

Case Report - Year 2016 - Volume 31 -
Surgical item left in the abdomen six years after abdominoplasty: case report
Corpo estranho retido cirurgicamente em abdômen seis anos após abdominoplastia: relato de caso
ABSTRACT
The retained surgical item in patients after closure of the wound is a situation that although rare is preventable and requires specific care such as institutional protocols for prevention. We report a case of removal of an already encapsulated pads by fibrin tissue (textiloma) from a patient six years after an abdominoplasty, which formed a palpable mass in her abdomen. The retained surgical items lead to variable symptoms such as palpable masses, compressions, non-absorptive loss and, sometimes, severe complications. The diversity of manifestations combined with their few frequency, most of the times, lead to underdiagnosis. Treatment should be individualized for each case, although in case of symptoms removal is indicated in most cases. Surgical removal is associated with complications as longer as objects remain in patient's body.
Keywords: Foreign bodies; Seroma; Abdominoplasty; Surgical instruments; Surgical sponges.
RESUMO
A permanência de corpos estranhos em pacientes após o fechamento da ferida operatória é uma situação que, embora rara, é evitável e demanda cuidados específicos como protocolos institucionais de prevenção. O caso relata a retirada de uma compressa já encapsulada por tecido de fibrina (textiloma) de uma paciente seis anos após abdominoplastia, formando uma massa palpável em seu abdômen. A permanência desses itens cirúrgicos leva a sintomas variáveis como massas palpáveis, compressões, síndromes disabsortivas e, algumas vezes, graves complicações. A diversidade de manifestações combinada a sua pouca frequência levam, muitas vezes, ao subdiagnóstico. O tratamento deve ser individualizado para cada caso, embora na presença de sintomas a retirada é indicada na grande maioria das vezes. A cirurgia de retirada está mais associada a complicações quanto maior tempo de permanência dos objetos no corpo do paciente.
Palavras-chave: Corpos estranhos; Seroma; Abdominoplastia; Instrumentos cirúrgicos; Tampões de gaze cirúrgicos.
Description of retained foreign body is rare in medicine. Currently, we use the term retained surgical items to designate gauze, instruments or tools accidentally left in the patient after closure of the wound, thus distinguishing them from objects that may be found in patients before the surgery, such as shrapnel.
The period for discovery of these objects in the patient varies, and most of them form a textiloma, characterized by the formation of fibrin capsule surrounding the retained material, as seen in the description of our case. Although uncommon, strategies must be approach and conscientious efforts made to reduce the proportion of these cases considering their legal and medical implications.
CASE REPORT
A 57-year-old patient (FGS) who underwent abdominoplasty at a hospital in the countryside 9 years before with a non-expert physician. The case developed, at the time, by appearance of large volume seromas, which were systematically punctured by the responsible physician. No records of imaging exam from that time. Seroma evolved with new sporadic recurrences and it was solved by the own patient who learned how to empty the seroma at home with needle and syringe.
Approximately two years ago, the patient noticed a lump bulging in the abdomen that was painless and without inflammation signs (Figure 1). The patient sought a plastic surgeon, who requested an abdominal wall ultrasound that showed a heterogeneous collection of approximately 1.5 liters. No foreign body was described.

Figure 1. Bulging in lower abdomen.
The patient was re-operated on after perform pre-operative tests, and we found plenty of encapsulated yellow fluid with the presence of gruns and debris without characteristic odor and a softened black mass on the bottom of the capsule (Figure 2). The total emptying of seroma and capsulectomy was performed (Figure 3). All material removed was sent to pathology department for analysis and the seroma was forwarded to cytological, culture and biochemical analyses.

Figure 2. Softened and dark mass in the bottom of the capsule.
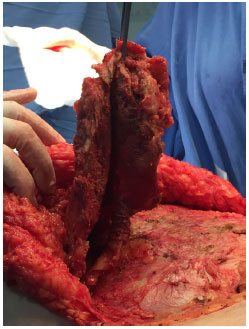
Figure 3. Removal of the mass.
A number of adhesion points and placement of Portovac drain for 5 days were carried out. Because there were no signs of infection in activity that was performed antibiotic prophylaxis for 48 h.
The pathology report showed fibrotic capsules with formation of granulation tissue and inflammation subacute multifocal inflammation and analysis of the liquid showed presence of rare cocci, and inflammatory features.
The patient is with 14 months postoperatively and showed complete resolution of bulging. There was no seroma recurrence.
DISCUSSION
The retained surgical item in patients after closure of the wound is rare1, preventable and requires specific care and institutional protocols for prevention. Among retained objects most common are cotton products (gauzes and swabs), corresponding to about 70% of cases2,3.
The most affected locations are abdominal and thoracic cavities3. There are also cases in which there was migration of the foreign body through a fistula created by the adjacent inflammatory process, and such object migrate, for example, from the abdominal cavity for subcutaneous and hollow viscera (which is retained) or organs of the gastrointestinal tract surrounding, which are eliminated with stools3,4.
When there retention of gauze and cotton pads there is formation of the so gossypibomas or textilomas. From these formations we can have two possible situations: 1. exudative inflammatory process with abscess formation (usually with early diagnosis and removal); and 2. Gossypiboma remains inert in the body, forming a fibrotic process and circumscribed mass3,5.
The patient's clinical feature varies according to the location of the foreign body and it may develop acutely, subacute or no symptoms. Its diagnosis is made, on average, 21 days after surgery2. The patient may present symptoms due to compression, obstruction, malabsorption syndrome, or bacterial growth. In addition, other non-specific symptoms can occur such as palpable tumor, nausea, vomiting, hematuria, urinary urgency, dysuria, pyuria, oliguria, anorexia, anemia and weighting loss4,5.
Among risk factors for postoperative retention are emergency procedures (risk nine times higher than in elective procedures), changes in the course of the surgery (complications - risk four times higher), and high body mass index (obese patients)2,3.
Once a surgically retained item is observed in the patient, symptoms should be sought, and if the patient reports any symptom, it must be removed1,5. In a multicenter review, the time for removal of the object was two days after surgery4,5.
However, the longer the item remains, the surgery is higher associated with difficultness and greater rate of complications. Therefore, asymptomatic patients and who have retained items for long time an observational management should be employed. The preferred approach to the abdominal region is laparotomy, but the use of laparoscopy has also been described in some cases5,6.
Strategies to reduce the incidence of these events are still little effective given the cost-effectiveness os procedures such as postoperative radiographs or instruments with electromagnetic sensors. Undoubtedly, best prevention is to increase awareness and improve communication between teams, especially during counting of gauzes1,6.
In 2015 the Nurses Association of Operating Room to improve and prevent episodes of retained surgical items created an updated recommendations of preventive practices, and these recommendations became gold standards in the U.S. concerning counting policies. Recommendations prioritize counting: before beginning the procedure, whenever new items are added to the sterile field, before closure of cavity within a cavity (such as uterus) and counting in the end of closure of the skin or procedure being counted audibly and checked by two individuals. In hospitals where the technique was employed, 97% of them had no retained surgical sponge for a period of one year7.
COLLABORATIONS
ANB Drafting of manuscript or critical review of its content.
GJSF Analysis and/or interpretation of data, drafting the manuscript, and critical review of the content.
EF Analysis and/or interpretation of data.
VAB Analysis and/or interpretation of data.
AMPJ Analysis and/or interpretation of data, drafting the manuscript, critical review of the content.
NSJ Analysis and/or interpretation of data.
REFERENCES
1. Williams RG, Bragg DG, Nelson JA. Gossypiboma--the problem of the retained surgical sponge. Radiology. 1978;129(2):323-6.
2. Gawande AA, Studdert DM, Orav EJ, Brennan TA, Zinner MJ. Risk factors for retained instruments and sponges after surgery. N Engl J Med. 2003;348(3):229-35.
3. Cima RR, Kollengode A, Garnatz J, Storsveen A, Weisbrod C, Deschamps C. Incidence and characteristics of potential and actual retained foreign object events in surgical patients. J Am Coll Surg. 2008;207(1):80-7.
4. Guner A, Hos G, Kahraman I, Kece C. Transabdominal migration of retained surgical sponge. Case Rep Med. 2012;2012:249859.
5. Singh R, Mathur RK, Patidar S, Tapkire R. Gossypiboma: its laparoscopic diagnosis and removal. Surg Laparosc Endosc Percutan Tech. 2004;14(5):304-5.
6. Gibbs VC, Coakley FD, Reines HD. Preventable errors in the operating room: retained foreign bodies after surgery-Part I. Curr Probl Surg. 2007;44(5):281-337.
7. Association of periOperative Registered Nurses (AORN). Guidelines for prevention of retained surgical items. In: Guidelines for Perioperative Practice. Denver: AORN; 2015. p. 347-63.
1. Universidade do Extremo Sul Catarinense, Criciúma, SC, Brazil
2. Hospital Brigadeiro, São Paulo, SP, Brazil
Institution: Universidade do Extremo Sul Catarinense, Criciúma, SC, Brazil.
Corresponding author:
Amanda Nunes Borges
Rua Santos Guglielmi, 230 - Mina Brasil
Criciúma, SC, Brazil Zip Code 88811-231
E-mail: amandanunes101@hotmail.com
Article received: August 8, 2016.
Article accepted: October 30, 2016.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter