

Original Article - Year 2016 - Volume 31 -
High-voltage electrical burns: five-year epidemiological analysis and updated surgical treatment
Queimaduras elétricas por alta voltagem: cinco anos de análise epidemiológica e tratamento cirúrgico atualizado
ABSTRACT
INTRODUCTION: Evaluation of a 5-year epidemiological analysis and updated surgical treatment of high-voltage electrical burns.
METHODS: A descriptive, retrospective cross-sectional study was conducted in the Center of Burn Treatment Dr. Oscar Plaisant, Federal Hospital of Andaraí, Rio de Janeiro, Brazil, from January 2009 to December 2014. A form was applied to the medical records of 38 patients included in the study in order to assess the defined variables.
RESULTS: In total, 38 patients with high-voltage burns were evaluated, 95% of whom were men aged between 21 and 42 years. The most frequent place of occurrence was the workplace in 55.3% of cases. The percentage of burned total body surface area ranged from 1% to 60%. The most affected part of the body was the left hand in 55.26% cases. Presurgical preparation for self-grafting was necessary in 34.21% subjects, and the mean time elapsed was 37.5 days. The type of surgical treatment was serial debridement under general anesthesia in 100% of the patients, self-grafting in 31.6%, amputation in 18.4%, and fasciotomy in 5.3%. The mortality rate was 0%.
CONCLUSIONS: The study indicated that electrical burns occur most often in young adults in the workplace; therefore, policies should be developed to raise safety awareness in the workplace. Despite the severity of the injury, patients with adequate clinical support and early surgical evaluation are more likely to survive, even with high rates of amputation, confirming the need for more research on electroporation.
Keywords: Burns; Electrical burns; Work accidents; Epidemiology.
RESUMO
INTRODUÇÃO: Avaliar cinco anos de análise epidemiológica e tratamento cirúrgico atualizado das queimaduras elétricas por alta voltagem.
MÉTODOS: Foi realizado um estudo descritivo, retrospectivo de corte transversal, no Centro de Terapia de Queimados Dr. Oscar Plaisant, do Hospital Federal do Andaraí, Rio de Janeiro, Brasil, no período de janeiro de 2009 a dezembro de 2014. Foi aplicado um formulário nos prontuários dos 38 pacientes incluídos no estudo, a fim de avaliar as variáveis definidas.
RESULTADOS: Foram analisados 38 pacientes por queimadura elétrica de alta voltagem, sendo 95% dos casos do sexo masculino, com faixa etária entre 21-42 anos. O local de ocorrência mais frequente foi o trabalho, em 55,3%. A porcentagem de SCQ variou de 1-60%. A parte do corpo mais acometida foi a mão esquerda, em 55,26%. O preparo pré-cirúgico para autoenxertia foi necessário em 34,21%, sendo a média de tempo transcorrido 37,5 dias, o tipo de tratamento cirúrgico foi desbridamento seriado sob anestesia geral em 100%, autoenxertia em 31,6%, amputação em 18,4% e fasciotomia em 5,3% dos pacientes. A taxa de óbito foi de 0%.
CONCLUSÕES: O estudo observou que as queimaduras elétricas ocorrem mais frequentemente em adultos jovens no local de trabalho, portanto, é necessário desenvolver políticas de sensibilização para a segurança no local de trabalho. Apesar da gravidade da lesão, pacientes com suporte clínico adequado e avaliação cirúrgica precoce têm mais probabilidade de sobreviver, mesmo com altas taxas de amputação, confirmando a necessidade de mais pesquisas sobre a eletroporação.
Palavras-chave: Queimaduras; Queimaduras elétricas; Acidentes de trabalho; Epidemiologia.
Currently, burns remain a major public health problem worldwide, causing approximately 265,000 deaths each year for flame burns alone, with more deaths due to scalds and approximately 1000 deaths per year by electrical burns in the United States alone1,2, generating an important socioeconomic impact.
Voltage is classified into two types: low (<500 V) and high voltage (>500 V)2. High-voltage electrical burns have a higher incidence in adult male workers in the field of electricity who come into contact with high-voltage wires, sometimes without adequate protection, with disastrous consequences. On the other hand, low-voltage burns impact children, who during playful activities, introduce their fingers and oral cavity into outlets and household artefacts, causing injury almost exclusively at the contact point3-5.
High-voltage electrical burns differ clinically from thermal or chemical burns, as they cause much more subdermal damage. Frequently, they cause extensive injury in deeper structures, generating an impact on the central nervous system, consequently leading to the development of multiorgan dysfunction. However, initially, their extent and severity may be underestimated6.
The term electric trauma involves the following three main mechanisms, which determine the patient's prognosis: 1) electrical trauma by passage of an electric current, 2) electrical arcing, and 3) flame after ignition of clothing7. The treatment of injuries by high-voltage electrical burns often includes serial debridement, skin self-grafting, fasciotomy, local or free flaps, and in situations of extreme unviability of the affected limb, amputation of up to 75% of the limb8.
This paper describes the consequences of accidental contact with electrical current, its correlation with global epidemiology, and the principles involved in the surgical treatment of burns according to the past 5 years' experience of the Center of Burn Treatment Dr. Oscar Plaisant of the Federal Hospital of Andaraí (CTQ-HFA) in Rio de Janeiro, Brazil.
OBJECTIVE
To analyze cases of high-voltage electrical burns and the surgical treatment performed during the period evaluated, in comparison with the current global statistics.
METHODS
From January 2009 to December 2014, a descriptive, retrospective cross-sectional study was conducted at the CTQ-HFA. The study sample consisted of 38 patients, including all those hospitalized and diagnosed as having high-voltage electrical burns. Patients with low-voltage electrical burns were excluded. A standard form elaborated by the authors was designed and applied.
The sources of information were the medical records of the patients, which were provided by the department of statistics and filing of the HFA. The following epidemiological indicators were evaluated: sex, age, place of occurrence, percentage of burned total body surface area (TBSA), body part affected, duration of preoperative preparation, type of surgical treatment, and mortality rate. These data were analyzed based on descriptive statistics.
This study complied with the principles of the Declaration of Helsinki of the World Medical Association-Ethical Principles for Medical Research Involving Human Subjects, 59th General Assembly of the World Medical Association, Seoul, October 2008. The research met the guidelines and regulatory standards for research involving human subjects provided for in Resolution No. 466 of 12/12/12 of the National Health Council of the Ministry of Health.
RESULTS
Thirty-eight patients hospitalized for high-voltage burns were evaluated, 95% of whom were male (Figure 1), aged between 21 and 42 years. The most frequent location of the occurrence was the workplace in 55.3% of the cases. The percentage of burned TBSA ranged from 1% to 60%. The most affected part of the body was the left hand in 55.26%. Presurgical preparation for self-grafting was necessary in 34.21%, and the average time elapsed was 37.5 days.
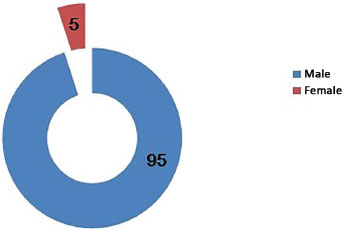
Figure 1. Distribution of all cases analyzed according to sex.
The type of surgical treatment used was serial debridement under general anesthesia in 100% of the cases, self-grafting in 31.6%, amputation in 18.4%, and fasciotomy in 5.3% of the patients (Figure 2).
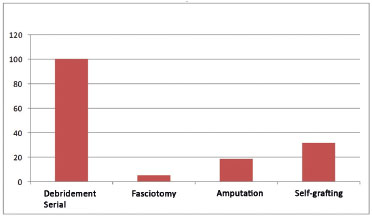
Figure 2: Percentage distribution of the type of surgical treatment initiated.
The mortality rate was 0%. Of the total number of amputations, 65% occurred between the first and the 10th day, and the limit to complete the necessary amputations was until the 20th day. From day 21, the rest of the cases were treated with self-grafting (Figure 3). The case shown in Figure 4 illustrates a mechanism of entry of electrical current in the palms of the hands (Figure 4), the extensive area of exit of the electrical current in the dorsal region (Figure 5), and the area prepared to perform skin self-grafting (Figure 6).
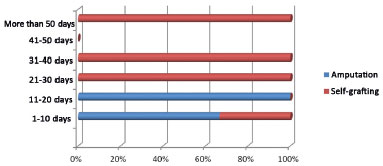
Figure 3. Temporal distribution of amputation and grafting.

Figure 4. Electrical burns and region of entry of current in the hands.

Figure 5. Patient with electrical burns, showing the exit wound of the current in the dorsal region.

Figure 6. Epithelization area in the affected region, ready for self-grafting.
DISCUSSION
Several series have shown the statistical predominance of the male sex in the incidence of high-voltage burns and the age of patients to range from 14 to 55 years. Pham et al.9 demonstrated in a multicenter study that in patients aged >55 years, electrical trauma constitutes only 1.6% of all trauma cases of this type. This is related of course with the professional activity in itself and the age of retirement.
The rate of injury in adults is significantly higher among men than among women. Several series have shown that these lesions are present in up to 80% of male patients, without racial proneness, most likely owing to occupational bias10. Our study results are in agreement with these data, with an age interval of 21-42 years.
The percentage of burned body surface area has been widely demonstrated as a major risk factor of mortality due to trauma. Gokdemir et al.11 reported burned TBSA of >20% and patient age of >40 years as direct risk factors of mortality. Our study showed extensive variability in TBSA between 1% and 60% (mean, 29.5%), without association with mortality, which may be related to the stabilization protocols, and initial and continuous clinical management initiated during the treatment period.
Nevertheless, it is crucial to emphasize that in this specific type of burns, the severity of the injury could not be determined based solely on the burned TBSA or on the places of entry and exit of electrical current because, on its course, electricity causes thermal injury in cells and tissues in its path, causing damage to multiple body organs and systems. The ideal time between the occurrence of trauma and the implementation of skin autograft is controversial.
Gokdemir et al.11 indicated that no generally accepted consensus has been reached regarding the ideal method. When the nonviable tissue is debrided early in preparation for grafting, even with the appearance of appropriate conditions in bed to accept the new tissue, on some occasions, the trauma is not yet definitive, and subsequent tissue necrosis with graft loss may occur. On the other hand, when grafting is executed after the 14th day after trauma, highlighting the area of necrosis to be debrided would be easier, but loss of apparently viable tissue can still be observed even after the 20th day.
In our series, the average time required for grafting was 37.5 days, reflecting an orientation of a more conservative conduct, with favorable results and without loss of grafts. Serial debridement under general anesthesia is part of the routine treatment for burned patients. Depending on the extent and depth of the burns, the decisions are made regarding the type of agent to be used during balneotherapy and the optimum time of preparation for posterior surgical procedures or as definitive treatment12. All the patients who attended our unit received this therapeutic modality.
For other burn etiologies, more-complex procedures tend to be performed more frequently, such as fasciotomy for prevention of compartment syndrome and limb salvage, which must be performed between the first 6 and 8 hours after the initial injury, if involvement is suspected. In other series, these represent up to 27%; while in the present study, an incidence of only 5.3% was observed for this type of procedure.
Amputations, which in our sample accounted for 18.4%, required implementation up to the tenth day on average because of the risk of infection of nonviable tissue or frank segmental necrosis of the affected limb. Other series reported a relatively similar rate of around 12%13.
Reconstruction with distal flaps (cross arm or abdominal) has practical disadvantages to be considered, such as the need for immobilization of the limb and consequent edema, in addition to extended hospitalization, which generates more costs. Therefore, whenever possible, local flaps or, in selected cases, microsurgical free flaps should be used14,15. In the sample analyzed, this type of reconstruction need not be performed.
CONCLUSION
This study shows a strong preponderance of high-voltage burns in the subgroup of workers, specifically in the area of construction and electricity. Thus, if a direct relationship exists between cause and effect due to the type of work, on the other hand, we can infer a significant precariousness in the prevention of work accidents and protection of workers.
When comparing with the literature, we observed no death in our study. However, the question of how many of these patients do not arrive at specialized treatment centers or were treated at other institutions remains unanswered. Strategies focused on this objective of absolute importance for an effective reduction in the incidence of this tragic outcome, which in an important number of cases, jeopardizes the life and the quality of life of patients, and stimulating scientific research in this area could contribute effectively to the improvement of the management protocols of burn victims.
COLLABORATIONS
THT Final approval of the manuscript, conception and design of the study, and draft of the manuscript or critical review of its contents.
JASR Analysis and/or interpretation of data, statistical analysis, conception and design of the study, and draft of the manuscript or critical review of its contents.
RCR Final approval of the manuscript.
KC Statistical analysis, and conception and design of the study.
MCVF Final approval of the manuscript.
LMJ Final approval of the manuscript.
REFERENCES
1. World Health Organization. Burn fact sheet no 365. 2014. [Acesso 2016 Jul 4]. Disponível em: http://www.who.int/mediacentre/factsheets/fs365/en/
2. Gajbhiye AS, Meshram MM, Gajaralwar RS, Kathod AP. The management of electrical burn. Indian J Surg. 2013;75(4):278-83.
3. Lengyel P, Frišman E, Babík J, Orság J, Baran M, Gajdoš J. Electrical burns in our workplace. Acta Chir Plast. 2014;56(1-2):13-4.
4. Zámecníková I, Stĕtinský J, Tymonová J, Kadlcík M. Burn injury in children. Acta Chir Plast. 2005;47(1):13-5.
5. Salehi SH, Fatemi MJ, Aśadi K, Shoar S, Ghazarian AD, Samimi R. Electrical injury in construction workers: a special focus on injury with electrical power. Burns. 2014;40(2):300-4.
6. Ghavami Y, Mobayen MR, Vaghardoost R. Electrical burn injury: a five-year survey of 682 patients. Trauma Mon. 2014;19(4):e18748.
7. Sanford A, Gamelli RL. Lightning and thermal injuries. Handb Clin Neurol. 2014;120:981-6.
8. Lipový B, Rihová H, Kaloudová Y, Suchánek I, Gregorová N, Hokynková A, et al. The importance of a multidisciplinary approach in the treatment of mutilating electrical injury: a case study. Acta Chir Plast. 2010;52(2-4):61-4.
9. Pham TN, Kramer CB, Wang J, Rivara FP, Heimbach DM, Gibran NS, et al. Epidemiology and outcomes of older adults with burn injury: an analysis of the National Burn Repository. J Burn Care Res. 2009;30(1):30-6.
10. Luz DP, Millan LS, Alessi MS, Uguetto WF, Paggiaro A, Gomez DS, et al. Electrical burns: a retrospective analysis across a 5-year period. Burns. 2009;35(7):1015-9.
11. Gokdemir MT, Aldemir M, Sogut O, Guloglu C, Sayhan MB, Orak M, et al. Clinical outcome of patients with severe burns presenting to the Emergency Department. J Current Surg. 2012;2(1):17-23.
12. Agbenorku P. Modernized standards in burns management: a comparative study in Komfo Anokye Teaching Hospital, Kumasi, Ghana. Burns. 2013;39(5):990-6.
13. Fernandes FM, Torquato IM, Dantas MS, Pontes Júnior Fde A, Ferreira Jde A, Collet N. Burn injuries in children and adolescents: clinical and epidemiological characterization. Rev Gauch Enferm. 2012;33(4):133-41.
14. Gajbhiye AS, Meshram MM, Gajaralwar RS, Kathod AP. The management of electrical burn. Indian J Surg. 2013;75(4):278-83.
15. Agbenorku P, Agbenorku E, Akpaloo J, Obeng G, Agbley D. Electrical burns: The trend and risk factors in the Ghanaian population. Ann Burns Fire Disasters. 2014;27(4):176-83.
1. Hospital Santa Casa de Misericórdia do Rio de Janeiro, Rio de Janeiro, RJ, Brazil
2. Hospital Casa de Portugal, Rio de Janeiro, RJ, Brazil
3. Hospital Federal do Andaraí, Rio de Janeiro, RJ, Brazil
4. Sociedade Brasileira de Queimaduras, Rio de Janeiro, Rio de Janeiro, RJ, Brazil
Institution: Hospital Santa Casa de Misericórdia do Rio de Janeiro, Rio de Janeiro, RJ, Brazil.
Corresponding author:
Thiago Henrique Tondineli
Rua Professor Gastão Bahiana, 496, Apt 1010 - Lagoa
Rio de Janeiro, Brazil Zip Code 22071-030
E-mail: thitondi@yahoo.com.br
Article received: October 5, 2015.
Article accepted: May 12, 2016.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter