

Original Article - Year 2017 - Volume 32 -
Efficacy of structured and conventional techniques on aesthetic and corrective rhinoplasty
Eficácia das técnicas estruturada e convencional na abordagem estética e reparadora do nariz
ABSTRACT
INTRODUCTION: Rhinoplasty, like other plastic surgery subspecialties, has greatly evolved in recent decades, as both a surgical technique and a diagnosis of the alterations that need to be performed. The objective of the current study was to evaluate the efficacy of the structured and conventional surgical techniques on nasal aesthetic and corrective approaches.
METHODS: A total of 49 patients, who underwent surgical operation by the author of this work, were retrospectively studied. The patient generally underwent one of the two surgical techniques. The efficacy of each technique was evaluated by means of the critique provided by the patients and the surgeon regarding the results, and the ability to reach the pre-operative goals.
RESULTS: Both techniques were efficient in attaining the final objective of the surgery. Patient and surgeon satisfaction were similar in both cases, and there were no major complications in any of the groups.
CONCLUSION: The present work showed that both the structured and the conventional techniques were efficient in the treatment of nasal alterations. The most important factor for selecting the best approach in each case was the correct pre-operative diagnosis of the required alterations.
Keywords: Rhinoplasty; Nasal cartilages; Nose; Costal cartilage.
RESUMO
INTRODUÇÃO: A rinoplastia, como outras subespecialidades da Cirurgia Plástica, apresentou evolução muito grande nas últimas décadas, tanto em termos de técnica operatória quanto em diagnóstico das alterações a serem tratadas. O objetivo deste trabalho é avaliar a eficácia das técnicas Estruturada e Convencional na abordagem estética e reparadora do nariz.
MÉTODOS: Foram estudados de forma retrospectiva 49 pacientes operados pelo autor do trabalho, que foram submetidos a uma das duas técnicas operatórias. A eficácia das técnicas foi avaliada a partir da crítica dos pacientes e do cirurgião com relação aos resultados e à capacidade de se chegar ao objetivo do pré-operatório.
RESULTADOS: Ambas as técnicas se mostraram eficazes para alcançar o objetivo final da cirurgia. A satisfação dos pacientes e do cirurgião foram semelhantes nos dois casos, e não houve complicações maiores em nenhum dos grupos.
CONCLUSÃO: O trabalho mostrou que tanto a técnica Estruturada quanto a Convencional são eficazes para o tratamento das alterações nasais, sendo o mais importante o correto diagnóstico pré-operatório das alterações para a escolha da melhor abordagem em cada caso.
Palavras-chave: Rinoplastia; Cartilagens nasais; Nariz; Cartilagem costal.
In the plastic surgery field, rhinoplasty is particularly important since the nose plays a crucial role in respiration and represents the central aesthetic with relevance to the harmony of the face. Thus, knowledge of nasal anatomy, its peculiarities, and the manner in which its structures are inter-related is fundamental for surgical success1,2.
Rhinoplasty experienced an important evolution in recent decades, with a radical change of concepts and paradigms. The approach to the nasal structure was initially performed from a philosophy of reduction, which involved, performing cartilage resections and narrowing the nasal bone base, by means of a closed technique. The long-term results, both functional as well as aesthetic, were limited and difficult to solve, as a consequence of scar contraction and a lack of support. Patients who underwent resection of the lateral branch of the alar cartilage, for example, would develop alar retraction and tip pinching, weakening of the lateral wall, and nasal valve collapse3,4.
With the evolution of nasal surgery, the original anatomy became more valued, and more easily accessed and understood due to the open rhinoplasty technique. The new approach was more focused on repositioning and restructuring existing tissue4. Depending on the surgeon's preference and training, cartilage grafting is more or less utilized, with respect to the uniqueness of each case.
A satisfactory rhinoplasty result, both aesthetic and corrective, depends on the final satisfaction of the patient, regardless of the technique used5. The present study aimed to evaluate the efficacy of two current surgical techniques in the treatment of nasal alterations, based on the experience of a single surgeon.
OBJECTIVE
To evaluate the efficacy of structured and conventional techniques on aesthetic and corrective rhinoplasty.
METHODS
The present study is clinical, primary, retrospective, and interventional. The author evaluated questionnaires and standardized pictures of patients who underwent rhinoplasty using either the structured or conventional technique. The efficacy of the techniques was evaluated based on the subjective critique from the patients, as well as the surgeon, regarding the results, both from an aesthetic and functional point of view, and the ability of reaching the expected goals.
The work was performed following the principles of the Declaration of Helsinki, which was revised in 2000, and the 196/96 Resolution of the National Health Council. Patients signed a Free and Informed Consent Form before each surgery.
The subjects were patients from the surgeon's private clinic, the ambulatory care unit of the Dr. Arthur Ribeiro de Saboya Hospital, and the São Paulo Hospital, in São Paulo, SP, where the surgeon works.
Inclusion criteria were patients who underwent rhinoplasty, using the structured or conventional technique, for aesthetic or corrective reasons, between March 2013 and June 2015. All procedures were performed by the same surgeon. There was no discrimination regarding the patients' gender, age, and anthropometric data.
Exclusion criteria included patients who were not operated on by the author of this study or who had not undergone nasal surgery by means of the aforementioned techniques.
The technique used on each patient was personalized, and based on a preoperative plan of facial analysis and diagnosis of deficiencies with the respective required treatment. The conventional technique was selected when the patient did not require a lot of grafting, presented with cartilage of good quality and support capacity, did not require complex structural modifications, and were not victims of traumas. The structured technique, on the other hand, was used on patients requiring extensive grafting, complex laterorhinia, and a reinforced structure to sustain the nasal tip or expand the airway.
The sample cohort included 49 patients who met the inclusion criteria, and were operated on consecutively. Of these, 29 (59%) and 20 (40%) patients underwent structured and conventional rhinoplasty, respectively. A total of 8 (16%) patients were from the surgeon's private clinic, 34 (69%) patients were from the São Paulo Hospital, and 7 (15%) patients were from the Dr. Arthur Ribeiro de Saboya Hospital ambulatory care unit.
Procedures
The patients underwent rhinoplasty in the surgical center under general anesthesia. The surgical team was comprised of at least two plastic surgeons and the anesthesiologist.
Following general anesthesia, antiseptic, and aseptic procedures, the patients received local infiltration with an anesthetic and vasoconstrictor solution at a ratio of 1:100,000 units, containing lidocaine, epinephrine, and 0.9% physiological saline. The nasal vibrissae were then trimmed using a number 15 blade scalpel, while waiting for the effect of the anesthetic solution.
In all open technique surgeries, the columellar incision was performed using a stepwise approach, followed by internal bilateral incisions in the caudal margins of the alar cartilages. After lifting the skin and exposing the bone and cartilage structures of the nose, the treatment was executed in a systematic way, always in the cranial-caudal direction.
When necessary, the grafts were preferentially constructed from the septal cartilage. If the septal cartilage had been previously used or was insufficient, then it was constructed from rib cartilage, which when required, was removed through a 3 to 5 cm incision in the thorax, followed by sectional dissection until the sixth or seventh rib, of which about 3 cm were removed.
After the removal, the Valsalva maneuver was always performed to detect eventual lesions to the visceral pleura. The thorax incision was closed in layers, and all drainage tubes removed. The grafts were constructed using a scalpel blade, with measures appropriate to each type of function and maintained in 0.9% physiological saline until being used. When the rib cartilage was used, the procedure required careful monitoring of the grafts, given its tendency to distort. Excessively distorted grafts were discarded.
The grafts were secured onto their destined locations using PDS 5-0 sutures, with the exception of the columellar strut, which was attached to the nasal spine using 4-0 nylon. The septal mucosa was approximated using vycril 5-0. The internal incisions were closed using vycril 5-0, while the columellar incision were closed using 6-0 nylon. No nasal splints were used. Tampons were inserted when there was excessive bleeding and removed after 24 h.
The bandage was created using micropore paper tape over the nasal bridge and tip, and aquaplast when fractures were performed. The aquaplast and the columellar suture were removed within 5 to 7 days, and the bandage replaced within 5 to 7 days, and then up to 2 weeks following the operation. The patients were instructed to keep their heads elevated during the first two weeks, and to clean the nose with 0.9% physiological saline during the first week. The patients received 1 g of cefazolin during the operation, 500 mg of cephalexin every 6 hours for a period of one week, nonsteroidal anti-inflammatory drugs for 3 days, and pain medication according to the intensity of pain. They were also instructed to rest for 30 days.
The patients were released from the hospital 6-12 hours after completion of the procedure. Patients underwent post-operative follow-up 5 days, 12 days, 1 month, 3 months, 6 months, and 12 months after the procedure, and annually thereafter to evaluate the results. Photographic evidence to evaluate the results was collected during follow-up.
RESULTS
A total of 49 rhinoplasty surgeries were performed; 9 (18%), 31 (63%), and 9 (18%) patients underwent the procedure in 2013, 2014, and until June 2015, respectively. In the entire cohort, only two (4%) surgeries were performed using the closed technique. In nine (18%) surgeries there was joint participation of otorhinolaryngologists for specific functional treatment input.
The patient cohort, comprised of 30 (61%) women and 19 (39%) men, had a mean age of 31 years (range: 17-46 years). A total of 12 (25%) patients received corrective rhinoplasty (Figures 1-12) while 37 (75%) patients received aesthetic rhinoplasty (Figures 13-20). Primary surgery was performed on 41 patients (83%), while 8 (17%) patients underwent secondary surgery.

Figure 1. Corrective rhinoplasty: pre-operative frontal photograph.
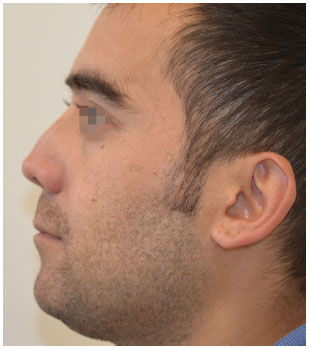
Figure 2. Corrective rhinoplasty: pre-operative left profile.

Figure 3. Corrective rhinoplasty: pre-operative right profile.
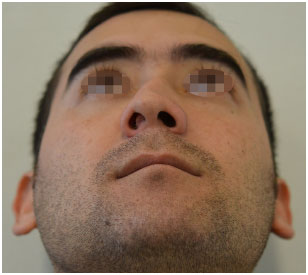
Figure 4. Corrective rhinoplasty: pre-operative basal photograph.
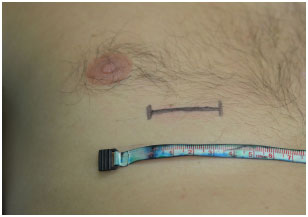
Figure 5. Structured corrective rhinoplasty: markings for rib cartilage removal.
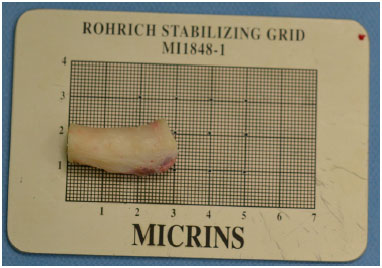
Figure 6. Structured rhinoplasty: rib cartilage for grafting.
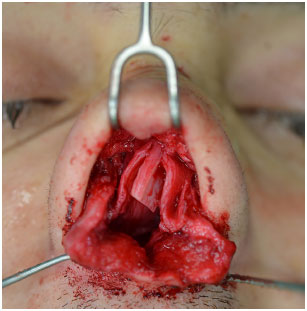
Figure 7. Corrective rhinoplasty: intra-operative after removal of the deviated septum.

Figure 8. Structured rhinoplasty: assembly of the "L Strut" cartilage structure.

Figure 9. Corrective rhinoplasty: frontal view. One month post-operative.

Figure 10. Corrective rhinoplasty: left profile. One month post-operative.

Figure 11. Corrective rhinoplasty: right profile. One month post-operative.
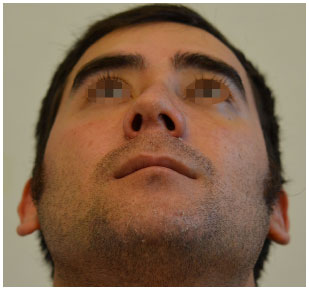
Figure 12. Corrective rhinoplasty: basal view. One month post-operative.

Figure 13. Aesthetic rhinoplasty: frontal view. Pre-operative.

Figure 14. Aesthetic rhinoplasty: left profile. Pre-operative.

Figure 15. Aesthetic rhinoplasty: right profile. Pre-operative.
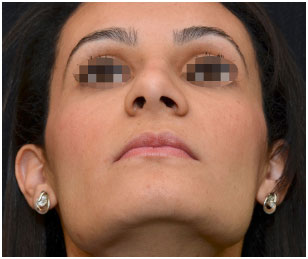
Figure 16. Aesthetic rhinoplasty: basal view. Pre-operative.

Figure 17. Aesthetic rhinoplasty: frontal view. One year post-operative.

Figure 18. Aesthetic rhinoplasty: left profile. One year post-operative.

Figure 19. Aesthetic rhinoplasty: right profile. One year post-operative.

Figure 20. Aesthetic rhinoplasty: basal view. One year post-operative.
The structured technique was used for all corrective surgeries. Of the aesthetic surgeries, 55% were done using the conventional technique, while 45% were performed using the structured technique. Two (4%) patients, who both underwent the structured technique, received oral treatment for the nasal septum depressor muscle. Nasal osteotomies were performed on 21 (72%) patients who underwent structured rhinoplasty, and 15 (75%) patients on whom conventional rhinoplasty was performed.
Of the 49 patients, 6 (12%) patients were followed for over 1 year post-operatively. Further, 11 (23%), 16 (33%), 8 (16%), and 8 (16%) patients were followed up to 1 year, 6 months, 3 months, and 1 month, respectively, after surgery.
Complications presented by the patients, regardless of the follow-up period, were as follows: return of the nasal bone base to the original pre-osteotomy point, lateral osteotomy with a high final aspect, partial re-occurrence of droopy nasal tip, skin retraction at the soft triangle, nostril asymmetry, partial recurrence of airway obstruction, bone callus formation following fracture. Of the 12 patients who underwent corrective surgeries, 5 (41%) patients presented with severe laterorhinia, and maintained some degree of residual deviation, which was not considered a post-operative complication.
For the 29 (59%) patients who underwent surgery using the structured approach, the complications were as follows: one partial recurrence of airway obstruction, one partial bilateral retraction in the soft triangle, three high lateral osteotomies, two returns of the bone base to the original point, one partial re-occurrence of droopy nasal tip, two nostril asymmetries, and one nasal tip asymmetry.
The partial recurrence of airway obstruction occurred in a patient who was a victim of trauma, and possessed a flat nose and synechiae that obstructed the right airway almost completely. The synechiae were detached, but the reported an improvement in respiration when it partially re-adhered. For patients undergoing surgery with the conventional technique the complications were as follows: two high lateral osteotomies, two detectable post-osteotomy calluses, two nostril asymmetries, and one nasal tip asymmetry.
There were no occurrences of infection, dehiscence, epistaxis, hematoma, or systemic complications such as thrombosis or embolisms.
DISCUSSION
Rhinoplasty is one of the most commonly performed plastic surgeries in the world, but it also one of the most challenging. Initially it was developed as a procedure to alter the shape of the nose through closed, or endo-nasal access, with characteristic reduction of the structures. In recent decades, however, many surgeons have adopted the open approach. There is currently no consensus on which is the best way to achieve a good result. The main alteration in the philosophy of which was indeed superior, was the exchange in the reduction approach to one with added support by using grafts or maintaining the original nasal structure4,6.
The present study aimed to subjectively compare two non-reduction techniques, which are currently applied in rhinoplasty. The conventional technique, defended by some surgeons, avoids the excessive use of cartilage grafts, while aiming to alter the shape of the nose with the use of sutures and small cartilage resections.
The structured technique, on the other hand, requires a larger amount of cartilage graft, mainly donated by the septal or rib cartilage, to assemble the nose. Apologists of this technique claim that it guarantees better results in the long term and allows better re-shaping of the structures7. Critics of the structured technique argue that the nose becomes very rigid to the touch, and that excess graft tissue becomes visible over time3,4.
In the present study, the choice of technique was based on the individual preoperative evaluation of each patient and their need for the use of grafts to obtain a good result. Patients undergoing the conventional technique required a small amount of grafting, usually only the columellar strut, which was always derived from the septal cartilage. Patients on whom the structured technique was performed, received grafts from the septal cartilage, when available and in sufficient amount, or from the rib cartilage.
Graft manufacture, when utilized, followed established principles that were previously published by Farkas et al.8 and Toriumi4,9,10. As such, there were no complications such as nose deviation up to the moment of post-operative follow-up consultations. The main grafts utilized in those cases were spreaders, the columellar strut, alar strut, septum extender, bridge and nasal tip grafts, and margin grafts. The grafts used on the nasal tip and the nasal margin were always derived from the septum or the cephalic portion of the alars.
Throughout the period during which the surgeries were performed, the author of this work modified some procedures, according to post-operative follow-ups and scientific updates. One of the alterations regarded osteotomies. With both the structured and conventional technique there were cases of nasal bone base returning to its original position, following lateral osteotomy.
In order to avoid this complication, an external transversal osteotomy associated with the lateral was more frequently performed, which left a smaller region of the bone in a fragile state, and prevented the bone returning to its original location. Patients who were victims of trauma, with airway damage, also did not receive aesthetic osteotomies, since centering the bone wall and inferior turbinate could further impede the air passage, as attested by Guyuron11 in a study using cadavers.
The evolution of the author's technique, which was based on follow-up consultations and studies by other surgeons, also included increased use of grafts in the alar margin. The use of this type of graft was especially elevated when the patient developed an important retraction in the soft triangles, according to a study by Lee et al.12, in which the main flaws in primary rhinoplasties, and the steps required to correct them, were analyzed.
In addition to using more grafts in structured rhinoplasty, another technique that was prevalent in these cases was the use of the depressor muscle of the nasal septum, via an oral approach, as described by Rohrich et al.13 This occurred in two patients who underwent the structured technique, but did not occur in any of the patients who underwent the conventional technique. The conclusion regarding this difference was that the patients who also needed this component to modify a droopy nasal tip, required further extensive restructuring, which results in the use of more grafts in order to avoid reoccurrence.
In the cases of droopy nose tip, with thick skin and weak alar cartilages, columellar struts were used. In most cases, these were attached to the caudal septum in order to assure that they would be kept in place. They were used with the aim of projecting, supporting, and correcting eventual tip asymmetries, according to a study by Rohrich et al.14 In the cases of trauma that required the amputation and reconstruction of the nasal septum, the strut was attached to the nasal spine and the distended spreaders, in order to form a new "L Strut", as previously described by Toriumi15.
The work on the nasal tip followed well-established principles, such as that outlined by Toriumi and Checcone16, in order to reach a harmonious result. In both techniques, sutures proposed by Gruber et al.17 were used to shape the alar cartilages, and grafts in some cases.
The complications presented in this study were not considered to be exclusive to, or dependent on, each technique. Rather, the complications were inherent to any nasal surgery, regardless of the surgeon's choice of surgical approach.
On final follow-up, the surgeon and the patients did not favor any of the techniques; a favorable result was reached using both approaches.
A few limitations in the present study must be noted. Many patients had a short follow-up period, of only a few months, which does not permit adequate evaluation of the final result, especially in cases where the rhinoplasty required at least a year for scar retraction and for tissue edema to subside. This short period of follow-up can be attributed to the fact that some patients did not return for post-operative consultations and that some surgeries were performed shortly before this article was written. Further, the evaluation of the surgical result was not performed using any objective measurements. In the future, it would be interesting to use questionnaires or objective measurements to document the results. Furthermore, the evaluation would be more complete and impartial if performed by other professionals of the field who did not take part in the surgical procedures.
Nonetheless, this is a novel study, since there is no other published work comparing the two rhinoplasty techniques. The limitations of the study may serve to develop future clinical research, such as clinical trials and prospective follow-up studies.
CONCLUSION
Both the conventional and structured techniques, were efficient for aesthetic and corrective rhinoplasty approaches, from the point of view of patient as well as surgeon satisfaction. It was concluded that the fundamental step in rhinoplasty success is the correct pre-operative evaluation in order to select the best technique for each case.
COLLABORATIONS
PRR Data analysis and/or interpretation; final approval of the manuscript; conceptualization and design of the study; performance of the surgeries and/or experiments; and manuscript writing or critical review of its content.
REFERENCES
1. Stevens MR, Emam HA. Applied surgical anatomy of the nose. Oral Maxillofac Surg Clin North Am. 2012;24(1):25-38. DOI: http://dx.doi.org/10.1016/j.coms.2011.10.007
2. Guyuron B. Dynamics in rhinoplasty. Plast Reconstr Surg. 2000;105(6):2257-9. PMID: 10839427 DOI: http://dx.doi.org/10.1097/00006534-200005000-00057
3. Whitaker EG, Johnson CM Jr. The evolution of open structure rhinoplasty. Arch Facial Plast Surg. 2003;5(4):291-300. DOI: http://dx.doi.org/10.1001/archfaci.5.4.291
4. Toriumi DM. Structure approach in rhinoplasty. Facial Plast Surg Clin North Am. 2005;13(1):93-113. DOI: http://dx.doi.org/10.1016/j.fsc.2004.07.004
5. Ching S, Thoma A, McCabe RE, Antony MM. Measuring outcomes in aesthetic surgery: a comprehensive review of the literature. Plast Reconstr Surg. 2003;111(1):469-80. DOI: http://dx.doi.org/10.1097/00006534-200301000-00085
6. Bagheri SC, Khan HA, Jahangirnia A, Rad SS, Mortazavi H. An analysis of 101 primary cosmetic rhinoplasties. J Oral Maxillofac Surg. 2012;70(4):902-9. PMID: 21684661 DOI: http://dx.doi.org/10.1016/j.joms.2011.02.075
7. Toriumi DM. Structure approach in rhinoplasty. Facial Plast Surg Clin North Am. 2002;10(1):1-22. DOI: http://dx.doi.org/10.1016/S1064-7406(03)00078-6
8. Farkas JP, Lee MR, Lakianhi C, Rohrich RJ. Effects of carving plane, level of harvest, and oppositional suturing techniques on costal cartilage warping. Plast Reconstr Surg. 2013;132(2):319-25. PMID: 23897331 DOI: http://dx.doi.org/10.1097/PRS.0b013e3182958aef
9. Kim DW, Shah AR, Toriumi DM. Concentric and eccentric carved costal cartilage: a comparison of warping. Arch Facial Plast Surg. 2006;8(1):42-6. DOI: http://dx.doi.org/10.1001/archfaci.8.1.42
10. Lopez MA, Shah AR, Westine JG, O'Grady K, Toriumi DM. Analysis of the physical properties of costal cartilage in a porcine model. Arch Facial Plast Surg. 2007;9(1):35-9. DOI: http://dx.doi.org/10.1001/archfaci.9.1.35
11. Guyuron B. Nasal osteotomy and airway changes. Plast Reconstr Surg. 1998;102(3):856-60. DOI: http://dx.doi.org/10.1097/00006534-199809010-00037
12. Lee M, Zwiebel S, Guyuron B. Frequency of the preoperative flaws and commonly required maneuvers to correct them: a guide to reducing the revision rhinoplasty rate. Plast Reconstr Surg. 2013;132(4):769-76. PMID: 23783064 DOI: http://dx.doi.org/10.1097/PRS.0b013e3182a01457
13. Rohrich RJ, Huynh B, Muzaffar AR, Adams WP Jr, Robinson JB Jr. Importance of the depressor septi nasi muscle in rhinoplasty: anatomic study and clinical application. Plast Reconstr Surg. 2000;105(1):376-83. DOI: http://dx.doi.org/10.1097/00006534-200001000-00059
14. Rohrich RJ, Hoxworth RE, Kurkjian TJ. The role of the columellar strut in rhinoplasty: indications and rationale. Plast Reconstr Surg. 2012;129(1):118e-125e. PMID: 22186526 DOI: http://dx.doi.org/10.1097/PRS.0b013e3182362b7a
15. Toriumi DM. Subtotal septal reconstruction: an update. Facial Plast Surg. 2013;29(6):492-501. DOI: http://dx.doi.org/10.1055/s-0033-1360600
16. Toriumi DM, Checcone MA. New concepts in nasal tip contouring. Facial Plast Surg Clin North Am. 2009;17(1):55-90. DOI: http://dx.doi.org/10.1016/j.fsc.2008.10.001
17. Gruber RP, Chang E, Buchanan E. Suture techniques in rhinoplasty. Clin Plast Surg. 2010;37(2):231-43. DOI: http://dx.doi.org/10.1016/j.cps.2009.12.010
1. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
2. Universidade Federal de São Paulo, Escola Paulista de Medicina, São Paulo, SP, Brazil
Institution: Universidade Federal de São Paulo, Escola Paulista de Medicina, São Paulo, SP, Brazil.
Corresponding author:
Paolo Rubez Rocha
Alameda dos Maracatins, 426, cj 110
Moema, SP, Brazil Zip Code 04089-000
E-mail: paolorr@uol.com.br
Article received: July 29, 2015.
Article accepted: November 11, 2015.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter