

Articles - Year 2003 - Volume 18 -
Marcus Gunn Syndrome
Síndrome de Marcus Gunn
ABSTRACT
The authors present a case of Marcus Gunn Syndrome, whose major feature is the synkinetic movement between mastication muscles and the upper eyelid, present in five per cent of the cases of congenital blepharoptosis. In the case presented, the synkinesia was observed between the left lateral ptreygoid and the upper right eyelid. The etiology of the Marcus Gunn phenomenon is not known and treatment is mainly aimed at the palpebral ptosis, when it is severe, by resecting or transposing the levator muscle and correcting other extra-ocular lesions, such as strabismus, amblyopia, anisometropia and other conditions detected by specialized examination. The diagnosis is generally made early by the child's parents or guardians who observe the synkinetic movement while nursing or fieding the infant. The assisting physician, or specialist, guides the treatment, mainly in relation to the indication or occasion for correcting major lesions. It is noteworthy to point out that the correction of the palpebral ptosis should, whenever possible, be accompanied by surgery of the palpebral levator in order to avoid the even more exaggerated permanence of the palpebral synkinesia.
Keywords: Marcus Gunn Syndrome; congenital palpebral ptosis; blepharoptosis
RESUMO
É apresentado um caso da síndrome de Marcus Gunn, cuja principal característica é o movimento sincinético entre a musculatura mastigatória e a pálpebra superior, presente em cinco por cento dos casos de blefaroptose congênita. No caso apresentado, a sincinesia foi observada entre a ação do pterigóideo lateral esquerdo e a pálpebra superior direita. A etiologia do fenômeno de Marcus Gunn é desconhecida, e o tratamento direciona-se principalmente para a ptose palpebral, quando severa, com ressecção ou transposição do músculo elevador palpebral e correção de outras lesões extra-oculares, como estrabismo, ambliopia, anisometropia e outras, detectadas pelo exame especializado. O diagnóstico em geral é feito precocemente, pelos pais ou responsáveis pela criança, que observam o movimento sincinético durante a amamentação ou alimentação do infante, cabendo ao médico assistente, ou especialista, orientar o tratamento, principalmente no que diz respeito à sua indicação ou oportunidade da correção das lesões principais. É importante notar que a correção da ptose palpebral deve sempre que possível ser acompanhada por cirurgia do elevador palpebral, a fim de evitar a permanência ainda mais exagerada da sincinesia palpebral.
Palavras-chave: Síndrome de Marcus Gunn; ptose palpebral congênita; blefaroptose
We present a case of Marcus Gunn Syndrome with the objective of re-establishing the knowledge of this condition that sometimes surprises the specialist, because it is arare phenomenon in daily clinical practice. It is a synkinesia between the movement of the masticating muscles, mainly the lateral pterygoids and opposite side palpebral levator, where the chewing movement is voluntary and the elevation of the eyelid involuntary and simultaneous(1,2), sometimes bringing about psychosocial discomfort to those with the condition. It occurs in five percent of cases of congenital palpebral ptosis, according to most authors, along with other accompanying eye lesions (1,2,3).
REVISION AND DIAGNOSIS
The Marcus Gunn (Robert Marcus Gunn) syndrome or phenomenon was described by the author of the same name in 1883, in a case report published in the Transactions of Ophtalmologic Society (UK), according to citation of Timothy W. Doucet in the American Journal of Ophtalmology(2,4). It is a syndrome comprised by synkinesia already described, and by other eye lesions such as strabismus, amblyopia, anisometropia and other possible co-existing extra or intra-ocular lesions. Diagnosis may be made early from the observations of the parents of the child bom with palpebral ptosis - because the Marcus Gunn phenomenon may present while baby is being nursed or fed - and drawn to the attention of the physician, pediatrician or ophthalmologist, who will not always be artentive to or know about the syndrome. The ophthalmologic examination will be very important to adequately assess, in addition to the palpebral ptosis (uni or bilateral), other ocular conditions that may be associated, as is frequently the case in the Marcus Gunn Syndrome, whose treatment may be initially more important than the palpebral ptosis itself. The actual nature of the neurological circuit that produces the synkinesia, in which motor branches of the trigerninus nerve make an incorrect connection with branches of the common ocular motor nerve, mainly at the innervation of the upper eyelid levator muscle, remains unknown (5). The synkinetic phenomenon may be triggered by the following movements (mouth): mouth opening, lateral mandible movements, chewing, sucking, teeth grinding and swallowing. The lateralizing movements of the mandible or teeth grinding are the most frequent movements that trigger the synkinesia. The elevation of the eyelid is more noticeable, the more accentuated the ptosis and is even more noticeable if the axis of the eye is directed downwards, as the sclera is more exposed in this position(1).
Ocular motor disorders occur in 5% of congenital palpebral ptoses with Marcus Gunn synkinesia. The latter is associated with strabismus in 50-60% of cases, with anisometropia in 25% and with amblyopia in 30-50%. Palpebral ptosis may be mild (less than or equal to 2 mm), moderare (3 mm), or severe (above 4 mm). There is no difference in incidence regarding gender, color of skin or race or family origin. Some authors relate heart arrhythmias and hypertherrnia during anesthesia in cases of Marcus Gunn Syndrome(6).
CASE REPORT
Patient S.T.M.S., white, female, 38 years old, born and living in the state of Rio de Janeiro (Macaé), without any personal or family backgraund condition related with the case, wanted to have esthetic rhinoplasty. She presented a mild right palpebral ptosis, only visible as a small alteration of the palpebral rim whose vertical axis was 2 mm less than the left one. The eye exam by the ophthalmologist did not reveal any abnormality, in terms of refraction, amblyopia or motor lesion. The patient herself drew the author's attention to the involuntary winking of the right upper eyelid while simulating lateralized chewing movements.
During the lateral movement of the mandible to the left, there was a clear elevation of the right eyelid (Figs. 1 and 2), mainly when the patient looked downward (ocular axis inclined down), as we may observe in Fig. 3. Eye closing was normal, even during mouth movements, that is, no synkinesia or it was compensated by the tonus of the palpebral orbicular muscle (Fig. 4). There was no history of heart arrhythmias during the patient's previous surgeries (cesarean sections). Pre- and intra-operative cardiac examinations were normal. The nose surgery was uneventful during the intra- and post-operative periods. There was no indication for correcting the mild palpebral ptosis and the patient said that during her lifetime she had been able to overcome and simulate normality of the Marcus Gunn phenomenon, having adapted herself conveniently, without any psychosocial discomfort, and therefore nothing was done in relation to the condition.

Fig. 1 - Patient opening eyes normally, with a slight difference in the right palpebral rim (smaller vertical axis) , revealing a mild palpebral ptosis.
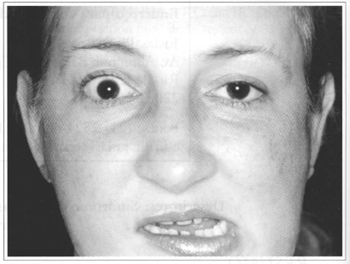
Fig. 2 - Patient with horizontal ocular axis, when moving mandible to the left; due to the action of the lateral pterygoid, the right upper eyelid rises synkinetically.
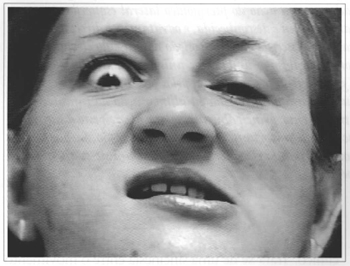
Fig. 3 - While moving the mandible with the ocular axis downwards, the patient exposes the sclera more clearly, making the synkinesia more noticeable.

Fig. 4 - With her eyes closed without effort and making mandible movements, the patient does not present synkinesia which is probably compensated for by the tonus of the orbicular palpebral muscle.
DISCUSSION
Although not very rare, the case presented deserves some comments, in that all congenital palpebral ptoses need to be assessed in terms of an existing Marcus Gunn phenomenon, which may significantly change the result of the palpebral ptosis correction, regardless of the severity or technique for correcting it. The synkinesia, itself does not have an adequate neurological correction, but can be improved through surgery by a partial resection of the eyelid levator or its transposition along with the correction of the ptosis (1,7,8,9). In severe ptoses, the most suitable surgical method seems to be the partial resection of the levator and suspension of the eyelid by the different techniques usually adopted, mainly suspension by aponeurotic or allogenic material grafting. Results may always be favorable, and the issue should be discussed in detail with the client. Inadequate treatment of the synkinesia of the palpebral levator in the post-operative period has been the most common demand cited by various authors. The best long-term results are around 64% of patients satisfied with surgery, when ptosis and synkinesia are corrected. Ptotic ou synkinetic lesions with a mild degree of esthetic or functional alteration should not be corrected, especially during childhood, because in most cases patients adapt very well to these conditions that may even improve with age. It is necessary to treat other coexisting eye lesions, sometimes as or more important than the ptosis or synkinesia.
FINAL COMMENTS
The case herein reported is that of a simple lesion, whose signs fortunately are restricted to a mild palpebral ptosis and clear pterygoid-palpebral synkinesia, duly controlled by the patient herself, without any major psychological or social discomfort. The synkinesia, in this case, was not accompanied by severe motor lesions (strabismus, severe ptosis or deficient movement of the eye), making any surgical intervention unnecessary, from our point of view.
REFERENCES
1. Blaydon SM. Marcus Gunn jaw-winking syndrome. Medicine Journ, 2001; vol. 2, 7.
2. Doucet TW, Crawford JG. The quantification, natural course and surgical results in Eyes with Marcus Gunn Syndrome. Am J Ophtalmol. 1981; 92(5):702-7.
3. Hwang JM, Park SH. A case of Marcus Gunn jawwinking and pseudo-inferior oblique overaction. Am J Ophtalmol; 2001; 131(1):.148-50.
4. Gunn RM. Congenital ptosis with peculiar associated movements of the affected lido Trans Ophtalmol Soc UK. 1883:3-283.
5. Freedman HL, Kushner BJ. Congenital ocular aberrant innervation - new concepts. J Pediatric Ophtalmol Strabismus. 1997; 34(1):10-6.
6. Kwik RS. Marcus Gunn syndrome associated with an unusual oculo-cardiac reflex Anaesresia. 1998; 35(1):46-9.
7. Bartkowisk SB, Zapala J, Wysynska-Pawelec G, Krzystkowa KM. Marcus Gunn jaw-winking phenomenon: management and results of treatment in 19 patients, J Craniomaxillofac Surg. 1999; 27(1):25-9.
8. Khwang SI, Tarbet KJ, Dortzbach RK, Lucarelli MJ. Management of moderate-to-severe Marcus Gunn jaw-winking ptosis. Ophtalmol. 1999; 106(6):1191-6.
9. Manners RM, Rosser p, Collin JR. Levator muscle transposition procedure: review of 35 cases. Eye. 1996; 10(5):539-44.
I - Plastic Surgeon, MD, Clínica de Otorrinolaringologia Prof. José Kós - Rio de Janeiro.
II - ENT Residents of Clínica Prof.José Kós.
Study performed at the Study Center of the Clínica Prof. José Kós.
Address for correspondence:
Josias Pires Ferreira, MD
Av.Almirante Barroso, 6 Cj. 1303
22031-001 - Rio de Janeiro - RJ Brazil
Phone: (55 21) 2524-6081 - Fax: (55 21) 2533-6516
e-mail: josias@cremerj.com.br


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter