

Original Article - Year 2016 - Volume 31 - Issue 3
Greater omentum flap in the treatment of infant postoperative mediastinitis
Retalho de omento maior no tratamento da mediastinite pós-operatória do lactente
ABSTRACT
INTRODUCTION: Postoperative mediastinitis is a serious condition that presents high mortality rates. The greater omentum flap has been used with good results in postoperative mediastinitis after cardiac surgery. The use of this approach has not been reported in infants probably because at this age, the greater omentum is membranous, not bulky, and has little amount of fatty tissue.
METHOD: Between July 2010 and August 2014, four infants who presented with mediastinitis after a cardiac surgery via sternotomy were treated. The surgical treatment consisted of steel wire removal, debridement, and wound washing, followed by transposition of the entire greater omentum to the mediastinal cavity. Surgical treatment was performed in a single step. No rewiring of the sternum was performed.
RESULTS: All four patients survived the treatment and were discharged from the intensive care unit without infection.
CONCLUSIONS: Although membranous and not bulky, the use of a greater omentum flap proved to be an excellent approach in infant postoperative mediastinitis.
Keywords: Mediastinitis; Sternotomy; Omentum; Cardiovascular surgical procedures; Infant.
RESUMO
INTRODUÇÃO: A mediastinite pós-operatória é uma condição grave, com altas taxas de mortalidade. O retalho de omento maior é usado com êxito no tratamento de mediastinites pós-operatórias decorrentes de cirurgia cardíaca. O uso dessa abordagem não foi relatado em lactentes, provavelmente porque nessa idade o omento maior é membranáceo, pouco volumoso e possui tecido adiposo escasso.
MÉTODOS: Entre julho de 2010 e agosto de 2014, foram tratados quatro lactentes com mediastinite pós-operatória decorrentes de cirurgia cardíaca, realizada por esternotomia. O tratamento cirúrgico consistiu em remoção dos fios de aço da osteossíntese esternal, desbridamento e lavagem do mediastino, seguidos da transposição de todo o omento maior para a cavidade mediastinal. O tratamento cirúrgico foi feito em um só tempo. Não foi feita nova síntese do esterno com fios de aço.
RESULTADOS: Os quatro pacientes sobreviveram ao tratamento e obtiveram alta da unidade de tratamento intensivo sem infecção.
CONCLUSÕES: Embora membranáceo e apresentando pequeno volume, o retalho de omento maior se mostrou um excelente método de abordagem da mediastinite pós-operatória do lactente.
Palavras-chave: Mediastinite; Esternotomia; Omento; Procedimentos cirúrgicos cardiovasculares; Lactente.
Milton1 introduced sternotomy for the mediastinal approach. Julian et al.2 described the method and made it known. Sternotomy became the most used approach worldwide to access the heart and great vessels. According to Engelman et al.3, the open method for treating postoperative mediastinitis was introduced by Spencer in 1961.
The open method, which is associated with high mortality, involves the removal of synthesis material (e.g., suture stitches and steel wires), followed by dressings, until healing is achieved by secondary intention. Kiricuta4 was the first to use a greater omentum flap in chest wall reconstruction in a case of breast cancer. Shumacker and Mendelbaum5 described a closed method of irrigation of the mediastinum that involves the use of antibiotics or antiseptic solutions such as povidone-iodine, administered through catheters, and performed after debridement of the mediastinum and new synthesis of the sternum.
Lee et al.6 introduced the greater omentum flap for the treatment of mediastinitis after cardiac surgery. Jurkiewicz et al.7 reported the use of pectoralis major muscle flaps for the treatment of mediastinitis. Since then, the flaps of the pectoralis major and rectus abdominis muscles have become widely used in the management of the surgical complications.
Since 1990, hyperbaric oxygen therapy has been used as an ancillary method in postoperative mediastinitis management. Although signs of better results were demonstrated in a small series in which the method was used, the real effectiveness of oxygen therapy is difficult to evaluate because of the different surgical approaches used in the treatment of such patients8.
Argenta and Morykwas9 introduced the use of vacuum-assisted closure (VAC) in the management of difficult treatment wounds. VAC can be translated to Portuguese as fechamento auxiliado pelo vácuo. Mendez-Eastman8, Obdeijn et al.10, and Tang et al.11 were the forerunners of the use of VAC in the treatment of mediastinitis.
Since 1994, the use of greater omentum flap became the approach of choice for postoperative mediastinitis treatment at the Clinic of Plastic Surgery of Felicio Rocho Hospital, in Belo Horizonte (MG). Silva Filho12 reported 20 cases of mediastinitis treated with greater omentum flaps in which only one death occurred, which was not connected with the technique used, although several patients were in extremis.
Increasingly severe operations, elderly and debilitated patients, and the treatment of newborns and infants with complex malformations are factors that have occasioned the appearance of serious complications such as postoperative mediastinitis. Mortality rates vary depending on the medical institution evaluated.
Mediastinitis is a serious life-threatening condition. In our country, surgeons usually delay treatment to allow the disease to resolve with antibiotics. Postponing debridement after diagnosis, irrespective of the method used for closing the wound, invariably leads to worsening of the clinical condition.
Pairolero et al.13 divided sternotomy infections into three types. Type 1 occurs in the early postoperative days. The drainage is serohemorrhagic; bacterial culture results can be negative; and cellulitis, osteomyelitis, or chondritis is absent. The mediastinum is soft and flexible. Type 2 occurs in the first weeks after the operation. The culture results are positive, the drainage contains pus, cellulitis and purulent mediastinitis are present, osteomyelitis frequently occurs, and chondrites are rarely found. The mediastinum may be hardened and thick. Type 3 occurs months after sternotomy. Chronic drainage contains pus from cutaneous fistulas, culture results are positive, and osteomyelitis, costochondritis, and foreign body reaction to the synthetic material in the sternum are present. Type 2 is the most severe type of mediastinitis.
OBJECTIVE
To determine if greater omentum transplantation, which has never been reported in the available medical literature, is effective in the treatment of postoperative mediastinitis in infants, following sternotomy.
METHODS
Data of four infants treated between July 2010 and August 2014, who presented with postoperative mediastinitis due to median sternotomy performed during cardiac surgery were reviewed. All the patients underwent surgery at the Hospital Felicio Rocho in Belo Horizonte, MG. Data were collected regarding sex, age, diagnosis that led to sternotomy, onset of the signs of postoperative mediastinitis, identification of microbial agents, omental transposition technique, postoperative complications, antimicrobial treatment, and time elapsed between the greater omentum transplantation and discharge from the intensive care unit (ICU).
Existing literatures were reviewed by using the following keywords: "mediastinitis," "sternotomy," "omentum majus," "greater omentum," "cardiac surgery," "infant," "mediastinite," "esternotomia," "omento maior," "cirurgia cardíaca," and "lactente."
This retrospective study was approved by the research ethics committee of Hospital Felicio Rocho (protocol No. CEP/HFR 433/14). An informed consent form was provided to the relatives or guardians of the patient prior to the surgery.
Surgical treatment was performed on an urgent basis, always under general anesthesia and endotracheal intubation. It was started with the complete opening of the sternotomy, the removal of the steel wires of the sternum, the debridement of necrotic tissue, and the extensive washing of the mediastinum with 0.1% povidone-iodine solution in saline. The debridement was economical, as it did not require sternectomy and costectomy. Omentum exposition was performed by using supraumbilical median laparotomy.
In three cases, the greater omentum was elongated by colo-omental detachment and ligature of the right gastro-omental pedicle, keeping the flap pedicled on the left gastro-omental vessels. In one case, the greater omentum was elongated by colo-omental detachment and ligature of the left gastro-omental pedicle, keeping the flap pedicled in the right gastro-omental vessels.
The greater omentum flap was transposed to the mediastinum through a transdiaphragmatic incision. The synthesis of the abdominal wall was executed by layers. The mediastinum was closed by suturing the subcutaneous tissue and skin, without rewiring of the sternum. All the patients received continuous suction tubular drainage for a few days until the drainage volume of secretions was reduced. All the patients empirically received systemic antibiotic therapy. Whether medications had to be changed or not was determined based on the results of Gram staining, cultures, and susceptibility tests.
Casuistic Description of Cases
Case 1 (Figures 1 to 7) was a male infant aged 5 months 13 days, weighing 4.3 kg, who underwent correction of the large interventricular communication (ventricular septal defect [VSD]) and pulmonary valvuloplasty on July 2, 2010. On the 12th postoperative day, surgical wound dehiscence was observed and mediastinitis was diagnosed. The cardiovascular surgeon performed wound debridement and primary closure. The infection worsened.

Figure 1. Case 1 - Purulent mediastinitis showing skin with residues of povidoneiodine from closed irrigation.

Figure 2. Case 1 - Debridement: removal of necrotic debris and synthetic material.
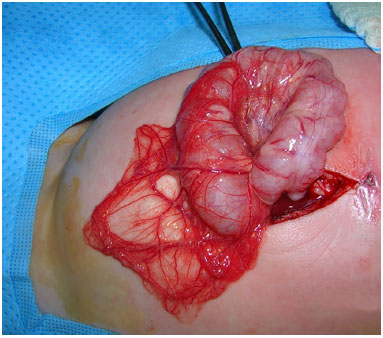
Figure 3. Case 1 - Supraumbilical median laparotomy and exposure of the greater omentum.
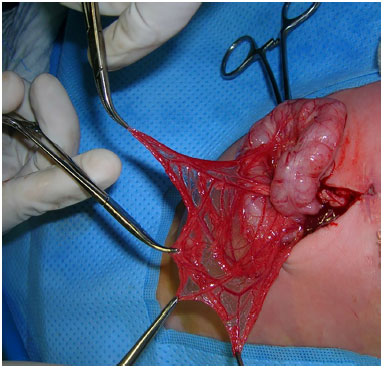
Figure 4. Case 1 - Exposure of the greater omentum, revealing the macroscopic absence of adipose tissue.
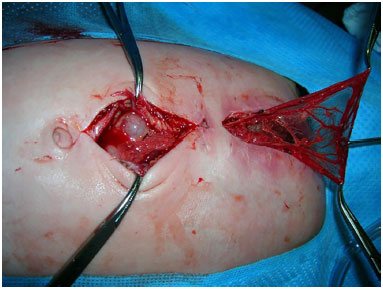
Figure 5. Case 1 - Transfer of the omentum into the mediastinum.

Figure 6. Case 1 - The greater omentum transferred into the mediastinum.

Figure 7. Case 1 - Wound closure and suction drainage.
On July 21, 2010, the patient was diagnosed as having purulent mediastinitis type 2 according to the criteria of Pairolero et al.13 A new debridement was performed, followed by transplantation of the greater omentum to the mediastinum. The transplant was pedicled in the right gastro-omental vessels (artery and vein) and transferred to the chest through a transdiaphragmatic incision. Blood cultures yielded methicillin-resistant Staphylococcus aureus (MRSA). Meropenem (until July 17, 2010) and vancomycin (until August 9, 2010) were prescribed. The evolution of the surgical wound was uneventful, and the patient was discharged from the ICU, cured of the infection, on August 16, 2010, 27 days after the transplantation of the greater omentum.
Case 2 (Figures 8 to 11) was a male infant aged 6 months 26 days, weighing 6.4 kg, who received heart surgery for tetralogy of Fallot (Blalock's operation) on November 29, 2010. On the eighth postoperative day, the patient was diagnosed with sero-hemorrhagic mediastinitis (Pairolero et al.13 type 1).

Figure 8. Case 2 - Serohemorrhagic mediastinitis.

Figure 9. Case 2 - Supraumbilical median laparotomy and exposure of the greater omentum.

Figure 10. Case 2 - The greater omentum transferred into the mediastinum.

Figure 11. Case 2 - Postoperative appearance on October 16, 2013, showing the patient in optimal conditions, 34 months after the transplantation of the greater omentum.
On December 7, 2010, the patient received debridement and transplantation of the greater omentum, pedicled on the left gastro-omental vessels, transferred to the chest through a transdiaphragmatic incision. Blood culture results were negative. In the tracheal aspirate, Pseudomonas aeruginosa was detected. Antibiotic therapy was scheduled for 6 weeks, consisting of vancomycin and piperacillin + tazobactam. Complete remission of the infection was observed. The patient was discharged from the ICU, cured of the infection, on January 6, 2011, 29 days after the transplantation of the greater omentum.
Case 3 was a male infant aged 4 months 6 days, weighing 3.3 kg, who was diagnosed as having Down's syndrome and tetralogy of Fallot. On November 9, 2010, the patient received heart surgery that consisted of pulmonary artery banding with a polytetrafluoroethylene (PTFE) strip and ductus arteriosus ligature. On the tenth postoperative day, he was diagnosed as having purulent mediastinitis (Pairolero et al.13 type 2).
On November 19, 2010, the patient underwent greater omentum transplantation, pedicled in the left gastro-omental vessels, transferred to the chest through a transdiaphragmatic incision. The mediastinal tissue culture yielded Staphylococcus aureus. The patient presented pleural empyema, which was drained by thoracotomy in December 23, 2010. The antibiotic therapy consisted of vancomycin and piperacillin + tazobactam until the sixth week, with complete remission of the infection. The patient was discharged from the ICU without infection on January 5, 2011, 44 days after the greater omentum transplantation.
Case 4 was a female infant aged 9 months 29 days, weighing 8.4 kg, who was diagnosed as having tetralogy of Fallot and received surgical correction of a VSD on July 22, 2014. On August 5, 2014, the patient presented mediastinitis. The cardiovascular surgeon performed debridement of the mediastinum and immediate closure, with drainage of the cavity. Worsening of the infection was observed.
On August 8, 2014, the patient had purulent mediastinitis (Pairolero et al.13 type 2). She underwent debridement and transplantation of the greater omentum, pedicled in the left gastro-omental vessels and transferred to the mediastinum through a transdiaphragmatic incision. Blood sample culture yielded beta lactamase-positive Staphylococcus aureus. The antibiotic therapy consisted of vancomycin adminstration for 28 days.
The patient was discharged from the ICU without infection on September 2, 2014, 15 days after the omentum transplantation.
RESULTS
All four patients with postoperative mediastinites treated with greater omentum transplantation were cured and discharged from the ICU without infection. The postoperative period in the ICU, after greater omentum transplantation, ranged from 15 to 44 days. The length of ICU stay was 27 days in case 1, 29 days in case 2, and 15 days in case 4. In case 3, the patient was admitted in the ICU for 44 days owing to pleural empyema that required drainage by exploratory thoracotomy. The average length of stay in the ICU considering the four cases was 28.75 days.
DISCUSSION
The first description of the use of the greater omentum flap was by Drummond and Morison14 in two cases of patients with ascites treated with a portosystemic shunt. The peritoneum of the anterior wall of the abdomen, liver, and the spleen were scarified by rubbing with a sponge. The greater omentum flap was sutured to the scarified area. Absorption of the ascites was observed.
Morison15, in 1906, called the greater omentum the "policeman of the abdomen" because of its exceptional ability to block inflammation and fistulas of the intra-abdominal organs. He also described the angiogenic capacity of the omentum, noting its adherence to tumors of the ovary and tuba uterina. He observed that the greater omentum resembles a jellyfish that can move and adapt to projections and recesses of the abdomen.
Williams16 thoroughly described greater omentum angiogenesis. It is the formation of new blood vessels, different from increased vascularity by vasodilation or vascular elongation. It is essential in several normal or pathological conditions such as tissue and organ growth, chronic inflammation, wound healing, cancer, and immune reactions. Profuse vascular network is located under the peritoneal surface of the omentum. Macrophages and mast cells capable of inducing angiogenesis are attached to omental capillaries.
Under adequate stimulation, angiogenic activities occur in omental vessels. Vascular penetrations and connections to adjacent tissue vessels are established. Angiogenic factors were isolated from cat omentum16. Wornom III et al.17 treated successfully seven cases of mediastinitis after heart transplantation by using greater omentum transplantation. They drew attention to the large dead space around the transplanted heart, which is generally smaller than the diseased organ. The greater omentum can fill the dead space around the transplant.
The only reported use of the greater omentum in newborns in the literature is that in the work of Bonnard et al.18 that described the treatment of a tracheoesophageal fistula with esophageal atresia in two children. One of the children underwent surgery at 2 days of age. Postoperative fistula formation was found and was reoperated but recurred. Use of a greater omentum flap was decided after the repair of the recurrent fistula. The flap was harvested by using videoendoscopy, with healing of the fistula.
The second patient, who presented with esophageal atresia and tracheoesophageal fistula, underwent surgery at 1 day of age. Biological glue was used in an attempt to repair the fistula, but without any result. Stenosis of the esophagus and tracheomalacia were found. Regardless of esophageal dilations and reoperation, the fistula persisted. The fistula was closed, and the greater omentum flap was used in the reoperation, with rapid recovery of the newborn.
Cases 1 (Figures 1 to 7), 3, and 4 had frank purulent mediastinitis (Pairolero et al.13 type 2). This condition can become life-threatening and needs urgent care. Case 2 (Figures 8 to 11) showed serohemorrhagic mediastinal drainage (Pairolero et al.13 type 1).
The treatment of choice in postoperative mediastinitis is not defined in the medical literature. Different methods are adopted by various surgeons. The open method uses dressings, closed drainage with antiseptic or antibiotic irrigation, and several muscle flaps to fill in the mediastinum. The authors of the present study consider the greater omentum flap as the treatment of choice for postoperative mediastinitis12,19, owing to its capacity to fill in the mediastinal cavity, without leaving dead spaces, besides the great angiogenic capacity of that portion of the peritoneum.
CONCLUSION
Although membranous and not bulky, the greater omentum flap proved to be excellent for use in the treatment of infant postoperative mediastinitis.
COLLABORATIONS
NAP Contributed to surgeries and/or experiments.
AFSF Contributed to surgeries and/or experiments.
JCRRA Contributed to the analysis; interpretation of data; approval of the final version to be published; conception and design of the study; drafting the manuscript and critical review of content of the study.
EHP Contributed to the analysis; interpretation of data; approval of the final version to be published; conception and design of the study; drafting the manuscript and critical review of content of the study.
MOR Contributed to surgeries and/or experiments.
RPLF Contributed to surgeries and/or experiments.
CAS Contributed to surgeries and/or experiments.
ACMA Contributed to the analysis, interpretation of data.
RLFS Contributed to the analysis interpretation of data, statistical analysis
REFERENCES
1. Milton H. Mediastinal surgery. Lancet. 1897;149(3839):872-5.
2. Julian OC, Lopez-Berlio M, Dye WS, David H, Grove WJ. The median sternal incision in intracardiac surgery with extracorporeal circulation; a general evatuation of its use in heart surgery. Surgery. 1957;42(4):753-61.
3. Engelman RM, Williams CD, Gouge TH, Chase RM Jr, Falk EA, Boyd AD, et al. Mediastinitis following open-heart surgery. Review of two years' experience. Arch Surg. 1973;107(5):772-8.
4. Kiricuta I. L'emploi du grand épiploon dans la chirurgie du sein cancéreux. Presse Med. 1963;71:15-7.
5. Shumacker Jr HB, Mandelbaum I. Continuous antibiotic irrigation in the treatment of infection. Arch Surg. 1963;86:384-7.
6. Lee AB Jr, Schimert G, Shaktin S, Seigel JH. Total excision of the sternum and thoracic pedicle transposition of the greater omentum; useful strategems in managing severe mediastinal infection following open heart surgery. Surgery. 1976;80(4):433-6.
7. Jurkiewicz MJ, Bostwick J 3rd, Hester TR, Bishop JB, Craver J. Infected median sternotomy wound. Successful treatment by muscle flaps. Ann Surg. 1980;191(6):738-44.
8. Mendez-Eastman S. Use of hyperbaric oxygen and negative pressure therapy in the multidisciplinary care of a patient with nonhealing wounds. J Wound Ostomy Continence Nurs. 1999;26(2):67-76.
9. Argenta LC, Morykwas MJ. Vacuum-assisted closure: a new method for wound control and treatment: clinical experience. Ann Plast Surg. 1997;38(6):563-76.
10. Obdeijn MC, de Lange MY, Lichtendahl DH, de Boer WJ. Vacuum-assisted closure in the treatment of poststernotomy mediastinitis. Ann Thorac Surg. 1999;68(6):2358-60.
11. Tang AT, Ohri SK, Haw MP. Novel application of vacuum assisted closure technique to the treatment of sternotomy wound infection. Eur J Cardiothorac Surg. 2000;17(4):482-4.
12. Silva Filho AF. Retalhos de epiploon nas esternotomias infectadas. Trabalho apresentado à SBCP para obtenção da condição de Membro Titular. Belo Horizonte; 1997.
13. Pairolero PC, Arnold PG, Harris JB. Long-term results of pectoralis major muscle transposition for infected sternotomy wounds. Ann Surg. 1991;213(6):583-9.
14. Drummond D, Morison R. A case of ascites due to cirrhosis of the liver cured by operation. Br Med J. 1896;2:728-9.
15. Morison R. On functional aspects of the greater omentum. Br J Med. 1906;1:76-8.
16. Williams R. Angiogenesis and the greater omentum. In: Goldsmith HS, ed. The omentum. Research and clinical applications. New York: Springer-Verlag; 1988. p.45-61.
17. Wornom IL 3rd, Maragh H, Pozez A, Guerraty AJ. Use of the omentum in the management of sternal wound infection after cardiac transplantation. Plast Reconstr Surg. 1995;95(4):697-702.
18. Bonnard A, Paye-Jaouen A, Aizenfisz S, El Ghoneimi A. Laparoscopically harvested omental flap for recurrent tracheoesophageal fistula in a newborn baby. J Thorac Cardiovasc Surg. 2007;134(6):1592-3.
19. Sampaio DT, Alves JCR, Silva AF, Lobo Júnior NC, Simões D, Faria W, et al. Mediastinite em cirurgia cardíaca: tratamento com epíploon. Rev Bras Cir Cardiovasc. 2000;15(1):23-31.
1. Sociedade Brasileira de Cirurgia Plástica, Belo Horizonte, MG, Brazil
2. Hospital Felício Rocho, Belo Horizonte, MG, Brazil
3. Instituto de Cirurgia Plástica Avançada, Belo Horizonte, MG, Brazil
4. Universidade Federal de Minas Gerais, Belo Horizonte, MG, Brazil
5. Faculdade da Universidade de Itaúna, Belo Horizonte, MG, Brazil
6. Academia Mineira de Medicina, Belo Horizonte, MG, Brazil
7. Sociedade Brasileira de Cirurgia Cardiovascular, Belo Horizonte, MG, Brazil
Institution: Clínicas de Cirurgia Plástica e Cirurgia Cardiovascular do Hospital Felício Rocho, Belo Horizonte, MG, Brazil.
Corresponding author:
Erick Horta Portugal
Rua Santa Maria de Itabira, 217 - Sion
Belo Horizonte, MG, Brazil Zip Code 30310-600
E-mail: erickhphp@yahoo.com.br
Article received: March 22, 2016.
Article accepted: August 6, 2016.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter