

Original Article - Year 2016 - Volume 31 -
Standardization of surgical treatment of acute electrical trauma
Padronização do tratamento cirúrgico do trauma elétrico na fase aguda
ABSTRACT
INTRODUCTION: Electrical burns are responsible for 5% to 15% of cases of burn accidents. The majority is associated with workplace accidents, in which high-voltage injuries (>1,000 V) predominate in male patients. The mortality rates vary from 2% to 15% in different burn centers. The objective is to review the standardization of surgical steps in the acute phase of debridement (the first 15 days) by comparison of creatine phosphokinase levels, intravenous hydration, and photographs to implement routine surgical stages.
METHODS: This was a quantitative, prospective study performed in a public hospital in the city of Fortaleza, Brazil, between July 2013 and December 2015. The population was composed of young adults between 15 and 50 years, of both sexes, who experienced electrical burns, with third-degree injuries and muscle involvement.
RESULTS: Of the 15 patients in the study, 9 (60%) patients underwent 13 surgical amputation procedures and 6 (40%) patients did not undergo amputation. One patient underwent three amputation procedures in the same limb (toe, foot, and thigh) and another patient underwent two amputations in the upper limbs.
CONCLUSION: Treatment in the acute phase of electrical shock must include immediate and adequate intravenous fluid replacement, along with surgical procedures of debridement and amputations, as early as possible, in steps with intervals of 48 to 72 hours.
Keywords: Electrical burns; Electrical shock; Debridement; Hydration; Amputation.
RESUMO
INTRODUÇÃO: As queimaduras elétricas correspondem de 5 a 15% dos casos de acidentes com queimaduras. A maioria está associada a acidentes do trabalho, nos quais predominam as lesões com alta voltagem (acima de 1.000 Volts), em pacientes do sexo masculino. As taxas de mortalidade variam de 2 a 15%, nos mais diversos centros de queimados. O objetivo é revisar padronização das etapas cirúrgicas na fase aguda de desbridamento (primeiros 15 dias) pela comparação de dosagem de creatofosfoquinase, hidratação venosa e fotografias para a aplicação de uma rotina de etapas cirúrgicas.
MÉTODOS: Trata-se de um estudo quantitativo, prospectivo, realizado em um hospital público da cidade de Fortaleza, CE, entre julho de 2013 a dezembro de 2015. A população foi composta por adultos jovens, entre 15 e 50 anos, de ambos os sexos, vítimas de queimaduras por choque elétrico, com lesão de terceiro grau, no mínimo muscular.
RESULTADOS: Foram realizados 12 procedimentos cirúrgicos de amputações nos 15 pacientes do estudo (60%). Seis pacientes não sofreram amputação (40%). Um paciente sofreu três procedimentos de amputação no mesmo membro (pododáctilo, pé e coxa esquerdos) e outro, duas amputações em membros superiores distintos.
CONCLUSÃO: O tratamento na fase aguda do choque elétrico deve incluir uma imediata e adequada reposição líquida venosa, associada com procedimentos cirúrgicos de desbridamentos e de amputações, o mais precoce possível, em etapas com intervalos de 48 a 72 horas.
Palavras-chave: Queimaduras elétricas; Choque elétrico; Desbridamento; Hidratação; Amputação.
Electrical burns correspond to 5% to 15% of burn accidents. The majority is associated with accidents at the workplace, in which high-voltage injuries (>1,000 V) are more predominant in male patients. Victims of these accidents display high morbidity and mortality, with high incidence of amputations and neurological disorders, reduced quality of life, and low rate of return to former work, and 5% to 32% do not return to any kind of work. The mortality rates vary from 2% to 15% in different burn centers1,2.
An electrical shock on the extremities has a devastating effect, compromising deeper structures and causing vascular thrombosis, which lead to progressive necrosis in structures that were not initially compromised3. Severe muscle injury, which affects the majority of patients, causing breakdown or destruction of striated muscle, is known as rhabdomyolysis4.
High levels of creatine phosphokinase (CPK >2,500 IU) indicate serious muscle damage, requiring urgent surgical debridement or amputation3. These surgical procedures, in addition to high volumes of intravenous hydration, should be used until the CPK level is at < 400 IU.
Authors differ in terms of surgical treatment during the critical period (i.e., the acute phase; first 15 days), with others choosing a more aggressive surgical treatment, while others performing the treatment in several stages throughout the critical period. Some authors, such as Baxter5 and Skoog6, attribute the continuous tissue damage and progressive muscle necrosis to damage in the vessels walls, thus preferring to perform debridement in serial stages. Others, like Hunt et al., Zelt et al., Silveberg et al., and Buchanan et al., confirmed through experimental studies that there is no tendency for progressive tissue necrosis, corroborating the views of those who advocate early aggressive surgical treatment of the affected areas. However, there is no standardization of these surgical steps correlating the voltage, tissue damage, and surgical planning during this critical initial period7-12.
In the acute phase of electrical burns, the standard surgical procedure is surgical debridement, which is done to remove devitalized tissues, or amputations. These procedures are carried out routinely in the Burn Treatment Center (CTQ) of the Dr. José Frota Institute (IJF); however, there is no standard in terms of appropriate time to initiate surgeries or the intervals between these procedures.
In most cases, debridement in the acute phase, in the public health network, extends for more than 15 days and may take up to a month or more, increasing the rates of morbidity and mortality. In addition, the intervals of surgeries take place approximately a week or more, maintaining high levels of CPK, thus increasing the possibility of renal failure.
OBJECTIVE
This study aimed to review the standardization of surgical steps in the acute phase of debridement through laboratory assessment (CPK), intravenous hydration, and photographs to establish a new routine of surgical steps, in order to develop a suitable treatment.
METHODS
This quantitative, prospective study was performed in IJF, a public hospital in the city of Fortaleza, Brazil, from July 2013 to December of 2015, in which each patient was attended exclusively, since the acute phase demands surgical steps with intervals of 48 to 72 hours.
The Burn Treatment Center was inaugurated in November 1993 and has a physical area of 1,400 m2 and capacity for 28 beds. The service has its own surgery center with two operating rooms and post-anesthesia recovery room with two beds. The clinic is attached to the CTQ and has two offices, balneotherapy room, dressing room, bathroom, and a reception area with a capacity for 15 seated patients.
The study population initially comprised 16 young adults between 15 and 50 years, of both sexes, who experienced electrical burns, with third-degree injuries and muscle involvement, and were hospitalized at the CTQ in a public reference hospital in the city of Fortaleza. One patient was eventually excluded from the study because of absence of muscle injury during the initial period of hospitalization. Owing to the low incidence of electrical burns (5% to 12% of total accidents), the number of patients is relevant to the study.
Patients with electrical shock, with areas of third-degree burn and muscle breakdown, burned surface area (BSA) of 3% to 25%, age between 15 and 50 years old, and signed informed consent form were included in the study. The exclusion criteria in this study were burns less than third degree or without muscle damage, age <15 years or >50 years, BSA <3% and >25%, alcohol dependence, illicit drug use, or psychiatric disorders.
Data collection was carried out by monitoring the patients during hospitalization, along with photos in all phases. A semi-structured interview about the accident and the epidemiological profile was conducted. On hospitalization, in the acute phase, laboratory tests were performed, including the assessment of CPK levels, and repeated every 48 to 72 hours before surgery.
During the hospitalization period, the patients' need for surgeries was analyzed, which was standardized between 48 and 72 hours, using a form with a description of the surgical procedures. The photographs were standardized at initial presentation and at pre- and immediate post-operative periods, with a Sony Cyber-Shot DSC-HX300 digital camera.
All patients received intravenous fluid replacement at admission, using the Parkland formula (4 mL/kg/BSA), and diuresis time control (via urinary catheter) to maintain a CPK levels <1,000 IU and light-colored urine. Diuresis was maintained at 100 mL/h during the period of intravenous hydration.
The collected data were analyzed with Microsoft Excel 2010 and the Statistical Package for Social Sciences (SPSS) program, version 17, with description using tables and graphs.
The study was approved by the Research Ethics Committee of the Dr. José Frota Institute Hospital (number 321.464).
RESULTS
Of the 15 patients in the study, there was a considerable predominance of males (N=13), representing 86.6% of the sample. The average age when the patients experienced the electrical burn was 35.07 years, and in the 2 female patients, the accident happened at home.
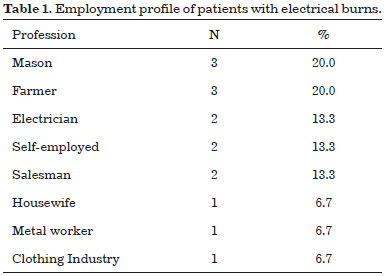
A clear heterogeneous distribution in terms of patient profession was observed (Table 1).
Regarding the origin of these patients, 33.4% were from Fortaleza (capital), whereas 66.6% were from the interior of the state, with the city of Canindé representing 13.3%.
The time between the accident and the care of the patient was 67.3 minutes, and time to hospitalization in a specialized center for burn treatment was 264 minutes, i.e., 4 hours and 24 minutes. These data show an adequate time of attendance, taking into account that the majority of accidents occurred inside the state.
The period of hospitalization of these patients was between 6 and 55 days, with an average of 32 days. There was no death during the acute phase, but two (13.3%) deaths occurred during the reconstruction phase. Loss of consciousness at the time of the electrical shock was reported in 86.7% of the patients.
With regard to BSA, the percentage of second-degree burns ranged from 0% to 35%, with an average of 5.2%. In terms of third-degree burns (object of study), these ranged from 3% to 26%, with an average of 9%. When noting the total BSA, an average of 14.23% was found, ranging from 3.5% to 45%.
The identification of all points of entry and exit from the electrical shock are presented in Table 2.

According to the purpose of the study, these patients were submitted, on average, to 4.8 surgeries in total, ranging from 3 to 8 surgeries, with a mean number of 3.53 surgeries for grafting. In relation to surgical debridement, an average of 2.87 surgeries were performed. The average number of surgical flaps was 0.40, ranging from 0 to 4 surgeries. The average number of fasciotomies was 0.13 per patient, ranging from 0 to 1.
Of the 15 patients in this study, 9 (60%) patients underwent 13 surgical amputations, with an average of 0.86 amputations per patient in our entire sample (Table 3). Six patients did not undergo amputation (40%); patient 4 underwent three amputation procedures in the same limb (toe, foot, and thigh) (Figure 1) and patient 16 underwent two amputations in the upper limbs (right and left) (Figure 2). Six of these amputations were in the upper limb, with one in the finger, four in the forearm, and one on the arm; six were in the lower limb, with three in the toes, one in the foot, and two on the thigh.
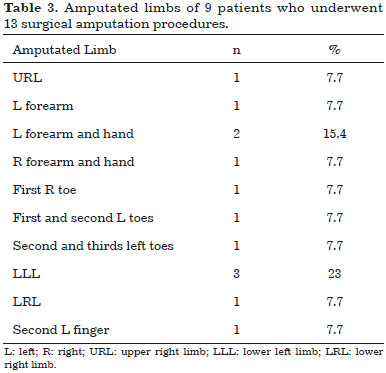

Figure 1. Progression of tissue destruction caused by electrical burns, with three amputation procedures required in the same lower limb of the patient. A: Patient admission showing the injury in the foot and leg; B: Amputation of four toes, 3 days after hospitalization; C: Progressive tissue destruction, 5 days after debridement; D: Amputation of the metatarsals and new cleaning of the limb; E: Destruction of tissues, including muscle, reaching the leg and thigh; F: Amputation at the level of the thigh.

Figure 2. Electrical burn in the right and left hands, with the injury progressing and eventually leading to bilateral amputation. A: Admission, with severe injuries in the R hand; B: Amputation at the level of the R forearm, on the fifth postoperative day after 14 days; C: Admission, with destruction of the tissues of the L hand; D: Amputation at the level of the L forearm, on the seventh postoperative period after 11 days. L: left; R: right.
DISCUSSION
In agreement with the works of Carvalho13 and Greco14, the present study shows a predominance of male victims of electrical burns, representing 86.6% of the sample. Serrano, as quoted by Coiffman3, reported that 99% of affected patients are male. Men have the majority of jobs that entail greater risks of electrical burns (electricians, construction workers, builders), whereas accidents with female patients took place in the home environment.
In this study, the mean age of the patients affected by electrical burns was 35.07 years, but a recent study reported an average of 25 years7. Comparing the two studies shows a gap of 10 years.
When it comes to accidents within the state (66.6%), for the most part, there was an appropriate time interval in primary care and a rapid hospitalization in a specialized burn center, with an average lapse of 4 hours and 24 minutes. In a study by Pereira et al.15, the time for attendance was up to 8 hours in the majority of patients, which indicates that the time for attendance in this study was appropriate. The mean hospital stay was 32 days, which indicates adequate surgical treatment during the acute and reconstruction phases, in agreement with the literature, which states that the earlier the approach, the shorter the duration of the postoperative period will be3,16.
As for the number of amputations, there was no difference between the affected limbs. According to the literature, the prevalence of electrical point of entry is the upper limb and exit in the lower limb, in agreement with this study, where 60% of entries were in the upper limb; 73.3% of the exit occurred in the lower limb3.
No patient died during the acute phase, the most critical period, in which the mortality rate is higher; however, 2 patients died during the reconstruction phase, with almost 30 days of hospitalization3,17. These deaths were probably due to several attempts at surgical reconstruction of the affected limbs using local and distal flaps, where surgical failure due to poor local vascularization, in addition to high metabolic consumption of patient with electrical trauma, was predominant.
It must be highlighted that the surgical team should weigh in the appropriate timing of amputations and avoid getting involved with emotional requests from family members and employers to save the affected limb at any cost; instead, they should objectively evaluate the real conditions of reconstruction with local, distal, or microsurgical flaps, remembering that this is a metabolically expended patient, with few nutritional reserves and that surgical failure, which has a high occurrence rate in these cases, may result in death.
A concept espouses that when the medical team considers performing a tracheostomy on a patient with burns of the upper airways, they should immediately perform the procedure, because by then, it might be too late. Perhaps this same adage can be applied to electrical burns in relation to amputations, evaluating the actual local conditions for reconstruction, the training of staff, and the conditions of the public hospital, in addition to the condition of the patient with metabolic consumption exhausted by electrical trauma.
All patients received appropriate intravenous fluid supply, the keeping urine output at 100 mL/h, without developing renal failure. Intervals of surgery for debridement and amputation (when necessary) remained between 48 and 72 hours, the time we deem necessary to replenish the lost proteins and blood elements and clinically evaluate the patient and assess the affected area.
All patients had progressive tissue necrosis and needed serial debridement, at different surgical times, with intervals between 48 and 72 hours, corroborating the authors who recommended debridement in stages. Patient 4 (Figure 1) underwent ascending amputation in the same affected limb, proving that electrical shock causes progressive tissue damage, since the amputations were performed in previously healthy tissue.
This statement corroborates with those of several authors such as Baxter5 and Skoog6, who argue that tissue damage continues and that progressive muscle necrosis is attributed to damage in the vessel wall.
CONCLUSION
In this study, we conclude that the treatment in the acute phase of electrical burns must include immediate and adequate replacement of intravenous liquid, controlled by the urinary output, along with surgical procedures of debridement and amputations as early as possible, in stages with intervals of 48 to 72 hours, to decrease the morbidity and mortality of patients.
COLLABORATIONS
EMLJ Analysis and/or interpretation of data; statistical analysis; final approval of the manuscript; conception and design of the study; completion of operations and/or experiments; drafting the manuscript or critical review of its contents.
VMML Analysis and/or interpretation of data; statistical analysis; final approval of the manuscript; conception and design of the study; completion of operations and/or experiments; drafting the manuscript or critical review of its contents.
EAP Analysis and/or interpretation of data; statistical analysis; final approval of the manuscript; drafting the manuscript or critical review of its contents.
GEF Analysis and/or interpretation of data; statistical analysis; final approval of the manuscript; completion of operations and/or experiments; drafting the manuscript or critical review of its contents.
REFERENCES
1. Lima Júnior EM, Novaes FN, Piccolo NS, Serra MCVF. Tratado de Queimaduras no Paciente Agudo. 2a ed. São Paulo: Atheneu; 2008.
2. Souza TJA, Bastos PRHO. Perfil sociodemográfico e etiológico de pacientes internados em um centro de referência para tratamento de queimados em Mato Grosso do Sul. Rev Bras Cir Plást. 2015;30(3):391-7.
3. Coiffman F, ed. Texto de Cirugía Plástica, Reconstructiva y Estética. 3a ed. Tomo I. Caracas: Amolca; 2006.
4. Vanholder R, Sever MS, Erek E, Lameire N. Rhabdomyolysis. J Am Soc Nephrol. 2000;11(8):1553-61.
5. Baxter CR. Present concepts in the management of major electrical injury. Surg Clin North Am. 1970;50(6):1401-18.
6. Skoog T. Electrical injuries. J Trauma. 1970;10(10):816-30.
7. Hunt JL, McManus WF, Haney WP, Pruitt BA Jr. Vascular lesions in acute electric injuries. J Trauma. 1974;14(6):461-73.
8. Zelt RC, Daniel RK. Electrical injury. In: Marsh J, ed. Current therapy in Plastic and Reconstructive Surgery. Toronto: Decker; 1989. p. 29-33.
9. Buchanan DL, Erk Y, Spira M. Electrical current arterial injury: a laboratory model. Plast Reconstr Surg. 1983;72(2):199-205.
10. Kuzon WM, Zelt RG, Green HJ, Ballard PA, Pynn BR, Plyley MJ, et al. Skeletal muscle energy metabolism following high voltage electrical injury. Surg Forum. 1986;37:621-3.
11. Zelt RG, Ballard PA, Common AA, Heroux P, Daniel RK. Experimental high voltage electrical burns: role of progressive necrosis. Surg Forum. 1986;37:624-6.
12. Silveberg B, Bannis JC, Verd GD, Acland RD. Microsurgical reconstruction for the electrical and deep thermal injury. Proc Am Burn Assoc. 1985;17:129-34.
13. Carvalho CM, Ferrari Neto O, Faria GEL, Milcheski DA, Gomez DS, Ferreira MC. Uso de retalhos em queimaduras elétricas nos últimos 10 anos. Rev Bras Queimaduras. 2013;12(1):2-5.
14. Greco Júnior JB, Moscozo MVA, Lopes Filho AL, Menezes CMGG, Tavares FMO, Oliveira GM, et al. Tratamento de Pacientes Queimados Internados em Hospital Geral. Rev Bras Cir Plást. 2007;22(4):228-32.
15. Pereira Júnior S, Ely JB, Sakae TM, Nolla A, Mendes FD. Estudo de pacientes vítimas de queimaduras internados no Hospital Nossa Senhora da Conceição em Tubarão - SC. Arq Catarin Med. 2007;36(2):22-7.
16. Bolgiani AN, Serra MCVF. Atualização no tratamento local das queimaduras. Rev Bras Queimaduras. 2010;9(2):38-44.
17. Artz CP, Moncrief JA, Pruitt BA Jr. Burns - a team approach. Philadelphia: WB Saunders; 1979.
1. Centro de Tratamento de Queimados, Hospital Instituto Dr. José Frota, Fortaleza, CE, Brazil
2. Federação LatinoAmericana de Queimaduras, Fortaleza, CE, Brazil
3. Universidade Federal de São Paulo, São Paulo, SP, Brazil
4. Centro Universitário Christus, Fortaleza, CE, Brazil
Institution: Centro de Tratamento de Queimados, Hospital Instituto Dr. José Frota, Fortaleza, CE, Brazil.
Corresponding author:
Edmar Maciel Lima Júnior
Rua Visconde de Mauá, 1650, ap. 801 - Aldeota
Fortaleza, CE, Brazil Zip Code 60.160-251
E-mail: edmarmaciel@gmail.com
Article received: January 24, 2016.
Article accepted: May 27, 2016.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter