

Case Report - Year 2016 - Volume 31 -
Complex reconstruction of the perineal and gluteal regions after resection of a large squamocellular carcinoma of the anal margin: a case report
Reconstrução complexa de regiões glútea e perineal após ressecção de extenso carcinoma escamocelular de borda anal: relato de caso
ABSTRACT
Perineal and gluteal regions may be affected by a wide spectrum of diseases, and the treatment may require extensive surgery and cause functional, aesthetic, and psychosocial damages at various levels. Wounds in the extensive perineal and gluteal regions after surgical treatment of neoplasia may represent a challenge in local reconstruction. Size, location, and availability of tissue around the lesion may hinder wound primary closure, requiring the use of one or more flaps. This article reports a case of reconstruction of the perineal and gluteal regions after oncological resection at the plastic surgery service of the Hospital das Clínicas at the Federal University of Minas Gerais. The muscle and fasciocutaneous flaps of the gluteus maximus and myocutaneous of the semimembranosus were used.
Keywords: Squamous cell carcinoma; Anal neoplasia; Surgical flaps; Reconstructive surgical procedures; Perineum.
RESUMO
As regiões glútea e perineal podem ser afetadas por um variado espectro de doenças, cujo tratamento pode demandar extensas mutilações e acarretar em prejuízo funcional, estético e psicossocial em variados graus. Feridas extensas da região perineal e glútea após o tratamento cirúrgico de neoplasias podem representar um desafio para a reconstrução local. Tamanho, localização e disponibilidade de tecido em torno da lesão são fatores que podem impedir o seu fechamento primário, tornando necessário o uso de um ou mais retalhos. Este artigo relata um caso de reconstrução de períneo e região glútea após ressecção oncológica, no serviço de Cirurgia Plástica do Hospital das Clínicas da Universidade Federal de Minas Gerais (UFMG). Foram utilizados os retalhos muscular e fasciocutâneo de glúteo máximo e miocutâneo de semimembranoso.
Palavras-chave: Carcinoma de células escamosas; Neoplasias do ânus; Retalhos cirúrgicos; Procedimentos cirúrgicos reconstrutivos; Períneo.
The perineal and gluteal regions may be affected by a wide spectrum of diseases, and treatment may require extensive surgery that results in functional, aesthetic, and psychosocial damages at various levels. Primary reconstruction favors lower morbidity and recovery time; however, the extent of lesions and/or resections do not often allow this type of closure. Thus, in-depth knowledge about the various possibilities of local reconstruction is important1,2.
Surgical treatments of malignant neoplasia in this region often involves extensive resection of the skin, subcutaneous tissue, muscle, vessels, nerves, and pelvic organ segments, which makes the closure of the generated damage extremely challenging3.
OBJECTIVE
This work aimed to expose and discuss a case of reconstruction of the perineal and gluteal regions after oncological resection at the plastic surgery service of the Hospital das Clínicas, Federal University of Minas Gerais (HC-UFMG), Belo Horizonte, MG.
CASE REPORT
Patient GCF, a 53-year-old man, who had a squamous cell carcinoma (SCC) of the anal margin, including the perineal, perianal, and gluteal regions (Figure 1), underwent abdominoperineal amputation of the rectus by the coloproctology team at the HC-UFMG and extended resection with extirpation of soft parts of about 80% of the left gluteus and 30% of the right gluteus, as well as parts of the gluteal muscle and pelvic floor (Figure 2).

Figure 1. Squamous cell carcinoma of the anal canal with involvement of the gluteal region.
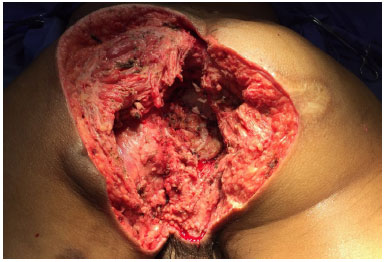
Figure 2. Extended oncological resection.
At its deepest point, the resection reached the pelvic cavity, with exposure of the pelvic organs. Such defect was closed by positioning a bovine pericardium implant and overlapping the left gluteus maximus muscle flap (Figures 3 and 4).
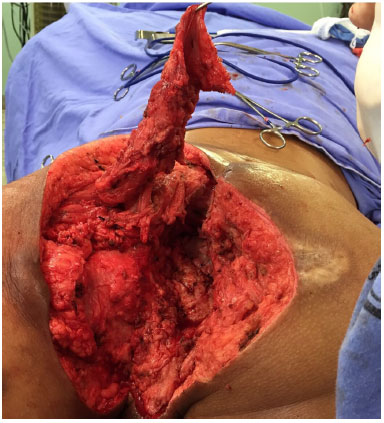
Figure 3. Positioned bovine pericardium and muscle flap of the maximus gluteus highlighted.

Figure 4. Positioned muscle flap.
The remaining defect was reconstructed with a VY advancement myocutaneous flap of the left semimembranosus and rotation of the right gluteus fasciocutaneous flap, followed by positioning of the drainage in a vacuum-sealed system (Figures 5 and 6).
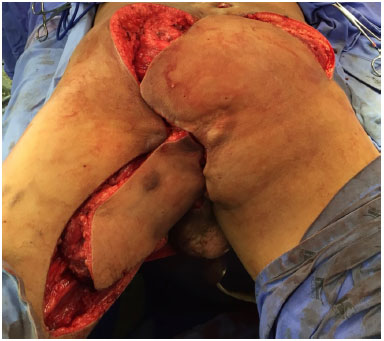
Figure 5. Positioned locoregional flaps.

Figure 6. Final aspect at the immediate postoperative period.
The patient showed good postoperative progression. In the fifth postoperative day (POD), the patient presented a small dehiscence in the confluence point of the three flaps. The dehiscence stopped its progression, reaching a maximum dimension of 4 cm, being treated in a conservative way, without requiring new surgical procedures such as closure by secondary intention (Figure 7).

Figure 7. Area of local dehiscence.
The drainage was maintained until the outflow was < 50 ml during 24 hours of serous secretion (10th POD). The patient was monitored postoperatively by nursing, physiotherapy, psychology, coloproctology, and plastic surgery teams.
During hospitalization, the patient presented with an obstructive acute abdomen caused by a band, with a new intervention performed by the coloproctology team, which increased the hospitalization time. The patient was discharge from the hospital on the 25th day he was judged as clinically well, with satisfactory tolerance to ambulation and without important pain complaints.
Currently, the patient is undergoing outpatient monitoring at the clinical oncology, coloproctology, and plastic surgery services, and the reconstructive surgical treatment showed good results (Figure 8).
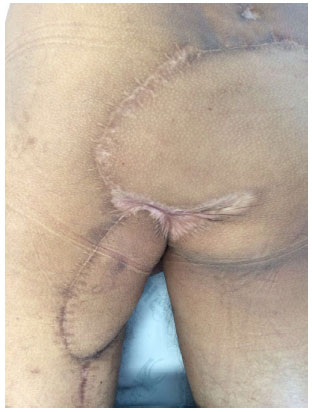
Figure 8. Final aspect at the time of return to ambulation.
DISCUSSION
The surgical treatment of SCC of the anal margin includes abdominoperineal resection, often performed together with neoadjuvant chemotherapy. The attempts to conduct primary closure of perineal wounds frequently result in complications4 due to the following: suture under tension, great dead pelvic space caused by oncological resection, field contamination, and poor-quality perineal skin already previously irradiated1.
The conventional abdominoperineal amputation comprises extirpation of the anal canal, anal sphincter, pelvic floor muscle, and portion of the rectus, and an extension depends on tumor dimensions and stipulated safety margin1,4.
In the present case, owing to the spread of the tumor to the gluteal region, particularly in the right part, the resulting defect was considerably greater than expected by conventional surgery, generating a great area of dead space at the bottom of the pelvic region and in the sacral area. Extensive resections such as the one described herein generally require local and regional flaps for closure.
A wide range of reconstruction options, from local flaps to free flaps, are available for reconstructing the gluteal-perineal region in literature. To cover such defects, the most universally used options include the vertical rectus abdominis myocutaneous (VRAM) flap, gracilis myocutaneous flap, rotation and gluteus advancement flap, or the myocutaneous and fasciocutaneous flaps from the posterior thigh region1.
The gluteus maximus muscle flap such as the one used to close the pelvic aperture as described herein is considered a safe to use because of its vascularization via two dominant pedicles, the lower and upper gluteus vessels (type III by the Mathes and Nahai classification).
This flap is technically easy to manufacture and used mainly to cover posterior perineal defects but can be extended to also reach anterior defects. However, the gluteus maximus flap requires a prone position and, generally, needs to be bilateral in extensive reconstructions5,6.
The myocutaneous flap of the semimembranosus, which was used to cover most of the perineum and lower portion of the gluteal region in the present patient, also had this same type of vascularization (type III), which justifies its efficacy. The left gluteus fasciocutaneous flap, used for the reconstruction of most of the gluteal region, was obtained and randomly fixed in rotation and, in the present case, did not present signs of failure6-8.
In reconstructions that use multiple flaps, the greatest tension point generally coincides with the point at which all the flaps join and may often occur in the center of the wound. This factor, associated with the debilitated nutritional state in which the patient was found, which is typical of oncological patients, was considered the main cause of the partial dehiscence observed2,6-8.
Complex reconstructions after extensive tumor resections are always a great challenge in plastic surgery. Defects in the perineal and gluteal regions result in morbidity, as they affect the motor, intestinal, urinary, and sexual functions at various levels.
Thorough knowledge of the anatomy, distribution, and physiology of locoregional flaps of this region is of utmost importance so that even in extensive resections, patients may have the perspective that they have received satisfactory reconstruction and rehabilitation.
COLLABORATIONS
WFFJ Writing the manuscript or critical review of its content.
BRB Writing the manuscript or critical review of its content.
TASS Writing the manuscript or critical review of its content.
HXMC Writing the manuscript or critical review of its content.
FN Writing the manuscript or critical review of its content.
PRC Analysis and/or interpretation of data and final approval of the manuscript.
REFERENCES
1. Wang ED, Conkling N, Xu X, Chern H, Finlayson E, Varma MG, et al. Perineal flap reconstruction following oncologic anorectal extirpation: an outcomes assessment. Plast Reconstr Surg. 2015;135(1):176e-84e.
2. Frasson M, Flor-Lorente B, Carreño O. Reconstruction techniques after extralevator abdominoperineal rectal excision or pelvic exenteration: meshes, plasties and flaps. Cir Esp. 2014;92 Suppl 1:48-57.
3. Inglin RA, Eberli D, Brügger LE, Sulser T, Williams NS, Candinas D. Current aspects and future prospects of total anorectal reconstruction-a critical and comprehensive review of the literature. Int J Colorectal Dis. 2015;30(3):293-302.
4. Blumetti J, Bastawrous AL. Epidermoid cancers of the anal canal: current treatment. Clin Colon Rectal Surg. 2009;22(2):77-83.
5. Mughal M, Baker RJ, Muneer A, Mosahebi A. Reconstruction of perineal defects. Ann R Coll Surg Engl. 2013;95(8):539-44.
6. Blondeel PN, Hallock GG, Morris SF, Neligan PC, eds. Perforator Flaps: Anatomy, Technique & Clinical Applications. 2nd ed. St Louis: CRC Press; 2013.
7. Pantelides NM, Davies RJ, Fearnhead NS, Malata CM. The gluteal fold flap: a versatile option for perineal reconstruction following anorectal cancer resection. J Plast Reconstr Aesthet Surg. 2013;66(6):812-20.
8. Mughal M, Baker RJ, Muneer A, Mosahebi A. Reconstruction of perineal defects. Ann R Coll Surg Engl. 2013;95(8):539-44.
1. Hospital das Clínicas da Universidade Federal de Minas Gerais, Belo Horizonte, MG, Brazil
2. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
Institution: Serviço de Cirurgia Plástica do Hospital das Clínicas da Universidade Federal de Minais Gerais, Belo Horizonte, MG, Brazil.
Corresponding author:
Walter Ferraz Flávio Júnior
Av. Professor Alfredo Balena, 189, sala 807 - Santa Efigênia
Belo Horizonte, MG, Brazil Zip Code 30130-100
E-mail: walter_ferraz@yahoo.com.br
Article received: July 16, 2016.
Article accepted: October 30, 2016.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter