

Original Article - Year 2016 - Volume 31 -
Risk factors for infection in burn in children and adolescents: a cohort study
Fatores de risco para infecção em crianças e adolescentes com queimaduras: estudo de coorte
ABSTRACT
INTRODUCTION: Prevention of infection in burned patients poses great challenges such as infection, which constitutes the most common cause of mortality after burn injury. An analysis of burned patients younger than 20 years-old was performed prospectively to identify the incidence of nosocomial infection (NI) and risk factors for N. We included in the study those admitted and treated from January 2012 to December 2012 at a public burn unit in Brazil.
METHODS: A total of 136 patients admitted at Burn Care Unit during the study period fulfilled inclusion criteria. We collected information related to NI and epidemiological data.
RESULTS: Most patients were male (63.2%) and non-white (57.4%). Patients' mean age was 7.64 years. Scalding was the most frequent causal agent (45.6%). The mean body surface area (BSA) was 15.7%. Most of patients (80.9%) had two or more damaged areas. Surgical treatment with grafts was needed in 69 cases (50.7%). Infection was seen in 59 cases (43.4%), and sepsis in 27 (19.8%). Cultures were positive in 22.8%, and Staphylococcus aureus was the most frequent isolated agent (31.2%) found. Antimicrobial drugs were used in 45.6% of patients. The mean length of hospital stay was 22.36 days and mortality rate was 2.5%. According to the statistical analysis there was an association between infection and admission to the Intensive Care Unit (ICU), invasive procedures, grafts, length of hospital stay and BSA.
CONCLUSION: Risk factors for infection in burn patients are length of hospital stay, BSA, invasive procedures, admission at ICU and grafts.
Keywords: Burns; Infection; Child; Adolescent; Risk factors.
RESUMO
INTRODUÇÃO: A prevenção de infecções em pacientes queimados é grande desafio, pois trata-se da causa mais comum de mortalidade após queimaduras. Um estudo prospectivo em 136 pacientes queimados menores de 20 anos, internados e tratados entre janeiro e dezembro de 2012, foi realizado para identificar a incidência e fatores de risco para infecção hospitalar (IH).
MÉTODOS: Pacientes internados na Unidade de Tratamento de Queimados que aceitaram participar e preencheram os critérios de inclusão, participaram do estudo. Foram coletadas informações referentes à IH e dados epidemiológicos durante o período de internação.
RESULTADOS: Do total dos pacientes, a maioria era do gênero masculino (63,2%) e não branco (57,4%). A média de idade foi 7,64 anos. Escaldadura foi o agente causal mais frequente (45,6%). A média de superfície corporal queimada (SCQ) foi 15,7%. A maioria dos pacientes (80,9%) apresentou duas ou mais áreas acometidas por queimadura. O tratamento cirúrgico com enxertos foi necessário em 69 casos (50,7%). Ocorreu infecção em 59 pacientes (43,4%) e sepse em 27 (19,8%). As culturas foram positivas em 22,8% e Staphylococcus aureus foi o agente isolado mais frequente (31,2%). Antimicrobianos foram usados em 45,6% dos pacientes. O tempo médio de permanência hospitalar foi 22,36 dias e a taxa de mortalidade 2,5%. Houve associação entre infecção e admissão em Unidade de Terapia Intensiva (UTI), monitorização invasiva, enxertos, tempo de internação hospitalar e SCQ.
CONCLUSÃO: Os fatores de risco para infecção em queimaduras são: tempo de internação hospitalar, superfície corporal queimada, monitorização invasiva, internação em UTI e enxerto.
Palavras-chave: Queimaduras; Infecção; Criança; Adolescente; Fatores de risco.
The burn is considered one of the most devastating human injuries. Pediatric burns are an important cause of childhood morbidity that often result in scarring and changes in appearance with loss of function. The psychological impact is generally long-lasting for both child and family1.
Burns are among the leading external causes of death in Brazil, second only to other violent causes, such as traffic accidents and homicides. Burns are also among the most common childhood accidents - they are the fourth leading cause of death after traffic injuries, drowning and falls2.
Several epidemiological studies have pointed out that most burn victims are children. Data from the Brazilian Society of Burns show that approximately one million burn cases occur every year in Brazil, of which 200,000 are treated in emergency services, and 40,000 of these require hospital admission. In Brazil burns is a major health problem affecting people of all ages and both sexes3.
Infection is the most common cause of death following burn injury. Burn victims are obviously at high risk for nosocomial infection (NI) due to immunocompromising effects of burn injury, cutaneous and respiratory tract injury, long Intensive Care Unit (ICU) stays (which may involve endotracheal intubation and/or catheterization of blood vessels and bladder) and broad-spectrum of antibiotic therapy2. Therefore, Burn Care Units (BCU) can be the site of explosive and prolonged outbreaks caused by resistant organisms3.
OBJECTIVE
This prospective study described incidence of hospital infection, and associated risk factors in children and adolescents with burns.
METHODS
Design of the study
This is a prospective observational study developed from January to December 2012 at a Burn Care Unit (BCU) of the Hospital João XXIII in Belo Horizonte, Minas Gerais, Brazil. The management is conducted by an interdisciplinary team including plastic surgeons, pediatricians, intensive care physicians, physiotherapists, dietitian, nursing and social working professional.
Data were collected by researchers daily during patients' hospitalization. All burned patients under 20 years who agreed to participate were included in the study. The follow-up was performed until hospital discharge or death.
The study included 136 burned victims admitted to the BCU. Patients and legal guardians who refused to participate in the study and patients who already had infection upon admission were excluded from the study.
Inclusion criteria
We included all patients younger than 20 years who were admitted at BCU of the Hospital João XIII because of thermal, chemical and electrical burn during the year of 2012. Those patients approached by team of researches and who agreed to participate were included.
Exclusion criteria
Patients and accompanying person who refused to report to participate in the study and those who had infection at hospitalization were excluded from the study.
All patients had individualized records including age, sex, origin, comorbidities, image and laboratorial tests, surgical and pharmacological interventions. The Burn Surface Area (BSA) was clinically determined (Lund and Browder table), as well as depth of burn and airways injury based on historic data of each case and clinical findings. Burn cause was determined by history, by the use of standard categories: flame burns, scalds, electrical, chemical and contact with heated solid objects.
The study of nosocomial infections was carried out in all inpatients in 2012. Only signs and symptoms of infections from 72 hours or more after hospitalization were attributed to nosocomial infection. The study was conducted by review of patients' medical records, nursing medication records, microbiology and hematology laboratory data, and radiological exams (particularly chest X-rays). The criteria of communicable Diseases Center (CDC)4 for nosocomial infection (NI) were used for diagnosis of nosocomial infection, including those for burn wound infection (BWI).
Treatment of burned patients
According to practices at BCU, treatment of burned patients is made by early removal of necrosis tissue and application of antimicrobial topics on the wound, followed by closing with flaps when indicated, mainly autograft with available donor areas. Blood transfusion, use of nutritional support, isolating of routine of patients with indication, and control procedures of infection were used when necessary.
Skin flaps were performed early when indicated, and they were repeated until all burned areas of the body were treated (Figures 1, 2 and 3). Superficial burns and affecting partly the dermis, without indication of grafting, we covered with silver sulfadiazine and occlusive dressing.

Figure 1. Wound with granulation tissue.

Figure 2. Prepartion of the site to receive the graft.

Figure 3. Graft.
Statistical Analysis
The possible association of two variables was evaluated using the by chi-square test, and the Yates correction. We applied the Fisher exact test if one of the cells of the contingency tables contains an expected value less than 5, adopting the two-tailed p value. In a second step a multivariate analysis using binary logistic regression was performed. The binary logistic regression method was applied to identify variables that were independently associated with nosocomial infection. Only those variables that were associated with the event of interest by an univariate analysis (p < 0.25) were included in the initial binary logistic regression model. Then, using a backward elimination strategy, we included in the final model those variables that retained a significant independent association. Possible interactions among variables that remained in the final model.
Ethical issues
All patients and legal guardians who agreed to participate were included. After the explanations about the objectives, methods, risks and benefits of the study the responsible for the child or adolescent, besides the patient himself if older than seven years, signed the informed consent, according to Resolution 169/96 of the National Health Council, which describes rules on human research. It was fully explained that there would be no retaliation for those who refused to participate in the study. Our study protocol was approved by the Ethical Committee of the institution under the number 50/2012.
RESULTS
A total of 136 patients younger than 20 years were admitted and included in the study. Most of them were boys (63.2%) and non-white (57.4%). Patients' mean age was 7.64 years (2 months to 19 years). Most of them (51.5%) came from another cities of the state of São Paulo, and 22% from the capital of São Paulo.
The table 1 shows that most patients did not have comorbidities (86.8%) and no associated trauma (97.8%). Scalding was the most frequent causal agent (45.6%), 91.2% were accidental, and occurred at patients' home (91.2%). The most common place at patients' home was the kitchen (51%).
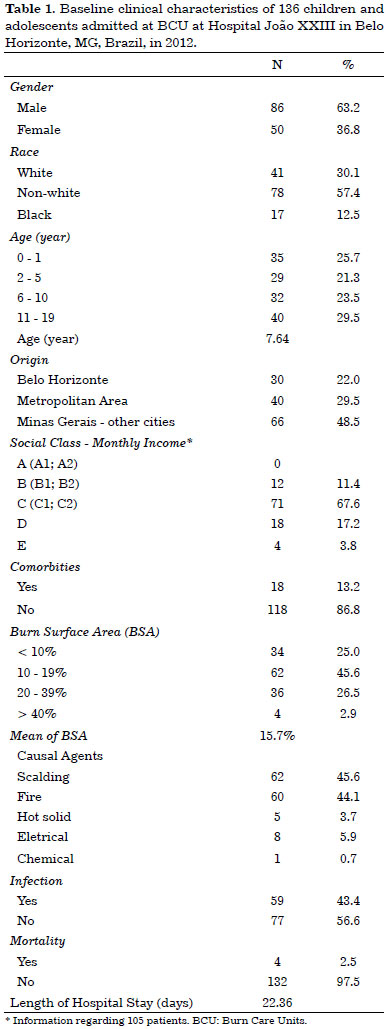
The mean TBSA was 15.7% (1% to 70%). Airway injury was diagnosed in 5.2% of patients. Most of them (80.9%) had two or more damaged areas. Surgical treatment with grafts was necessary in 69 cases (50.7%).
Table 2 shows that infection was seen in 59 cases (43.4%), and sepsis in 27 (19.8%). Infections included 31 (52.5%) on burned wound, 11 (18.6%) systemic infection, two pneumonias, two catheters related infection, one urinary tract infection, and 12 had more than one affected site. Cultures were positive in 22.8% of cases, and Staphylococcus aureus was the most frequent isolated agent (31.2%) followed by Pseudomonas aeruginosa (27.1%). Antimicrobial drugs were used in 45.6% of patients. The cefepime was the most used medication (41.8%). The mean time of antimicrobial drugs use was 12.9 days.
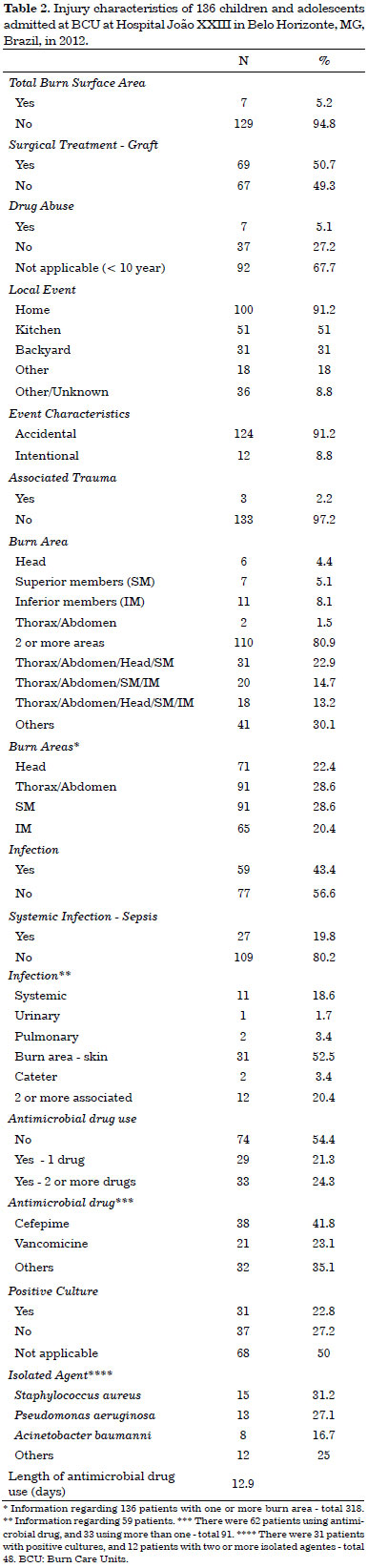
The mean length of hospital stay was 22.36 days (4 to 114 days) and mortality rate was 2.5%.
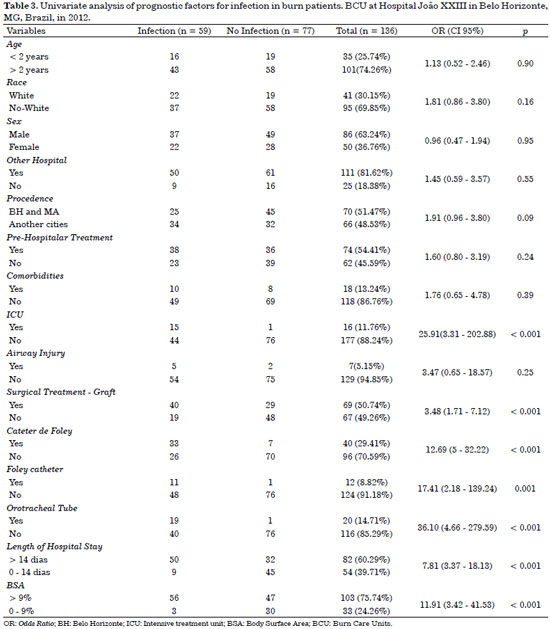
The univariate analyses of prognostic factors for infection in burned patients are described in Table 3. Age, race, gender, origin, pre-hospital treatment, comorbidities and airway injury were not independently significant in the development of nosocomial infection (p > 0,05). On the other hand, there was a strong association among variables related with invasive procedures such as central venous catheterization, urinary catheterization, endotracheal intubation and nosocomial infection.
There was also an association among infection and admission at burn ICU and length of hospital stay. Surgical treatments with grafts, length of hospital stay longer than 14 days and BSA greater than 10% were also significantly associated factors with nosocomial infection (p < 0,05) (Table 3).
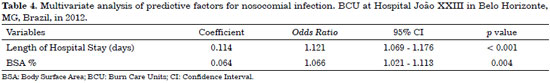
In a multivariate analysis, after adjustment by the binary regression logistic method, only two variables remained as independent predictors of nosocomial infection: length of hospital stay and BSA (Table 4).
DISCUSSION
Although eradication of infection in burn patients is impossible, a well conducted surveillance, infection control and prevention programs can help reduce its incidence. It is known that effective surveillance and infection control may reduce infection, mortality rates, length of hospital stay, and associated costs.
In this prospective cohort study, we report clinical features and outcomes of a non-selected group of pediatric patients admitted during 2012 at a highly specialized burn care unit. Our sample is similar to several published series of pediatric patients with burn injuries. Our surveillance showed a NI rate of 43.4% in the study population with predominance of burn wound infection (52.5%).
BWI was the most common infection according to Oncul et al.5 (56%) and in contrast to other reports in which there was a predominance of pneumonia6,7 and primary blood stream infection (BSI)7. The low incidence of BWI in Wurtz et al. 6 is in part attributed to routine early burn wound closure, which is not possible in our center due to the delay of patients' arriving from different areas.
High rates of NI were seen in burn patients admitted to burn intensive care unit, exceeding the published rates for surgical and medical intensive care units, which ranged from 15 to 50 per 100 admissions6.
Data from the National Nosocomial Infection Surveillance - NNIS - System8, from 1995 to 2000 involving nearly 800 ICU of which 17 were burn units, showed that BSI rates were higher in burn ICUs compared with others types of ICUs. In our study, the rate of BSI was 18.6% similar to two recent studies reporting 19.9%5 and 18.6%9.
The most frequently used invasive devices were urinary catheter whereas the least was the ventilator. The rate of NI related to invasive devices was higher in our study similar to rates found in the literature5,6,9, and for this reason, more strictly infection control procedures should be implemented.
In this study, similar to previous ones6,9,10, univariate analysis suggested the following risk factors for NI: admission in ICU with invasive measures (central venous catheterization, urinary catheterization, endotracheal intubation), length of hospital stay longer than 14 days, BSA greater than 10% and surgical treatment with grafts. However, after adjustment by regression logistic model, only two variables remained as independent predictors of NI: length of hospital stay and BSA.
It is important to notice that by multivariate analysis we can infer that each day of hospitalization added 12% risk of NI and each 1% of total body surface area increases about 7% in the risk of NI (table 4). This result is in agreement with the study of Oncul et al.10 that variables related to NI in logistic regression were BSA, comorbidities, broad spectrum antibiotic use and usage of invasive devices. Nevertheless, it should be pointed out that possibly the urinary indwelling catheter was a proxy marker for invasive procedures, since in the univariate analysis all these factors were strongly associated with NI.
Mozingo et al. 11 showed that bacteremia secondary to surgical debridement is related to size (> 45%) and duration of the burn injury (greater than 10 days old) and the prophylaxis is not needed for patients with small, acute burns. In our study, five patients without infection received prophylactic antimicrobial agents. The use of antimicrobial drugs in our BCU could be further restricted if prophylaxis was given only to immunocompromised patients or those with more severe injuries and longer cicatrization time.
Because of the risk of developing antibacterial resistance, some investigators suggested no antibiotic usage in burn patients during initial days12. An open wound that does not close within few days is likely to get infected at any time13. Topical antibiotics associated with wide debridement of dead tissue ensure the penetration of optimal concentration of the drug of viable tissue and minimize risk of infection.
In our study, S. aureus (31.2%) was the most prevalent microorganism on burn patients, followed by P. aeruginosa (27.1%), according to Oncul et al.5, and Winzer et al.6. Although enterococci have not been reported as a frequent cause of burn wound sepsis in the past, several recent studies have reported an increasing incidence of enterococcal bacteraemia in burn patients14. Similarly, studies of nosocomial infections have noted an increase in fungal isolates, particularly Candida species8.
Data from the National Nosocomial Infection Surveillance System indicated that the rate of nosocomial fungal infections was highest in burn and trauma wounds8. In our study, Candida was isolated in only one patient. S. aureus accounted for 31.2 per cent of isolates. The reason for the predominance of gram-positive pathogens may be the length of stay of our patients in the BICU.
Several studies have shown that the flora of individual burn wounds changes over time: gram-positive organisms are gradually replaced by gram-negative15. The average length of stay in our unit was 22.36 days. In addition, gram-negative bacilli, which were once common colonizers of burn wounds, and consequently common causes of nosocomial infections in burn patients, have become less common in recent years due to topical antibiotics and effective systemic antibiotics, particularly for Pseudomonas15. In our study, thirteen infections (27.2%) were attributable to Pseudomonas.
In 1992, a study with 537 (80 inpatients and 453 outpatients) burned children and adolescents conducted by Costa et al.16 in the same hospital , showed similar epidemiological profile: 59% males, aged under five years-old (36%) and 53% white, but most of them came from Belo Horizonte (70%), in contrast with our study that most patients came from a different area (22%). Most events occurred at patients' home, in kitchen (59%), by scalding (60%), which is similar to our results. The mean TBSA was 20%, similar to our results.
Sepse was present in 8% that was different from our study 27 (19.8%), which should be due to our center enlargement in recent years. Cultures were positive in 24%, and Staphylococcus aureus was the most frequent isolated agent16, similar to our study. The mean length of hospital stay was 30 days and the mortality rate was 4%16, which suggests an improvement in our hospital, since the median length of hospital stay was 22.36 days and the mortality rate was 2.5% in our study.
Over the last several decades, deaths due to infection in burn patients have decreased. Early surgical excision and closure, in our experience, has been an important factor in limiting burn wound infection. Our study suggests that infection control measures in invasive monitoring may protect patients as well as reduce length of hospital stay. The decrease in the severity of injuries, reduce of infection rates can be achieved through campaigns for accident prevention.
CONCLUSION
The results of our study indicated that risk factors for infection in burns are length of hospital stay, burned body surface, invasive monitoring, admission to ICU and grafts.
COLLABORATIONS
JSFL Contributed with elaboration of the study, statistical analyses and drafting of the manuscript. Principal author of the study.
EAO Contributed with elaboration of the study, statistical analyses and drafting of the manucript.
ACRAA Contributed with data collection and follow-up of patients included in the study.
MMO Contributed with data collection and follow-up of patients included in the study.
REFERENCES
1. Young AE. The management of severe burns in children. Curr Pediatr. 2004;14(3):202-7.
2. Aragão JA, Aragão MECS, Filgueira DM, Teixeira RMP, Reis FP. Epidemiologic study of burn injuries in children admitted to the Burn Unit of the Hospital de Urgência de Sergipe. Rev Bras Cir Plást. 2012;27(3):379-82.
3. Rossi LA, Barruffini RCP, Garcia TR, Chianca TCM. Quaimaduras: características dos casos tratados em um hospital escola em Ribeirão Preto (SP), Brasil. Rev Panam Salud Pública. 1998;4(6):401-4.
4. Greenhalgh DG, Saffle JR, Holmes JH 4th, Gamelli RL, Palmieri TL, Horton JW, et al.; American Burn Association Consensus Conference on Burn Sepsis and Infection Group. American Burn Association consensus conference to define sepsis and infection in burns. J Burn Care Res. 2007;28(6):776-90.
5. Oncul O, Ulkur E, Acar A, Turhan V, Yeniz E, Karacaer Z. Prospective analysis of nosocomial infections in a burn care unit, Turkey. Indian J Med Res. 2009;130(6):758-64.
6. Wurtz R, Karajovic M, Dacumos E, Jovanovic B, Hanumadass M. Nosocomial infections in a burn intensive care unit. Burns. 1995;21(3):181-4.
7. Taylor GD, Kibsey P, Kirkland T, Burroughs E, Tredget E. Predominance of staphylococcal organisms in infections occurring in a burns intensive care unit. Burns. 1992;18(4):332-5.
8. National Nosocomial Infections Surveillance System. National Nosocomial Infections Surveillance (NNIS) System Report, data summary from January 1992 to June 2002, issued August 2002. Am J Infect Control. 2002;30(8):458-75.
9. Santucci SG, Gobara S, Santos CR, Fontana C, Levin AS. Infections in a burn intensive care unit: experience of seven years. J Hosp Infect. 2003;53(1):6-13.
10. Oncul O, Yüksel F, Altunay H, Açikel C, Celiköz B, Cavuşlu S. The evaluation of nosocomial infection during 1-year-period in the burn unit of a training hospital in Istanbul, Turkey. Burns. 2002;28(8):738-44.
11. Mozingo DW, McManus AT, Kim SH, Pruitt BA Jr. Incidence of bacteremia after burn wound manipulation in the early postburn period. J Trauma. 1997;42(6):1006-10.
12. Ugburo AO, Atoyebi OA, Oyeneyin JO, Sowemimo GO. An evaluation of the role of systemic antibiotic prophylaxis in the control of burn wound infection at the Lagos University Teaching Hospital. Burns. 2004;30(10):43-8.
13. Kumar P. Prophylatic antibiotics in burns. Burns. 2006;32(5):655-6.
14. Jones WG, Barie PS, Yurt RW, Goodwin CW. Enterococcal burn sepsis. A highly lethal complication in severely burned patients. Arch Surg. 1986;121(6):649-53.
15. Manson WL, Pernot PC, Fidler V, Sauer EW, Klasen HJ. Colonization of burns and the duration of hospital stay of severely burned patients. J Hosp Infect. 1992;22(1):55-63.
16. Costa DM, Abrantes MM, Lamounier JA, Lemos ATO. Estudo descritivo de queimaduras em crianças e adolescentes. J Pediatr (Rio J.). 1999;75(3):181-6.
1. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
2. Universidade Federal de Ouro Preto, Ouro Preto, MG, Brazil
3. Universidade Federal Minas Gerais, Belo Horizonte, MG, Brazil
4. Santa Casa de Misericórdia de Ouro Preto, Ouro Preto, MG, Brazil
5. Programa de Iniciação Científica, Belo Horizonte, MG, Brazil
Institution: Universidade Federal Minas Gerais, Belo Horizonte, MG, Brazil.
Corresponding author:
Joyce de Sousa Fiorini Lima
Rua Três, 611-101 - Lagoa
Ouro Preto, MG, Brazil Zip Code 35400-000
E-mail: joycefiorini@gmail.com
Article received: June 9, 2015.
Article accepted: September 29, 2015.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter