with no statistical difference between groups (p = 0.111).
Complications only occurred in the anatomic implant group. Rotation of the implant occurred in 3 patients, accounting for 10% of the sample (95% confidence interval [CI] = 2.1%-26.5%).
Table 1 and Figures 1 and 8 show an association between type of implant used and morbid obesity (p = 0.027). Thus, there was a greater percentage of morbid obesity (13.3%) in patients undergoing surgery with anatomic implants compared to patients undergoing surgery with round implants (1.4%). The other variables showed no associations with the type of implant used.
Due to sagging skin, round block technique was used proportionally more frequent in the anatomic implants, representing 43% of the sample, but was only used in 27.1% of the round implants. Non-completion of round block predominated in the group receiving round implants.
The subglandular plane was the most used, representing 76.6% of the total sample. Of 30 anatomic implants, 86.7% were placed in the subglandular plane. Of 70 round implants, 71.4% were placed in the subglandular plane.
The incidence of associated surgeries per type of implant was similar, at around 60% in the 2 samples; liposuction was the most common procedure, with an overall incidence of 34%. The use of implants of different volumes for symmetry was more common with round implants.
Table 2 and Figure 9 show an association between the dissection plane and round block technique in all patients (p = 0.001) and the group with round implants (p = 0.001). Thus, in the group of patients with round implants and a retromuscular plane, there were no cases using round block technique, while in patients who underwent subglandular placement, round block technique was used in 38.0%.
Furthermore, patients who underwent subglandular placement also experienced greater use of round block technique (40.8%), compared to patients who underwent retromuscular placement (4.2%).
Table 3 and Figures 10 and 11 show that the group of patients who received anatomic implants received a greater mean implant volume than the group of patients who received round implants (p < 0.001). In the round block and subglandular groups, there were no statistical differences in mean volume (p = 0.424) between those without round block and retromuscular plane and those without round block and subglandular plane.
DISCUSSION
In plastic surgery, many procedures rely on the prior experience of the surgeon. Any attempt to perform a procedure on a more objective basis is desirable. Citing an important example, Professor Ivo Pitanguy systematized reduction mammoplasty, thus allowing reproduction of his technique and facilitating the teaching of plastic surgery to residents.
Patients present a wide variety of features in the skin envelope, parenchyma, and adjacent tissues, and the complication rate increases when these characteristics are not respected6.
Accordingly, Tebbetts4 developed the TEPID system of objective evaluation, which took into account the tissue of the patient as the most important factor in planning the implant.
The High Five system, also developed by Tebbetts4, was the successor to the TEPID system, and presented a more comprehensive and pragmatic approach to preoperative planning for breast implantation. This objective system was adopted by the author for routine use due to the predictability of results and a lower rate of reoperation8.
Tebbetts4 stated in the original article that the goal is to prioritize the well-being of the tissues in the long term and thus decrease reoperation rates; in a series of more than 2,000 cases, the reoperation rate was 3%, but decreased to 0.2% by changing the size of the implant.
Adams10, in a series of 300 cases, reported a 2.8% rate of reoperation. The author of this study encountered only 2 examples among 100 operated cases. The first case required an exchange of bilateral implants due to grade IV Baker capsular contracture in the left breast and grade III contracture in the right breast, 6 months after initial surgery.
The second case presented with grade IV capsular contracture in the left breast, and was managed with an exchange of implant and modification of the retromuscular plane. In this specific case, liposuction of the lateral region of the breast was performed, suggesting the possible existence of a connection between a probable seroma and occurrence of capsular contracture. Thus, the surgical revision rate was 2%, lower than the 4.2% described by Jewell and Jewell11 and the 12.5% reported by Bengtson et al.12
In no case was an exchange of breast implant required due to asymmetry. Only one case presented with clinically detectable asymmetry in the late postoperative period; this was preexisting, but, was more pronounced in the preoperative period. The patient was satisfied with the result, although the author offered surgical correction.
In the series studied, 24% of the implants were submuscular and 76% were subglandular. When choosing the location of the implant, the plastic surgeon should take into account technical criteria established in the medical literature, and try to apply these to the profile of the patient7.
Published studies recommend both planes, with advantages and disadvantages; thus, it is important to master both techniques to meet the needs of each patient13.
The subglandular plane is theoretically the best for placement of the implant because it respects the original anatomy of the breast, even though it is associated with a higher rate of complications than the submuscular plane14.
According to McCarthy et al.15, the placement of the implant under the pectoralis major muscle allows better visualization and a greater quantity of mammary parenchyma available for imaging, when compared to the location under the gland, regardless of the size of the breast and type of implant. Moreover, a lower incidence of capsular contracture has been reported with the use of this approach9,16, consistent with the results found by the author. Tebbetts6 suggested the placement of the implant in a double plane, with greater or lesser release of the greater pectoral muscle, according to the needs of each case.
As an alternative, Graf et al.17, described the placement of the implant in the subfascial plane, with the reported benefit of better coverage of the upper pole of the breast, and without excessive manipulation of the pectoral muscles; good results were confirmed by Tebbetts4 and the series was reported by Espírito Santo18.
In the case of capsular contracture with an implant in the subglandular and subfascial plane, patients with visible and palpable implants or thin mammary parenchyma present a challenging reconstruction. In such cases, a secondary mastoplasty with exchange of the subglandular for the submuscular plane, associated with capsulotomy, is perhaps the only alternative14-17.
The inframammary incision allows direct and ample access for implant placement, which may be subglandular, submuscular, subfascial, or in a double plane. The resulting scar measures 4 to 5 cm, and it should mostly be positioned on the lateral portion of the breast midline. This is most commonly used by plastic surgeons in Brazil and some North American surgeons9.
Periareolar access was described in 1972 and is widely used today14. The incision is planned in the lower portion of the areola and allows easy adjustment of the inframammary fold with a discreet scar. Augmentation mastoplasty may not be the only surgery in the patient's life; it may be necessary to exchange the implants at some point, and a mastopexy may be required.
Hence, the areola must be taken into consideration; for aesthetic quality and to minimize scars on the breast, the author regards periareolar access as more suitable, both as a primary approach and for future approaches inherent to the procedure.
Some disadvantages are the potential risk of contamination by a lesion of the lactiferous ducts, change in the sensitivity of the nipple, and a difficult dissection in patients with an areola less than 3 cm in diameter. This approach is indicated for patients with tuberous breasts17,19. In this series, no patient developed infection or difficulty in lactation.
Round implants provide more predictable results and have the relative advantage of clinically inapparent rotation. This is not the case with the anatomic implant, in which even slight rotation becomes clinically apparent14.
Some factors can prevent the rotation of the anatomic implant. The first is the texture of the implant, which creates friction, and a so-called Velcro effect19. The second is the adhesion of the implant to the surgical pocket, which is influenced by extensive dissection, an immature capsule, or an unstable implant location 18, as when a double capsule is formed or when there is an abnormal amount of fluid in the pocket acting as a lubricant. Adams10 stated that a tightly dissected pocket was a preventive factor against rotation of an anatomic implant, and considered this to be a static structure14.
The natural tendency of a sphere is to preserve its form, with maximum volume and minimum surface area; as a round implant is similar to a sphere, the pocket tends to adhere better to the implant when contraction occurs, with less dynamic alteration. With the round implant, a more spherical capsule forms when normal scar retraction occurs, which differs considerably from the shape of the anatomic implant14-19.
It is well known that anatomic implants have a high risk of rotation, which occurred in 10% (3 cases) in this series, motivating the author to adopt new strategies such as the use of conical implants coated with polyurethane, in a series that will be described in the future. Adams10 encountered anatomic implant rotation in 2.7% of 37 cases; this was managed clinically, without the need for reoperation. Jewell and Jewell11 reported an incidence of 0.8% in 119 patients who underwent surgery. Bengtson et al.12 observed a 2.6% rate of rotations in a multicenter study with a follow-up of 3 years.
In patients who previously underwent surgery to treat morbid obesity, the use of anatomic implants was more common, with 13.3% of cases in this group, against 1.4% who received round implants. These patients had greater skin elasticity, and anatomic implants offered better volumetric distribution with adequate compensation of the surgical pocket. For the same reason, the use of round block technique was more common in the group receiving anatomic implants.
In the group that received round implants, there was a lower incidence of skin laxity, which justifies the use of this type of implant more commonly in the retromuscular plane.
There were no cases of hematoma among the 100 cases that underwent surgery by the author, which can be attributed to rigorous hemostasis, use of cold saline compresses, and external compression for 10 min. This incidence is consistent with that found by Adams10 who also observed no cases of hematoma in 37 patients who received anatomic implants.
Although some patients had a high body mass index, rippling was not observed, demonstrating that surgical planning according to criteria established by Tebbetts4 is effective. In 119 cases, Jewell and Jewell11 found a 7.6% incidence of rippling, and Adams10 reported 16%, 15 of which occurred with textured round implants and only one with an anatomic implant.
Significant seroma formation and clinical sequelae were not detected in any patients. Late seroma was also not observed.
There were no cases of infection in this series, which can be attributed to a protocol using antiseptic treatment of gloves, implant, and the surgical pocket, as recommended by Adams10, who found only 3 cases of infection in a series of 229. It is believed that the routine use of skin contact barriers also contributed significantly to the prevention of infection.
Capsular contracture occurred in 1 patient in the group with anatomic implants (3.3%) and 5 (7.1%) in the group with round implants. Clinical and surgical procedures were adopted for prevention, and the incidence of grade III contracture was similar to the 2.5% reported by Jewell and Jewell11, with no grade IV contractures; this was slightly higher than the 0.58% described by Adams10.
There was no evidence of increased risk of false negative imaging examinations for detection of malignancy. However, when the implant is placed under the pectoralis major, better visualization is possible and a greater amount of breast parenchyma may be examined18-21.
CONCLUSION
The use of objective criteria for preoperative planning as recommended by Tebbetts19 resulted in a low rate of reoperation and complications. Periareolar access provided satisfactory results in all cases, with discreet scars using both types of implants. In addition, this access results in a minimal scars on the breast, since the areola may be affected in future surgeries such as mastopexy or exchange of implants. The patient should be informed about the possibility of rotation of the anatomic implant and should actively participate in implant selection.
COLLABORATIONS
MCSG Completion of surgeries and/or procedures and conception and design of the study.
CSS Writing the manuscript or critical review of its contents.
JA Statistical analysis.
DTG Analysis and/or interpretation of data.
REFERENCES
1. International Society of Aesthetic Plastic Surgery. ISAPS Global Statistics [citado 2016 Set 15]. Disponível em: http://www.isaps.org/news/isaps-global-statistics
2. Graf R, Auersvald A, Biggs T. Mamoplastias de aumento: problemas e soluções. In: Mélega JM, Baroudi R, eds. Cirurgia plástica - fundamentos e arte: cirurgia estética. São Paulo: Medsi; 2003. p.591-607.
3. Tebbetts JB, Adams WP. Five critical decisions in breast augmentation using five measurements in 5 minutes: the high five decision support process. Plast Reconstr Surg. 2006;118(7 Suppl):35S-45S.
4. Tebbetts JB. A system for breast implant selection based on patient tissue characteristics and implant-soft tissue dynamics. Plast Reconstr Surg. 2002;109(4):1396-409.
5. Adams WP Jr. Mamoplastia de aumento de plano duplo. In: Adams WP, ed. Atlas de Cirurgia Plástica. Porto Alegre: McGraw Hill; 2011.
6. Tebbetts JB. Dual plane breast augmentation: optimizing implant-soft-tissue relationships in a wide range of breast types. Plast Reconstr Surg. 2001;107(5):1255-72.
7. Baptista RR, Salles AG, Remigio AFN, Cruz DP, Ferreira MC. Avaliação dos resultados estéticos após mamoplastias de aumento com o uso de implante redondo vs. Anatômico. Rev Bras Cir Plást. 2010;25(Supl):1-102.
8. Benelli L. A new periareolar mammaplasty: The "round block" technique. Aesth Plasti Surg 1990;14(1):93-100.
9. Adams WP Jr, Rios JL, Smith SJ. Enhancing patient outcomes in aesthetic and reconstructive breast surgery using triple antibiotic breast irrigation: six-year prospective clinical study. Plast Reconstr Surg. 2006;117(1):30-6.
10. Adams WP Jr. The process of breast augmentation: four sequential steps for optimizing outcomes for patients. Plast Reconstr Surg. 2008;122(6):1892-900.
11. Jewell ML, Jewell JL. A comparison of outcomes involving highly cohesive, form-stable breast implants from two manufacturers in patients undergoing primary breast augmentation. Aesth Surg J. 2010;30(1):51-65.
12. Bengtson BP, Van Natta BW, Murphy DK, Slicton A, Maxwell GP; Style 410 U.S. Core Clinical Study Group. Style 410 highly cohesive silicone breast implant core study results at 3 years. Plast Reconstr Surg. 2007;120(7 Suppl 1):40S-8S.
13. Zeitoune GC. Subpeitoral ou subglandular: qual é a melhor localização do implante para pacientes com hipomastia. Rev Bras Cir Plást. 2012;27(3):428-34.
14. Neligan P, ed. Plastic Surgery. Volume Five: Breats. Toronto: Elsevier; 2013. p.13-37.
15. McCarthy CM, Pusic AL, Disa JJ, Cordeiro PG, Cody HS 3rd, Mehrara B. Breast cancer in the previously augmented breast. Plast Reconstr Surg. 2007;119(1):49-58.
16. Spear SL, Bulan EJ, Venturi ML. Breast augmentation. Plast Reconstr Surg. 2004;114(5):73E-81E.
17. Graf RM, Bernardes A, Rippel R, Araujo LR, Damasio RC, Auersvald A. Subfascial breast implant: a new procedure. Plast Reconstr Surg. 2003;111(2):904-8.
18. Espírito Santo PRQ. Mastoplastia de aumento via axilar: avaliação da técnica subfascial. Rev Bras Cir Plást. 2010;25(4):663-7.
19. Tebbetts JB. Does fascia provide additional, meaningful coverage over a breast implant? Plast Reconstr Surg. 2004;113(2):777-9.
20. Handel N. Secondary mastopexy in the augmented patient: a recipe for disaster. Plast Reconstr Surg. 2006;118(7 Suppl):152S-63S.
21. Embrey M, Adams EE, Cunningham B, Peters W, Young VL, Carlo GL. A review of the literature on the etiology of capsular contracture and a pilot study to determine the outcome of capsular contracture interventions. Aesthetic Plast Surg. 1999;23(3):197-206.
1. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
2. Hospital dos Defeitos da Face, Cruz Vermelha Brasileira, São Paulo, SP, Brazil
Institution: Hospital dos Defeitos da Face, Cruz Vermelha Brasileira, São Paulo, SP, Brazil.
Corresponding author:
Maria Claudia Sanchez Giometti
Rua Juquis, 31, ap 166 - Moema
São Paulo, SP, Brazil Zip Code 04081-010
E-mail: mclaudiagiom@hotmail.com
Article received: July 28, 2014.
Article accepted: November 12, 2014.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter