

Articles - Year 2003 - Volume 18 -
Modified Vertical Abdominoplasty in Formerly Obese Patients
Abdominoplastia Vertical Modificada em Pacientes Ex-Obesos
ABSTRACT
Modified vertical abdominoplasty was peiformed on 19 patients at our Service - Clínica Privada e Hospital Municipal de Ipanema - in the last two years, in which we observed a decrease in the incidence of complications and operative time, and better esthetic results with the classical and lateral abdominal excess treatment. The technique consists of a combined vertical and horizontal incision with a single block resection, without plicature of the aponeurosis of the rectus abdominis and without drainage.
Keywords: Abdominoplasty; formerly-obese; single block; without plicature; without drainage
RESUMO
Foram submetidos a abdominoplastia vertical modificada 19 pacientes nos últimos 2 anos em nosso Serviço - Clínica Privada e Hospital Municipal de Ipanema -, sendo observada diminuição da incidência de complicações, do tempo operatório e melhor resultado estético com tratamento dos excessos abdominais clássicos e laterais. A técnica consiste de incisão combinada vertical e horizontal com ressecção em monobloco, sem plicatura da aponeurose dos retos abdominais e sem drenagem.
Palavras-chave: Abdominoplastia; ex-obesos; monobloco; sem plicatura; sem drenagem
The increase in the number of obese patients submitted to reduction gastroplasty has led to the emergence of a new type of patient for abdominoplasty - with a lot of abdominal and flank flaccidity, and freguently with a previous estethetically inadequate vertical scar, associated ar not with an incisional hernia (Figs. 5 and 6).
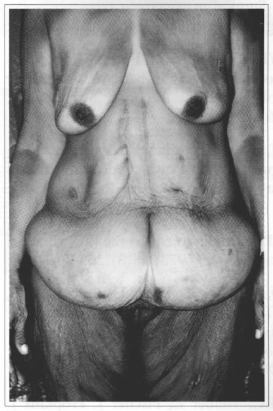
Fig. 5 - Preoperative; front view. Presence of a large excess of vertical and lateral abdominal skin, with previous poor quality scars.
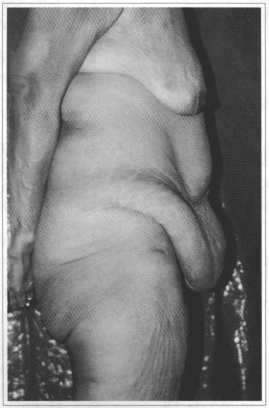
Fig. 6 - Preoperative; lateral view. Note the presence of a large excess of vertical and lateral abdominal skin, with supra-umbilical bulging due to the incisional hernia.
The literature review revealed that in these cases, abdominoplasty combined with a vertical resection of the abdominal skin has already been performed by Joffe(1), Matory et al. (2) and Hart et al. (3), who published 15 cases in which they used the Regnault incision (4) combined with a vertical incision, overlapping a previous gastroplasty scar and peri-umbilical skin.
Sensöz et al.(5) and Hughes et al. (6) recommend treating the incisional hernia associated with the abdominoplasty.
The minimum waiting period of 2 years after reduction gastroplasty in order to perform abdominoplasty that was recommended by Zook(7), Savage(8) and Hart(3) has currently been reduced to 18 months in our Service.
The modified vertical abdominoplasty (MVA) was initially developed for patients with a previous vertical scar, in whom we also performed more detaching and vacuum drainage. We gradually developed marking without detaching the abdominal flap and along with a single block resection without drainage.
MATERIAL AND METHOD
Nineteen formerly obese patients, with an average age of 40 years and body mass index (BMI) ranging between 25 and 40, with or without incisional hernia, and with or without a vertical abdominal scar, were submitted to MVA.
All horizontal and vertical skin excesswas marked and removed previously in a single block. No detachment for anaining proximity at the median line, plicature or drainage is performed.
Technique: Marking is performed with the patient standing, in an anatomical position, and the median line is drawn frorn the xiphoid process to the pubic symphysis, observing the centralization of the umbilicus. A bidigital maneuver verifies all lateral skin excess in relation to this vertical line. The maximum point in lateral distance from the medial line is 10 to 12 cm. The horizontal skin excess is marked as in a classical abdominoplasty. The points of intersection of the ellipses are calied A, B (supra-umbilical) and C (suprapubic) (Fig.l).
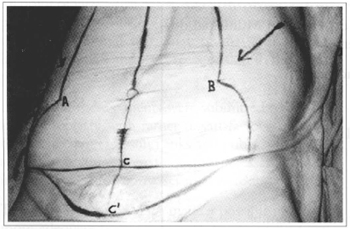
Fig. 1 - Preoperative drawing. Points A and B should be extended to point C without tension and to point C' in cases where there is flaccidity of the pubis.
All excess tissue above the supraumbilical line is drawn as a triangle, leaving points A and B in the direction of the xiphoid pracess with a slight arch forming an angle of 30° at the apex of the triangle (Fig. 1).
When the patient has excess of skin in the pubic region, we mark the C' point, 4 to 6 cm below the C point (Fig. 1). In the supine position, after anesthetic induction (general or epidural) and decontamination of the patient, marks are checked so that all excess tissue may be removed safely.
Points A and B should be taken to the suprapubic region without tension, using a bi-digital maneuver.
The whole drawn line is infiltrated with a solution of 100 ml of 0.9% saline and 1/200,000 adrenalin.
The whole tissue is marked and resected in a single block with suecessive hemostasia and maintenance of the umbilical pedicle.
Neither plicature of the rectus abdominis nor drainage is performed. The hernias found are treated.
The borders of the flaps with the A and B points are pulled downwards and medially toward the direction of the C point (Fig. 2) and sutured (Fig. 3); marking is performed with repositioning of the umbilicus, closure of the vertical and transversal incisions in 3 planes (Fig. 4), and the deepest plane is fixed to the aponeurosis.
Dressing is semicompressive.
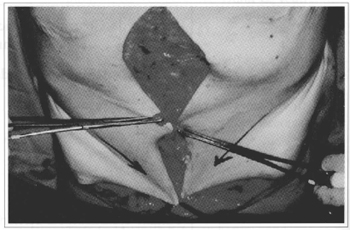
Fig. 2 - Inferior-medial traction of points A and B toward point C, a maneuver performed without tension.
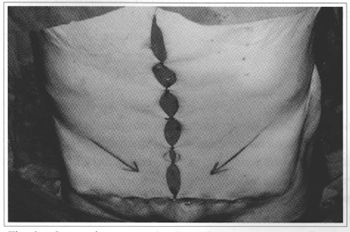
Fig. 3 - Suture of points A and B to C; marking of the flap of the new umbilical site.
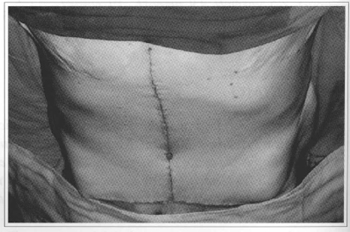
Fig. 4 - Suture in 3 planes and repositioning of the umbilical scar.
RESULTS
We observed two cases of seroma that developed well.
Two patients had to be submitted to a neoumbilicoplasty due to inadeguate irrigation of the umbilical scar after dissection of the hernial pouch, and an adeguate esthetical result was reached.
We were able to treat lateral abdominal and pubic excesses whenever present and decrease the transversal scar, without needing further surgical procedures to correct them.
DISCUSSION
The ideal patient has undergone gastroplasty at least 18 months earlier; is stable from the weight and clinical point of view(3,7,8); has an adequate psychosomatic profile and a BMI below 40; may or may not have a vertical abdominal scar; may or may not have an incisional hernia; and has excess of skin in flanks and pubis (Figs. 5 and 6).
In the past, these patients were submitted to classical abdominoplasty with rather unsatisfactory results in relation to skin excess in flanks and pubis, and further surgical procedures were freguently necessary; a higher incidence of postoperative seromas were also observed.
The development of MVA made it possible to attain a more adeguate body contour (Figs. 7 and 8). Complications decreased (9,10,11) because of the absence of detachments and a shorter surgical time, and new procedures to treat the remaining excesses became unnecessary. All this has led to reduction in costs and more satisfied patients.
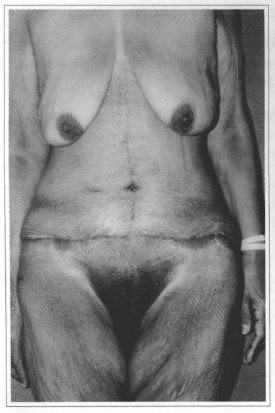
Fig. 7 - Postoperative; front view. There was a significant improvement of the body contour, by treating lateral and medial excesses and repositioning the pubic region.
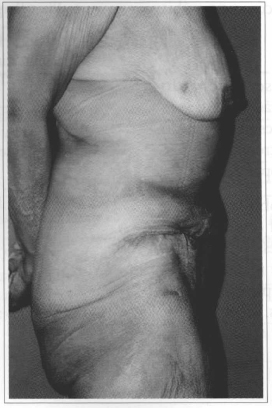
Fig. 8 - Postoperarive; lateral view. Significant improvemenr of the body contour, with the treatment of vertical and lateral excesses and repositioning of the pubic region.
CONCLUSION
MVA is easy to perform, attains an adequate aesthetic result and a lower rate of complications, although it has the disadvantage of a vertical scar in those cases where there is no previous scar.
REFERENCES
1. Joffe SN. Surgical management of morbid obesity - Pragress report. Gut. 1981; 22(3):242-54.
2. Matory WE Jr, O' Sullivan J, Fudem G, Dunn R. Abdominoplasty surgery in pacients with severe morbid obesity, Plast Recanstr Surg. 1994; 94(7) :976-87.
3. Hart NB, Voundarrargian V, Zoystom CMS. Abdominoplasty following vertical banded gastraplasty for morbid obesiry Br J Plast Surg. 1995; 48 (6):423-27.
4. Regnault P. Abdominoplasty by the W Technique. Plast Reconstr Surg. 1975; 55(3):265-74.
5. Sensöz O, Arifoglu K, Kocer U, Celebioglu S, YaziciA, Tellioglu AT, et al. A new appraach for the treatament of recurrent large abdominal hernias: The overlap flap. Plast Reconstr Surg. 1997; 99(7) :2074-8.
6. Hughes KC, Weider L, Fischer J, Hopkins J, Antonetti A, Manders EK, DW111E. Ventral hernia repair with simultaneous panniculectomy. Am Surg 1996; 62(8):678-81.
7. Zook EG. The massive weigth loss pacient. Clin Plast Surg. 1975; 2(3):457-66.
8. Savage RC. Abdominoplasty following gastrointestinal bypass surgery. Plast Reconstr Surg. 1983; 71(4):500-7.
9. Grazer FM, Goldwyn RM. Abdominoplasty assessed by survey, with emphasis on complications. Plast Reconstr Surg. 1977; 59(4):513-7.
10. Floras C, Davis PKB. Complications and long-term results following abdominoplasty: A retrospective study Br J Plast Surg. 1991; 44 (3):190-4.
11. Vartine VL, Morgan RF, Williams GS, Gumper TJ, Drake DB, Knox LK, Lin KY. Wound complications of abdominoplasty in obese patients. Ann Plast Surg. 1999; 42(1):34-9.
I - Member of the Brazilian Society of Plastic Surgery, Chief Medical Resident of the Medical Residency of the Plastic Surgery Service of Hospital de Ipanema.
II - Candidate Member to the Brazilian Society of Plastic Surgery, Medical Resident of the Plastic Surgery Service of Hospital de Ipanema.
III - Member of and Specialist by the Brazilian Society of Plastic Surgery, Former Medical Resident of the Plastic Surgery Service of Hospital de Ipanema.
IV - Member of the Brazilian Society of Plastic Surgery, Chief Medical Resident of the Medical Residency and Head of the Plastic Surgery Service of Hospital de Ipanema.
Serviço de Cirurgia Plástica do Hospital Municipal de Ipanema
Address for correspondence:
Luiz Fernando da Costa, MD
Rua Visconde de Caravelas, 21
22710-030 - Rio de Janeiro - RJ Brazil
Phone / Fax: (55 21) 2266-3537
e-mail: cplastica@luizfernandodacosta.com.br


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter