

Case Report - Year 2016 - Volume 31 -
An original case of symmetric lipohypertrophy: case report and review of the literature
Caso original de lipo-hipertrofia simétrica: relato de caso e revisão de literatura
ABSTRACT
A middle-aged healthy woman who presented with longstanding history of slow growing masses located bilaterally and symmetrically on the upper and lower extremities closed to major joints. Imaging and pathology tests following excision of masses revealed normal subcutaneous fat. There was no evidence of well-circumscribed lipomas. A review of the literature identified a number of lipohypertrophic disorders, which may be present in a symmetrical fashion. The characteristics of the disorders, however, did not fully agree with characteristics observed in our patient. Although not absolute, the closest disease found to fit our case is a rare symmetrical lipodystrophy known as Madelung's disease. Of 150 reported cases, only 3 described involvement of lower extremities as seen in our case. We report a detailed description of a case, its management and post-operative follow-up. Different types of symmetrical lipodytrophies are also discussed.
Keywords: Lipodystrophy; Lipoma; Subcutaneous fat; Lipomatosis, multiple symmetrical; Lower extremity.
RESUMO
Paciente do sexo feminino, saudável, meia-idade e com história prolongada de massas com crescimento lento localizadas bilateralmente e simetricamente nos membros superiores e inferiores, próximas às principais articulações. Exames de imagem e patológicos após excisão das massas revelaram massas constituídas por gordura subcutânea normal. Não houve evidências de lipomas bem-circunscritos. Na revisão de literatura, destacaram-se diversos distúrbios lipo-hipertróficos, com possível apresentação simétrica. As características das afecções encontradas não eram, porém, totalmente concordantes com as características de nossa paciente. Embora não de modo absoluto, a doença que mais estreitamente se assemelhou ao caso foi lipodistrofia simétrica rara, conhecida como doença de Madelung. Dos 150 casos relatados, em apenas 3 foi descrito comprometimento dos membros inferiores, como ocorreu em nosso caso. Este relato apresenta descrição detalhada do caso, seu manejo e seguimento no pós-operatório. Os tipos distintos de lipodistrofias simétricas também são discutidos.
Palavras-chave: Lipodistrofia; Lipoma; Gordura subcutânea; Lipomatose; Simétrica múltipla; Membro inferior.
Lipodystrophy is a disturbance of fat metabolism1. Progressive lipodystrophy is a rare condition characterized by loss of subcutaneous fat from upper body that may be associated with fat hypertrophy below the waist. Some types of lipodystrophies present with gross buildup of fat in symmetrical regions of the body1. This report presents and describes the management of an original case of multiple symmetrical lipohypertrophies not consistent with any of symmetrical lipodystrophic disorders described in the literature so far.
CASE REPORT
Patient history
A 42-year-old, healthy, caucasian woman of Iraqi descent was admitted at our service with large subcutaneous masses, symmetrically located on upper and lower extremities that had been slowly and steadily growing over the past 14 years. She reported that masses appeared simultaneously, as opposed to the largest ones that appeared earlier. The masses became bothersome in appearance and hindering daily activities. Associated symptoms included a longstanding history of fatigue and weakness.
A significant factor of her past medical history is only a gastro-esophageal reflux disease controlled with daily dose of proton pump inhibitor. The patient denied smoking and consuming alcohol. Her family history revealed prevalence of type II diabetes mellitus, coronary artery disease as well as obesity. A full checkup was done few months earlier including thyroid function tests, lipid studies, fasting blood sugar and cortisol levels, which were all within normal limits.
Physical examination
The patient had body mass index of 41.6 and height of 1.51 cm. The mini-mental status assessment revealed normal cognitive functions. Masses were noted to be symmetric in both location and size, well circumscribed, firm and mobile with no overlying skin changes. The most prominent pair was located laterally over the proximal thigh with their maximal projection at the level of the hip joints (Figures 1 and 2).

Figure 1. Anterior view: Preoperative picture of the patient with symmetrical masses at the lateral aspect of the hip joints and the medial aspect of the knee joints.

Figure 2. Lateral view: Preoperative picture of the patient with a pair of superimposing masses at the lateral aspect of the hip joint.
The prominent bulges were physically deforming and estimated to be 26x12x14 cm. A second pair symmetrically located cephalad to the former masses was smaller and asymmetric in size measuring 8x7x7cm and 5x5x3 cm on the right and left sides, respectively. A third pair was located at the medial aspect of each knee measuring 10x6x4 cm on the right and 12x8x5 cm on left side (Figure 1). The last pair, was located at the level of the lateral epicondyles, and seemed have slightly less asymmetric in size 5x4x3cm and 4x3x3cm. The right elbow mass was the only one moderately tender to palpation.
The skin overlying all the masses appeared to have normal color and consistency compared to the rest of the patient's skin with no areas of fat reabsorption or surrounding edema. All extremities had normal strengths and sensory perception . There were no intra-abdominal masses on deep palpation and the liver span was normal.
Imaging
A magnetic resonance image of the hip and lower extremity was performed to determine the location and extent of involvement. The masses were noted to have ill-defined borders, localized in the subcutaneous fat sparing muscular structures. Edema was noted in the deep fat planes at the anterior aspect of the proximal thighs. The rest of the findings were insignificant except for an abnormal high signal in the left gluteus maximus tendon consistent with mild tendinopathy, and normally appearing bone marrow and joints (Figure 3).
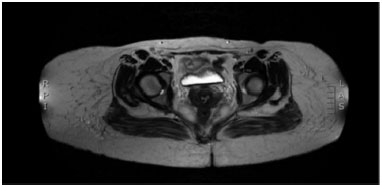
Figure 3. Magnetic resonance image of hip and lower extremity showing masses with ill-defined borders localized in the subcutaneous fat.
Surgical intervention
After discussing the risks and benefits of surgery with the patient, we decided to proceed with surgical excision in order to restore regular daily activity. Following infiltration with xylocaine with adrenaline, elliptical skin incisions on top of the masses were performed to access the subcutaneous tissues until identification of borders of the masses. The darker coloration and different tissue consistency of these masses were clearly discernible from the surrounding adipose tissue.
However, excision of the masses was tedious and time consuming due to the absence of dissection planes separating them from the surrounding healthy adipose tissue. The masses were multilobulated, adherent to the surrounding soft tissues and lacked a surrounding capsule. Despite the rich blood supply, there was no discernable dominant pedicle to any of masses. Most of the blood loss was from the deeper fascial attachment planes. The masses were completely resected from the fascial planes without involvement of any deep structures. One large Blake drain was inserted in each of the resultant soft tissue defects. A compressive garment was applied at the end of the procedure.
RESULTS
The postoperative course of the patient was uneventful with ambulation resumed on postoperative day one, patient was discharge with all drains on day 3, elbows and knees drains were removal on day 7 and thighs drains were removal with cessation of antibiotics on day 12.
At one-month follow up, seromas were found at the thighs surgical sites, which resolved in four weeks followed by serial drainages.
The patient was regularly seen with no recurrence of masses or seromas at 6 months follow-up.
Pathological findings on gross inspection revealed normal looking fat tissue distributed in lobules. Microscopic evaluation showed normal fat cells with normal cell size by subjective evaluation.
DISCUSSION
Lipohypertrophy and lipoatrophy constitute the two categories of lipodystrophies2. Although different in terms of etiologies and associations, these two may still coexist in some lipodystrophic disorders2.
Lipohypertrophic syndromes appeared to be low on the diagnostic scale because of the multiple comorbidities associated with them2,3. A relevant example known as Berardinelli-Seip syndrome, is a generalized lipodystrophy syndrome associated with acromegaloid features, muscular pseudohypertrophy, acanthosis nigricans and hepatomegaly, among many others3. Syndromes are usually recognized at birth, although diagnosis may be made later on childhood or puberty3.
Localized lipohypertrophy has been observed to be a complication of multiple insulin injections at the same site4. This is a more prevalent phenomenon among type I diabetics patients and can present as early as 2 years from initiating insulin treatment4.
Lipohypertrophy is a well-known complication in patients with acquired immunodeficiency syndrome (AIDS) who use high activity antiretroviral therapy (HAART)5,6. AIDS-associated lipohypertophies most commonly involve the posterior cervical fat, forming a buffalo hump, anterior cervical fat and breast tissues of both men and women6. These are also associated with insulin resistance and hyperlipidemia5.
Lipedema is a chronic disorder of fat metabolism that is presented, exclusively, in women7. It is characterized with symmetrical swelling of the lower extremities7. This is caused by symmetrical impairment of fatty tissue storage and metabolism resulting in evenly distributed nodes of subcutaneous tissue8.
The progression of lipidema can be divided into three stages. In the early stages, small subcutaneous nodules may be palpated8. The second stage is characterized by enlargement of these nodules that assume an uneven distribution with overlying orange peel-like skin8. In the most advanced stages, subcutaneous fat tissue projects outside the skin of the knees and thighs hindering mobility8. Edema in this disease is typically tender, sparing the ankles and feet, differentiating it from lymphedema7,8.
The projection of subcutaneous fat from the knees and thighs in our patient is concordant with lipedema, yet absence of the main diagnostic features of lipedema such as skin changes overlying the fat nodules and tender lower extremity swelling made it a less likely diagnosis.
Among the different reported lipodystrophy cases and their associations reported in the literature, the closest one to fit the clinical presentation of the patient in this report is multiple symmetrical lipomatosis (MSL), also known as Launois-Bensaude lipomatosis or Madelung's disease. It is a rare progressive disease characterized by large fatty accumulations9. Lesions are typically non-encapsulated lipomas that frequently penetrate the muscle fascia9. They are situated symmetrically at the neck, shoulders, supraclavicular, deltoid, abdomen, groin and buttock regions10.
Of 150 reported cases, only 3 had severe leg involvement9. The pathogenesis of this disease is unknown, however, it has been strongly linked to alcoholism, hepatic disturbances, reduced glucose tolerance, hyperlipoprotenemia, hyperuricemia, neuropathy, renal tubular acidosis and hypothyroidism9,10.
Our literature search failed to spot a case report of Madelung's disease that is not associated with any metabolic, endocrinological or neurological symptoms. In addition, most lipohypertrophies usually present with diffuse, non-circumscribed outgrowth of subcutaneous fat1, unlike the lipoma-shaped lesions found in our case. In MSL patients, fat cells from lipomatous tissue are smaller than normal adipocytes. This was discordant with the histological findings observed in this case. Furthermore, the natural history of Madelung's disease suggests high likelihood of lipohypertrophic recurrences; however, this was not the case of our patient at 6 month follow-up.
Whether post resection recurrence might occur at a later stage or it could be observed in the future.
CONCLUSION
The case we are presented does not completely fit into a specific lipohypertrophic disorder. However, although not absolute, the closest disease found to be concordant with our case is a rare symmetrical lipodystrophy known as Madelung's disease. Whether it is safe to categorize our case as a variant of Madelung's disease or it remains debatable.
COMPLIANCE WITH ETHICAL STANDARDS
Ethical standards were not violated in this article, since the patients' names were not mentioned and the pictures did not reveal the patients' identity.
REFERENCES
1. Clarkson P. Lipodystrophies. Plast Reconstr Surg. 1966;37(6):499-503. PMID: 5932410 DOI: http://dx.doi.org/10.1097/00006534-196606000-00004
2. Lacour M. Disorders of Fat tissues. In: Irvine AD, Hoeger PH, Yan AC, eds. Harper's Textbook of Pediatric Dermatology. Oxford: Wiley-Blackwell; 2011.
3. Pelosini C, Martinelli S, Bagattini B, Pucci E, Fierabracci P, Scartabelli G, et al. Description of an AGPAT2 pathologic allelic variant in a 54-year-old Caucasian woman with Berardinelli-Seip syndrome. Acta Diabetol. 2011;48(3):243-6. DOI: http://dx.doi.org/10.1007/s00592-011-0308-7
4. Omar MA, El-Kafoury AA, El-Araby RI. Lipohypertrophy in children and adolescents with type 1 diabetes and the associated factors. BMC Res Notes. 2011;4:290. DOI: http://dx.doi.org/10.1186/1756-0500-4-290
5. Singhania R, Kotler DP. Lipodystrophy in HIV patients: its challenges and management approaches. HIV AIDS (Auckl). 2011;3:135-43.
6. Caye N, Le Fourn B, Pannier M. Surgical treatment of facial lipoatrophy. Ann Chir Plast Esthet. 2003;48(1):2-12. DOI: http://dx.doi.org/10.1016/S0294-1260(02)00176-0
7. Taylor JR, Wilansky D. Symmetrical lipodystrophy with hypothyroidism. Ann Plast Surg. 1979;2(6):517-21. DOI: http://dx.doi.org/10.1097/00000637-197906000-00011
8. Hoehn RJ, Qazi HM. Benign symmetrical lipomatosis. Case report. Plast Reconstr Surg. 1976;58(5):626-30. PMID: 981407 DOI: http://dx.doi.org/10.1097/00006534-197611000-00023
9. Schuler FA 3rd, Graham JK, Horton CE. Benign symmetrical lipomatosis (Madelung's disease). Case report. Plast Reconstr Surg. 1976;57(5):662-5. PMID: 1273146
10. Capeau J, Magré J, Caron-Debarle M, Lagathu C, Antoine B, Béréziat V, et al. Human lipodystrophies: genetic and acquired diseases of adipose tissue. Endocr Dev. 2010;19:1-20. PMID: 20551664
American University of Beirut Medical Center, Beirut, Lebonon
Institution: American University of Beirut Medical Center, Beirut, Lebanon.
Corresponding author:
Nazareth Papazian
Mazraat Yachouh, Sami Bershan, Hbous
Beirut, Lebanon Zip Code 11072020
E-mail: nazareth.j.papazian@gmail.com
Article received: July 19, 2015.
Article accepted: October 8, 2015.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter