

Original Article - Year 2016 - Volume 31 -
What is the outcome 5 years after cervicoplasty?
O que muda no resultado de uma cervicoplastia 5 anos depois?
ABSTRACT
INTRODUCTION: An approach based on multiple anatomical structures and the use of different surgical strategies seems to achieve more lasting results in cervical rejuvenation surgery. Thus, extended cervicoplasty is an option with favorable results and low complication rates. However, little has been published regarding the durability of the results. This study aimed to objectively evaluate the long-term results obtained with extended cervicoplasty in difficult cases.
METHODS: Twenty patients, classified as having a "difficult neck," underwent extended cervicoplasty and were followed for 5 years. The results at 1- and 5-year post-operative follow-up were evaluated by eight plastic surgeons, using six objective criteria based on a theoretically ideal neck. The comparison of the results obtained at these time points was performed using a paired Student's t-test, with a level of significance of 5%.
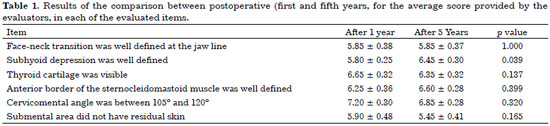
RESULTS: There was no significant difference in five of the six items evaluated (p-value ranging from 0.137 to 1.000), in the comparison between the first and fifth postoperative years. Subhyoid depression displayed a significantly better mean score in the fifth evaluation year than that observed in the first year after surgery (p = 0.039): from 5.80 ± 0.25 points (mean ± standard error of the mean) in the first year, to 6.45 ± 0.30 points in the fifth postoperative year.
CONCLUSION: Extended cervicoplasty is an important alternative in the treatment of the neck region, and even provides lasting results in difficult cases.
Keywords: Rhytidoplasty; Cervicoplasty; Neck muscles; Rejuvenation; Neck.
RESUMO
INTRODUÇÃO: A abordagem de múltiplas estruturas anatômicas e a utilização de diferentes estratégias cirúrgicas parece contribuir para a obtenção de resultados mais duradouros na cirurgia do rejuvenescimento cervical. Para isso, a cervicoplastia ampliada é uma opção com resultados agradáveis e baixos índices de complicações. A durabilidade dos resultados obtidos é, no entanto, pouco discutida na literatura. O objetivo desse estudo é avaliar objetivamente a manutenção dos resultados a longo prazo obtidos com a cervicoplastia ampliada aplicada em casos difíceis.
MÉTODOS: Vinte pacientes, classificadas como "pescoço difícil", foram submetidas à cervicoplastia ampliada e acompanhadas por 5 anos. Os resultados do pós-operatório de 1 e de 5 anos foram avaliados por oito cirurgiões plásticos, por meio de seis critérios objetivos vinculados a um teórico pescoço ideal. A comparação entre os resultados obtidos nestes momentos foi realizada por meio do teste t-student pareado, considerando um nível de significância de 5%.
RESULTADOS: Não houve diferença significativa em cinco dos seis itens avaliados (valor de p variando entre 0,137 a 1,000), na comparação entre o primeiro e o quinto ano de pós-operatório. A depressão subhioideia apresentou pontuação média na avaliação do quinto ano significativamente melhor do que aquela observada no primeiro ano após a cirurgia (p = 0,039), passando de 5,80 ± 0,25 pontos (média ± erro padrão da média) no primeiro ano, para 6,45 ± 0,30 pontos no quinto ano de pós-operatório.
CONCLUSÃO: A cervicoplastia ampliada se valida como alternativa importante no tratamento da região cervical mesmo em casos difíceis, proporcionando a obtenção de resultados duradouros.
Palavras-chave: Ritidoplastia; Cervicoplastia; Músculos do pescoço; Rejuvenescimento; Pescoço.
For more than 15 years, the authors have studied the available technical alternatives to obtain better results in cervical rejuvenation surgery1. The main focus has been on the search for strategies to minimize partial loss of cervicoplasty results over time, especially in those patients with severe tissue flaccidity2-4. In such cases, the durability of surgery is frequently questioned in the literature and in plastic surgery clinics1,5,6.
An approach based on multiple anatomical structures and the use of different surgical strategies seems to contribute to a more lasting result in facial surgery2,3,5-8. Thus, the authors have successfully applied a so-called extended cervicoplasty technique1.
The technique differs from the so-called conservative or minimally invasive procedures recommended by some authors for the treatment of the cervical region9-11. Extended cervicoplasty combines classic procedures described by different authors over the years, with broad cervical dissection, vigorous mobilization of deep tissues, resection of excess structures, and fixation of flaps in rigid structures2,3,12 -14.
The authors recommend the technique routinely, and especially for patients with a "difficult neck"4, classified as McKinney grade IV15, including those with excess skin sagging in the lower third of the face and very marked platysmal bands.
Using this technique, one can achieve agreeable cervical rejuvenation with safe, reliable, reproducible, and durable results16.
OBJECTIVE
The objective of this study was to present the experience of the authors with extended cervicoplasty performed in patients with a "difficult neck," with evaluation based on objective analysis, and discussion of the outcomes and long-term maintenance of the results.
METHODS
This study included all patients classified as McKinney grade IV15 who underwent extended cervicoplasty at the author's private clinic in Campo Grande, Mato Grosso do Sul, from January 2008 to August 2010.
Preoperative photographs taken by the same photographer are reproduced herein, and have similar image characteristics.
Surgery was performed according to classic techniques previously described by the authors1,16. With the patient sedated, anesthetic infiltration was performed in the cervical region with about 150 ml of a solution containing 0.125% lidocaine with adrenaline 1:200,000, followed by liposuction of the cervical region, based on the need in each case.
The submental sulcus was incised and the anterior neck region was dissected with Metzembaum scissors. The platysma muscles were easily identified, and were partially freed from the deep structures in the mid-cervical region using blunt dissection. In this manner, 2 muscular flaps with about 4 cm of extension were made. Subplatysmal fat, when present in excess, was exposed and resected.
The muscle flaps of the platysma were then approached in the midline with suture using single-layer monofilament 4-0 nylon, 5-9 cm long, from the submental incision to the proximity of the thyroid cartilage. The classic round lifting sequence recommended by Pitanguy17 was then performed. A large cervicofacial cutaneous flap was made; with the superficial musculoaponeurotic system exposed, an inverted "L" plication was initiated in the zygomaticofacial region and extended to the lateral cervical region, close to the sternocleidomastoid muscle. Cutaneous flap traction at the end of surgery contributed to the greater definition of the treated cervical region (Figures 1 to 3).
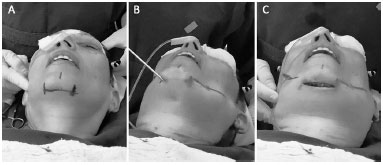
Figure 1. Intraoperative aspects; A: Marking of the submental incision; B: Wide liposuction of the cervical region; C: Incision and broad mid-cervical detachment.
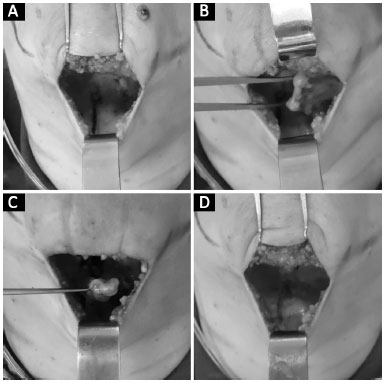
Figure 2. Intraoperative aspects - mid-cervical approach; A: Wide detachment and visualization of the medial edges of the platysma muscles (marked in blue in the detached area); B: Construction of left platysma muscle flap; C: Visualization of subplatysmal fat to be resected; D: Advancement and suturing of the two muscular flaps in the mid-cervical line.
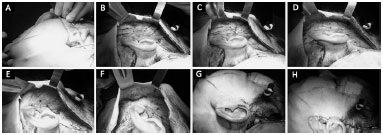
Figure 3. Intraoperative aspects - lateral cervical approach; A: Liposuction; B: Wide detachment and marking of the area to be plicated; C: Beginning of plication; D: Upper segment of plication completed; E: Lower segment of plication completed; F: Completion of plication; G: Cutaneous flap traction; H: Resection of excess skin.
In the postoperative period, the patients were initially followed weekly and then every 2 months. At 1 year, new photographic images (using the same views as those in the preoperative period) were taken. In the fifth postoperative year, the patients were contacted and underwent an evaluation. Patients who had undergone additional surgery in the middle or lower third of the face during this interval were excluded from the study, as were those who did not follow up. The others participated in a new photo session similar to the first.
The patients included in the study had their preoperative, and 1- and 5-year postoperative photos submitted for evaluation by eight plastic surgeons of the Brazilian Society of Plastic Surgery (SBCP).
The results of extended cervicoplasty were evaluated by a method based on the classical precepts of Ellenbogen & Karling18, which sought to identify an ideal cervical result in the postoperative period (Figure 4).
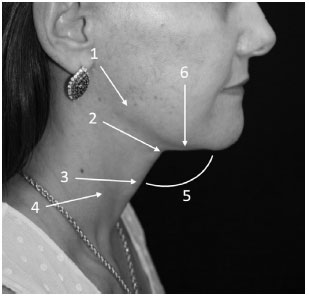
Figure 4. Aspects considered ideal in the analysis of the results of extended cervicoplasty 18; 1: Well defined face-neck transition in the jaw line; 2: Presence of well-marked subhyoid depression; 3: Visible thyroid cartilage; 4: Anterior border of the identifiable sternocleidomastoid muscle; 5: Cervicomental angle between 105º and 120º; and 6: Absence of residual skin in the submental region.
The 1- and 5-year postoperative photos were analyzed according to the following criteria: (1) well-defined face-to-neck transition at the jaw line; (2) presence of well-marked subhyoid depression; (3) visible thyroid cartilage; (4) identifiable anterior border of the sternocleidomastoid muscle; (5) cervicomental angle between 105º and 120º; and (6) absence of residual skin in the submental region (in profile view).
Each item identified as present was assigned one point. The sum of the points given by each surgeon was tabulated and submitted to statistical analysis. The comparison between the first and fifth postoperative years for the average score obtained in the evaluation of surgery was performed for each of the criteria with a paired Student's t-test. Statistical analysis was performed using the SigmaPlot statistical program, version 12.5, using a level of significance of 5%.
RESULTS
In the study period, 39 patients classified as McKinney grade IV15 underwent extended cervicoplasty. Of these, 19 (48.7%) were excluded from the analysis: 12 did not return for follow-up, 4 had undergone definitive filling in the lower 1/3 of the face in this period, and 3 had photos that were considered unsuitable for the analysis of all the items investigated by the plastic surgeon evaluators. All 20 patients included in the study were female, white, with a mean age of 57 ± 11 years.
The average duration of the surgical procedure was 202 ± 27 minutes. No difficulty was found in the preparation of the platysma muscle flaps, nor in the resection of the subplatysmal fat. All patients were discharged after about 24 hours of hospitalization.
Postoperative recovery was considered satisfactory, with 2 patients presenting mild and clinically resolved hematomas, 2 with small areas of partial necrosis of the upper retroauricular cutaneous flap, and 1 with temporary paralysis of the submandibular branch of the facial nerve. The remaining patients had an uneventful course.
The results of the comparison in the first and fifth years after surgery for the average score obtained in each of the items assessed are presented in Table 1. Regarding the item, "Subhyoid depression was well defined," The mean score in the fifth year assessment was significantly better than that observed in the first year after surgery (paired Student's t-test, p = 0.039), from 5.80 ± 0.25 points (mean ± standard error of mean) in the first year, to 6.45 ± 0.30 points in the fifth postoperative year.
On the other hand, there was no difference between the 2 analysis periods in relation to other items assessed (p value ranging from 0.137 to 1.000). These results are also presented in Figure 5.
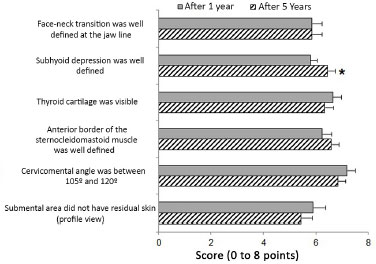
Figure 5. Graph showing the mean score in the evaluation of surgery, in each of the items evaluated. Each bar represents the mean and standard error of the mean. * Significant difference compared to one year after surgery (paired Student's t-test, p = 0.039).
The results are presented as mean ± standard error of the mean, or as a p-value in a paired Student's t-test.
Figures 6 and 7 present some of the treated patient photos in frontal view, and right and left profile; preoperative (top row), 1-year postoperative (middle row), and 5-year postoperative photos (bottom row).

Figure 6. Top figure: preoperative aspect patient A. Intermediate figure: 1-year postoperative aspect. Lower figure: 5-year postoperative aspect.

Figure 7. Upper figure: preoperative aspect patient B. Intermediate figure: 1-year postoperative aspect. Lower figure: 5-year postoperative aspect.
DISCUSSION
There is a consensus that the success of surgery for cervical rejuvenation involves achieving a natural and long-lasting result2,11. Extended cervicoplasty, a procedure widely used by Brazilian plastic surgeons for the integrated treatment of the lower third of the face, seeks to achieve this goal1.
The technique is practical, simple, and easily performed by surgeons who do less facial plastic surgery. It merges classical precepts advocated Millard et al.19, who validated wide cervical access and direct lipectomy through incision in the submental region; Connell20 and Feldman14, who demonstrated the importance of more aggressive and direct approaches in the platysma muscle; and Pitanguy17, who aimed for recovery of the natural anatomical position of the tissues through round lifting.
These precepts, safely used for years, provide the surgeon with the opportunity to achieve a more enduring result in facial plastic surgery, using a technique that both broadly and directly approaches the structure to be treated; the technique is able to mitigate opposing muscular forces precisely and effectively, and relocates and secures detached tissues in rigid and firm structures3,4.
Hence, extended cervicoplasty can directly treat the patient's chief complaint: sublymphatic lipodystrophy, flaccidity, ptosis of the platysma muscle, and cutaneous redundancy in the middle third of the face2,12. Less-reported deformities such as visible submandibular glands and bulging of the digastric muscle region are also indirectly well treated with this technique13. This indirect action minimizes the need for even more aggressive procedures with potentially more severe complications2,3,6,12,13.
In a recent study using a more subjective method for evaluating the results, the authors did not find a difference in classification of the outcomes obtained in the first and fifth postoperative years16. This finding prompted the present study, in which a more objective and timely analysis of characteristics considered ideal in the postoperative period were investigated, to determine whether there would be worsening of the results over time2,18.
Although this is an extended approach, the technique is safe and presents similar complication rates to those reported in the literature1,11,13. The complications described herein resemble those published by Destro et al.21 and Pita et al.3 and resolved satisfactorily, without sequelae. Major complications such as major hematomas, sialomas, and nerve lesions have not been reported6,13.
The authors have routinely performed this technique in all candidates for cervical rejuvenation. The variation is in the extent of surgery. In less pronounced cases, detachment, traction, and plication are less aggressive1.
In cases with severe tissue flaccidity, such as those presented here, the authors recommend the classic technique to achieve better outcomes, since a more conservative or minimally invasive approach seems to affect the short-term results, and increases patient dissatisfaction and reintervention rates3,5,10.
The evaluation of the long-term results of extended cervicoplasty has been investigated by the authors for years1. The definition of the durability of postoperative results is fundamental, so that extended cervicoplasty achieves elective status for difficult cases4. This is even more important when compared to the much less aggressive surgical strategies currently advocated by several authors5,10.
The analysis of the results presented herein showed that no significant differences were identified in 5 of the 6 items evaluated when comparing the results obtained in the first and fifth years, proving that the results of the extended cervicoplasty remained stable until the fifth postoperative year.
An exception in this case was the item "Subhyoid depression was well defined," which was statistically significant in the analysis, being more apparent in the fifth postoperative year. Thus, we believe that a desirable outcome, one of the main objectives of the technique, can be achieved, especially in the long-term postoperative period.
The late resolution of deep tissue edema and the progressive liposabsorption of the tissues treated by surgery, especially the submental fat, may have contributed to the greater definition of the region, improving the evaluation of this aspect in the fifth postoperative year.
The marked presence of a subhyoid depression greatly benefits the cervicomandibular angle, especially in the profile view, and is one of the most desirable aspects in the postoperative period for cervical surgery13. The improvement in the definition of subhyoid depression over time further enhances the technique used, improving its late results. We believe, however, that more studies are needed to accurately define the importance of the evolution of this particular aspect in extended cervicoplasty.
The results obtained in patients followed up for 5 years showed that extended cervicoplasty enables a lasting result that remains stable over the years, even in patients with a "difficult neck".
CONCLUSION
Extended cervicoplasty is reaffirmed as an alternative for the plastic surgeon interested in cervical rejuvenation of difficult cases, and provides lasting results.
COLLABORATIONS
DNS Analysis and/or interpretation of data; statistical analysis; final approval of the manuscript; conception and design of the study; performance of operations and/or experiments; drafting the manuscript or critical review of its contents.
KGA Final approval of the manuscript; conception and design of the study; performance of operations and/or experiments.
CAAB Final approval of the manuscript; conception and design of the study; performance of operations and/or experiments.
JIJ Final approval of the manuscript; conception and design of the study; completion of operations and/or experiments.
GEDO Drafting the manuscript or critical review of its contents.
MGM Drafting the manuscript or critical review of its contents.
BRMS Analysis and/or interpretation of data; statistical analysis; final approval of the manuscript; conception and design of the study; drafting of the manuscript or critical review of its contents.
LIB Analysis and/or interpretation of data; statistical analysis; conception and design of the study; drafting the manuscript or critical review of its contents.
REFERENCES
1. Nunes D, Ilgenfritz Jr J, Viana GP, Viana GAP, Almeida KG, Cury M, et al. Extended cervicoplasty for correction of cervical changes. Rev Bras Cir Plást. 2011;26(1):58-65.
2. Rohrich RJ, Rios JL, Smith PD, Gutowski KA. Neck rejuvenation revisited. Plast Reconstr Surg. 2006;118(5):1251-63.
3. Pita PCC, Azevedo SFD, Cabral PO, Melo SRPP. Gravitational cervical lifting. Rev Bras Cir Plast. 2010;25(2):291-6.
4. LaFerriere KA, Paik YS. Complete corset platysmaplasty: evolution of addressing the aging neck. Facial Plast Surg. 2014;30(4):431-7.
5. Abraham RF, DeFatta RJ, Williams EF 3rd. Thread-lift for facial rejuvenation: assessment of long-term results. Arch Facial Plast Surg. 2009;11(3):178-83.
6. Auersvald A, Auersvald LA. Innovative tactic in submandibular salivary gland partial resection. Plast Reconstr Surg Glob Open. 2015;2(12):e274.
7. Liu TS, Owsley JQ. Long-term results of face lift surgery: patient photographs compared with patient satisfaction ratings. Plast Reconstr Surg. 2012;129(1):253-62.
8. Letizio NA, Anger J, Baroudi R. Rhytidoplasties: cervicofacial SMAS-plasty according to vector suturing. Rev Bras Cir Plást. 2012;27(2):266-71.
9. Righesso R, Chem EM, Netto R, Martins ALM, Sartori N. Endoscopically assisted rhytidoplasty of the lower third of the face: the videoendoscopic corset. Rev Bras Cir Plást. 2014;29(3):328-36.
10. Daher JC, Ribeiro Júnior I, Esteves BP, Curado DMC, Lima RQ, Almeida CM, et al. Closed platysmotomy: a 7-year review. Rev Bras Cir Plást. 2015;30(3):403-7.
11. Jordan JR, Yellin S. Direct cervicoplasty. Facial Plast Surg. 2014;30(4):451-61.
12. Larson JD, Tierney WS, Ozturk CN, Zins JE. Defining the fat compartments in the neck: a cadaver study. Aesthet Surg J. 2014;34(4):499-506.
13. Mendelson BC, Tutino R. Submandibular Gland Reduction in Aesthetic Surgery of the Neck: Review of 112 Consecutive Cases. Plast Reconstr Surg. 2015;136(3):463-71.
14. Feldman JJ. Neck Lift my way: an update. Plast Reconstr Surg. 2014;134(6):1173-83.
15. McKinney P. The management of platysma bands. Plast Reconstr Surg. 1996;98(6):999-1006.
16. Silva DN, Rosseto M, Seno GZ, Meira ESB, Machado MG, Oguchi GED. Cervicoplastia Ampliada: avaliação dos resultados no quinto ano de pós-operatório. In: XXXI Congresso Brasileiro de Cirurgia. Curitiba; 2015 Ago 02-05; Curitiba, PR, Brasil.
17. Pitanguy I. The round-lifting technique. Facial Plast Surg. 2000;16(3):255-67.
18. Ellenbogen R, Karling JV. Visual criteria for success in restoring the youthful neck. Plast Reconstr Surg. 1980;66(6):826-37.
19. Millard DR, Pigott RW, Hedo A. Submandibular lipectomy. Plast Reconstr Surg. 1968;41(6):513-22.
20. Connell BF. Cervical lifts: the value of platysma muscle flaps. Ann Plast Surg. 1978;1(1):32-43.
21. Destro MWB, Destro C, Baroudi R. Pontos de adesão nas ritidoplastias: estudo comparativo. Rev Bras Cir Plást. 2013;28(1):55-8.
1. Universidade Federal de Mato Grosso do Sul, Campo Grande, MS, Brazil
2. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
3. Serviço de Cirurgia Plástica, Universidade Federal de Mato Grosso do Sul, Campo Grande, MS, Brazil
Institution: Universidade Federal de Mato Grosso do Sul, Campo Grande, MS, Brazil.
Corresponding author:
Daniel Nunes e Silva
Rua da Paz, 129 - Jardim dos Estados
Campo Grande, MS, Brazil Zip Code 79002-190
E-mail: dermatoeplastica@gmail.com
Article received: December 3, 2015.
Article accepted: October 3, 2016.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter