

Original Article - Year 2017 - Volume 32 -
Assessment of immediate symmetrization in breast reconstruction
Avaliação das simetrizações imediatas em reconstrução de mama
ABSTRACT
INTRODUCTION: The surgical treatment of breast cancer frequently results in mutilation. Breast reconstruction in mastectomized women aims to create a new esthetically acceptable breast symmetrical to the contralateral breast. The objective of this study was to assess the feasibility of symmetrization of the contralateral breast simultaneously with breast reconstruction, discuss possible complications, and perform a brief review of the literature.
METHODS: A retrospective study was conducted in the Department of Plastic Surgery of Hospital Daher from October 2013 to February 2015. Breast reconstruction outcomes immediately after mastectomy for breast cancer were assessed, and all patients undergoing symmetrization of the contralateral breast in the same surgical stage using the same surgical technique were selected for inclusion and statistical analysis.
RESULTS: The study comprised 42 patients within the established criteria, totaling 21 reconstructions with simultaneous symmetrization (Group 1) and 21 symmetrization procedures in two stages (Group 2). The mean age was 53.86 years in Group 1 and 52.62 years in the control group. The groups were comparable in all variables. Data regarding postoperative complications were analyzed. Some of the studied patients did not complete all stages of reconstruction. The group that underwent immediate symmetrization attained more symmetry. The patients aged 45 years and with lower body mass index attained more symmetry in Group 1.
CONCLUSION: The implementation of symmetrization procedures at the same stage of unilateral breast reconstruction is associated with low complication rates and revision surgeries. In selected cases, immediate symmetrization may be preferable to the procedure in another surgical stage.
Keywords: Breast cancer; Breast neoplasms; Mammoplasty; Mastectomy.
RESUMO
INTRODUÇÃO: O tratamento cirúrgico do câncer de mama resulta com frequência em mutilação. A reconstrução de mama em mulheres mastectomizadas objetiva criar nova mama esteticamente aceitável e simétrica à mama contralateral. O objetivo deste estudo é estudar a viabilidade da simetrização da mama contralateral simultaneamente à reconstrução de mama, discutir possíveis complicações e fazer uma breve revisão da literatura.
MÉTODOS: Estudo retrospectivo realizado no Serviço de Cirurgia Plástica do Hospital Daher, de outubro de 2013 a fevereiro de 2015. Avaliadas as reconstruções mamárias imediatas pós-mastectomia por câncer de mama e selecionadas para inclusão todas as pacientes submetidas à simetrização da mama oposta no mesmo tempo cirúrgico, com mesma técnica cirúrgica e análise estatística.
RESULTADOS: Estudados 42 pacientes dentro dos critérios estabelecidos, totalizando 21 reconstruções com simetrização simultânea (Grupo 1) e 21 simetrizações em dois tempos (Grupo 2). A média de idade foi de 53,86 anos para o Grupo 1 e 52,62 anos para o grupo controle. Os grupos foram comparáveis para todas as variáveis. Os dados referentes às complicações pós-operatórias foram analisados. De todas as pacientes estudadas, algumas não finalizaram todas as etapas da reconstrução. O grupo que realizou simetrização imediata alcançou mais simetria. Pacientes com até 45 anos e com índice de massa corporal menor alcançaram mais simetria no Grupo 1.
CONCLUSÃO: A execução de procedimentos de simetrização no mesmo tempo de uma reconstrução de mama unilateral está associada a baixa taxa de complicação e de cirurgias de revisão. Em casos selecionados, a simetrização imediata pode ser preferível ao procedimento em outra etapa cirúrgica.
Palavras-chave: Mama; Neoplasias da mama; Mamoplastia; Mastectomia.
Breast cancer is the most common cancer among women1. According to the World Health Organization (WHO), more than 1,050,000 new cases occur per year worldwide. In Western countries, one in eight women will experience the disease during their lifetime2. The surgical treatment of breast cancer frequently results in mutilation.
Breast reconstruction is proposed as a part of the treatment of patients with breast cancer. The motivation and the desire of the patients are the main indications for reconstructions to be performed, thus reducing the deformities that develop after mastectomy. Besides its oncological safety, its psychological benefits have become an integral part of the treatment of breast cancer3-5.
The surgical treatment of breast cancer has evolved considerably from the era of Halstead radical mastectomy6. Further, one of the most current manifestations of this evolution can be observed today in the so-called skin-sparing adenomastectomies, in which attempts are made to preserve the skin of the breast as much as possible to improve the quality of the reconstruction, while preserving the nipple areola complex (NAC) in some cases.
The goal of breast reconstruction in women undergoing mastectomy is to create a new esthetically acceptable breast, besides attaining symmetry with the contralateral breast7. The reconstruction of the breast alone does not provide a harmonic result in most cases however perfect it is. Creating symmetry from different conditions of each side in a single surgery is quite rare. Even in cases of bilateral mastectomies, additional procedures are frequently necessary to achieve such outcomes.
Late reconstructions were traditionally the most popular method, while waiting for the adjuvant treatment and complete resolution of the neoplasm8. However, immediate reconstructions are now the current trend, which offer psychological benefits and improve esthetics without delaying the adjuvant treatment or worsening the prognosis of the patient8.
The decision to operate the contralateral breast is complex and multifactorial. Symmetrization is part of a planning and proper execution of the unilateral reconstruction8. The need for symmetrization of the contralateral breast depends on the pre-mastectomy characteristics, surgeon's preference, post-reconstruction characteristics, type of mastectomy, and reconstruction method used1.
Globally, it is accepted that the procedures on the contralateral breast should only occur in a second surgical stage7. Recently, there have been some groups performing symmetrization of the contralateral breast in the same mastectomy and reconstruction stage.
The potential advantages of this single-stage approach include: reduction in the number of surgeries, duration of treatment, and costs and avoidance of a prolonged period of asymmetry, especially if the secondary procedure is delayed by adjuvant therapy7.
The concerns that are often raised on the simultaneous reconstruction and contralateral symmetrization are that the additional surgery and surgical stage can increase complications or need for blood transfusions, and changes may occur in the shape of the breast during healing and may lead to new asymmetries.
OBJECTIVE
The objective of this study is to investigate the importance and feasibility of symmetrization of the contralateral breast simultaneously with breast reconstruction, discuss possible complications, and conduct a brief literature review.
METHODS
This was a retrospective study conducted in the Department of Plastic Surgery of Hospital Daher in Brasília, DF, from October 2013 to February 2015. The outcomes of the breast reconstructions immediately after mastectomy for breast cancer performed during this period were evaluated, and all patients undergoing symmetrization of the contralateral breast at the same surgical stage were selected for inclusion in the study. The control group included the same number of patients; however, they underwent symmetrization in a second surgical stage. Therefore, it is an intentional non-random sample.
Surgical Technique
The surgical techniques used in the two groups, both for immediate and late symmetrizations, were the same. The patients who underwent partial mastectomy and were reconstructed using mammoplasty (with or without the placement of a prosthesis) were submitted to the same surgery for the contralateral breast.
For the patients who underwent total mastectomy, the reconstruction included the placement of a prosthesis and temporary expansion or construction of a latissimus dorsi muscle flap. In this group, placement of a submuscular prosthesis with or without adjustments of the skin (mastopexy) was performed in the contralateral breast.
Data collected
The evaluated population characteristics were as follows: age, body mass index (BMI), breast size, presence of comorbidities, such as diabetes, hypertension, and hypothyroidism, and smoking status. The analyzed variables were as follows: hematoma, seroma, minor infection (defined as cases of erythema in a patient who has used antibiotics and with regression of presentation), major infection (infection that led to the loss of the implant), capsular contracture, and necrosis (flap and/or NAC). Data, such as the number of post-operative consultations, number of surgeries per patient, and need for complementary treatments, such as chemotherapy and radiation therapy, were also evaluated.
Statistical Analysis
The continuous variables with a normal distribution were analyzed using the Student's t-test for independent samples and presented as means ± standard deviations (SDs).
The continuous variables without a normal distribution were analyzed using the Mann-Whitney test and presented as medians and interquartile ranges.
The categorical variables were analyzed using the chi-squared test or Fisher's exact test, as appropriate, and were presented as absolute numbers and percentages. p values < 0.05 were considered statistically significant.
The present study followed the principles of the Helsinki Declaration, adopted by the 18th World Medical Assembly, Helsinki, Finland in June 1964 and corrected by the 29th Medical Assembly, Tokyo, Japan in October 1975, the 35th World Medical Assembly Venice, Italy in October 1983, and the 41st World Medical Assembly, Hong Kong in September 1989.
RESULTS
During the study period, 42 patients were selected within the established criteria, totaling 21 reconstructions with simultaneous symmetrization (Group 1) and 21 symmetrizations in two stages (Group 2).
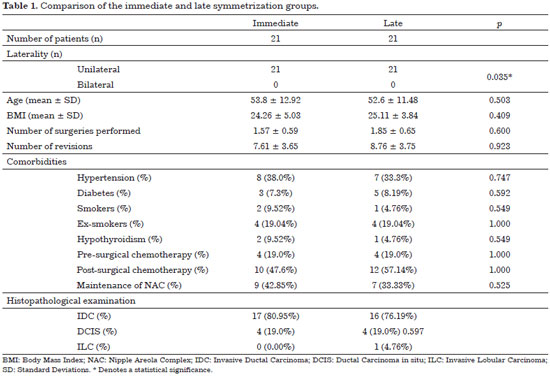
The mean age was 53.86 years for Group 1 and 52.62 years for the control group. The groups were comparable in all variables. The demographic data are shown in Table 1.
Table 1 shows the data that prove the homogeneity of the groups by means of statistical assessments. The unilaterality of the cases was predominant and had a statistical significance (p = 0.035) but without a clinical relevance.
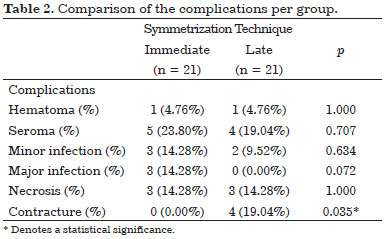
The data regarding the post-operative complications are listed in Table 2. No statistically significant differences were found between the groups for the rates of minor infections, hematoma, seroma, and necrosis. Group 1 presented with higher rates of major infections but without a statistical significance, and Group 2 presented with higher rates of capsular contractures with a statistical significance (p = 0.035).
There was a predominance of reconstructions with the use of prostheses, totaling 23 cases, followed by the use of expanders in 15 cases. There were no statistically significant differences regarding the type of reconstruction between the groups.
Of all the patients studied, some did not complete all stages of reconstruction. Those who completed the stages were distributed as shown in Table 3; Group 2 had a smaller number than Group 1. The number of surgeries of the patients who completed the reconstruction stages and needed corrections in the contralateral breast was lower in Group 1, in which simultaneous symmetrization was performed (Table 4).
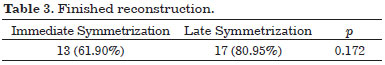
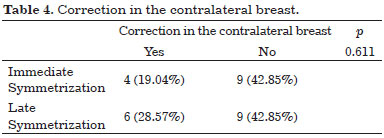
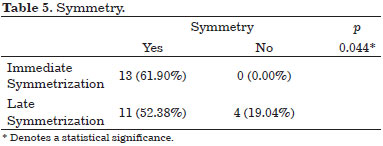
Table 5 indicates that the group that underwent immediate symmetrization attained significantly more symmetry (p = 0.044).
The patients up to 45 years old attained more symmetry in Group 1 with a statistical significance for this evaluation (Table 6).
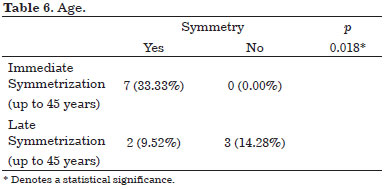
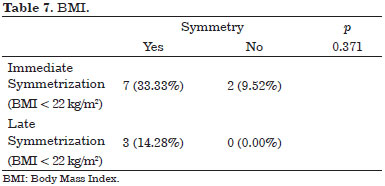
The patients with a BMI < 22 kg/m2 attained more symmetry in Group 1 (immediate symmetrization) than in Group 2 (delayed symmetrization), also with a statistical significance (Table 7).
Post-operative radiotherapy was performed in 11 patients who underwent simultaneous symmetrization (Group 1) and nine patients who underwent symmetrization in two stages (Group 2).
The results of the two methods studied are shown in the photographs in Figures 1 to 4.

Figure 1. Symmetrization in two stages. Left mastectomy is performed at the first surgical stage with reconstruction of the breast with an expander and contralateral mastopexy in the second surgical stage with a submuscular prosthesis for symmetrization with the contralateral breast.

Figure 2. Immediate symmetrization. Left mastectomy is performed with immediate reconstruction of the breast with an expander and contralateral symmetrization with mastopexy with a submuscular prosthesis for immediate symmetrization.
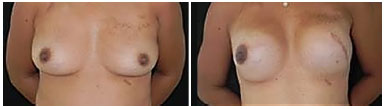
Figure 3. Immediate symmetrization. Left mastectomy is performed with immediate reconstruction of the breast with a submuscular expander and submuscular implant in the breast for contralateral symmetrization at the same surgical stage.
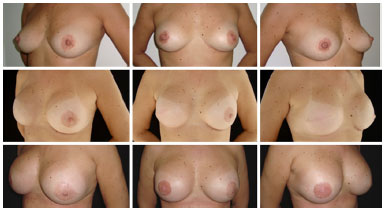
Figure 4. Immediate symmetrization. In the upper portion, the preoperative images of the patient are shown. In the middle portion, left mastectomy is performed with immediate reconstruction of this breast with a submuscular implant and simultaneous symmetrization in the contralateral breast with a submuscular implant. In the lower portion, a second surgical stage only for the construction of the nipple areola complex is performed.
DISCUSSION
The importance of breast symmetrization is becoming increasingly evident in breast reconstruction procedures. At present, we have more options for reconstructions than in the past, and our technical skills have improved. The expectations of women with breast cancer have been strengthened by virtue of the fact that the plastic surgeon is frequently able to reconstruct a breast with a natural volume and contour9-11.
The need for other surgical stages for completion of reconstruction is an important part of this process and must be previously understood and accepted by the patient. Thus, additional procedures, such as mammoplasty of the contralateral breast, reconstruction of the NAC, and corrections of irregularities and unsightly scars, are often essential to achieve a satisfactory esthetic result12.
The intention to perform the symmetrization procedure at the stage of initial reconstruction attempts to provide immediate symmetry of the breast and avoid the need for secondary procedures while maintaining patient safety 7. Hudson & Skoll13 reported the need for surgery in a healthy breast as a disadvantage; however, they cited that other studies have shown that over 80% of patients undergoing reconstructions will require a surgery in the contralateral breast for symmetrization.
Another way of addressing immediate symmetrization would be to minimize the size of the second stage surgery, leaving only small adjustments to be made, which is our biggest goal.
In our series, the number of surgeries to correct the contralateral breast was lower in Group 1 (immediate symmetrization), and Group 1 attained significantly more symmetry than Group 2 (delayed symmetrization) (p = 0.044). Moreover, post-operative radiotherapy was performed in 11 patients who underwent simultaneous symmetrization (Group 1) and in nine patients who underwent symmetrization in two stages (Group 2) without compromising the surgical outcomes achieved in symmetry or needing additional refinement surgeries.
Smith et al.7 showed that performing symmetrization at the same stage as the initial reconstruction resulted in a reduction of 76% of patients needing additional surgeries. Only 13% of the patients needed secondary symmetrization procedures.
To this end, we compared statistically equivalent groups, and we found that the complication rate in Group 1 (immediate symmetrization) was lower than that in Group 2 (delayed symmetrization).
Smith et al.7 also showed that the complication rates (11%) and blood transfusion rates (9%) were low. The complication rate for the contralateral breast was extremely low (1%), although previous studies have shown a desire to perform these procedures simultaneously because the risk of blood loss causes an unacceptably high rate of blood transfusion14-18.
We also found that the patients who presented with loss of reconstruction (implant removal owing to infection) showed no complications in the contralateral breast. Therefore, symmetrization in this specific group of patients did not alter the outcome.
A series of smaller studies are related to the subject; however, these studies did not comment on the indications, safety, or approach19-26.
Hudson & Skoll13 reported 18 cases of simultaneous contralateral symmetrization in single-stage reconstructions using implants. There were no complications in the contralateral breast; however, the average follow-up period was less than a year, and although they mentioned surgical complications in the reconstructed breast, they did not discuss revisions.
The patients submitted to the expansion of the tissue and reconstruction with implants are even more likely to require a symmetrization procedure. Two series show that 62-66% of women undergoing expander/implant reconstructions require contralateral symmetrization, compared with 37-41% of autologous reconstruction7.
In the groups studied herein, the reconstructions with prosthesis and expanders prevailed, which facilitates the symmetrization using the same technique. In all immediate symmetrizations, submuscular prostheses were used, except for the breast augmentation patients.
According to the literature, reductive mammoplasty is the most common symmetrization procedure in patients who had reconstruction using autologous tissues, and symmetrizations with prostheses are more common for reconstructions that used expanders or prostheses8, which was also observed in this series.
We also note that three patients were subjected to partial mastectomy and reconstructed with mammoplasty (oncoplastic surgery). In these patients, we performed contralateral mammoplasty for breast symmetrization, and these cases aroused our interest in attempting to develop a technique for the total mastectomies as well.
Hudson & Skoll13 showed that breast reduction or mastopexy in the contralateral breast, which was performed at the same stage as the symmetrization mastectomy, yielded good results and an obvious reduction in the costs when the surgery was performed in a single stage.
Stevenson & Goldstein26 performed a retrospective review of 25 patients who underwent reconstruction with a pedicled TRAM via a simultaneous symmetrization procedure compared with 14 patients who only had reconstruction with a TRAM. They found no differences in the surgical stage, blood loss, or length of hospital stay between the two groups; and no patient needed revisions of the contralateral side for symmetry. The average follow-up was 16 months.
Huang et al.27 also published a recent report on 22 cases using the free TRAM technique for unilateral reconstruction of the breast with the simultaneous symmetrization and observed that the esthetics was better than that in patients undergoing similar reconstructions without symmetrization.
In the only large series conducted by Chang et al.28, it was found that 50% of patients undergoing breast reconstructions require a contralateral symmetrization procedure. In their series, 14% (154 of 1120) of the patients underwent an immediate contralateral symmetrization procedure and 36% (404 of 1120) underwent a delayed contralateral procedure.
A revision of the procedures for contralateral symmetry was performed in 21% of patients, in general. The rate of revision was higher for augmentation mammoplasties and mastopexies in the immediate group than in the late-treatment group; however, there was no difference in the rates of revision for breast reduction between the two groups. A higher incidence of complications was reported in the immediate symmetrization procedure; however, the average number of procedures performed was significantly higher in patients undergoing delayed contralateral procedures than in those undergoing immediate contralateral procedures28.
Younger patients aged < 45 years and thinner patients with a BMI < 22 kg/m2 attained significantly more symmetry in Group 1 (immediate symmetrization) than in Group 2 (delayed symmetrization). Clinical series have shown that up to 86% of patients undergoing unilateral reconstructions benefit from surgery in the contralateral breast to improve symmetry12,19,29-31.
Smith et al.7 showed that their study provides further support for these results, demonstrating a significant reduction in the number of secondary procedures (24%) and revisions of symmetry (13%) in patients undergoing autologous reconstruction and immediate contralateral symmetrization procedures.
CONCLUSION
It is concluded that the implementation of symmetrization procedures at the stage of unilateral breast reconstructions is associated with a low complication rate and need for revision surgeries, even if the patients undergo post-operative radiation therapy. Furthermore, it enables some degree of symmetry earlier in the breast reconstruction process. Therefore, we believe that in selected cases, immediate symmetrization may be preferable to the procedure in another surgical stage.
COLLABORATIONS
MCC Analysis and/or interpretation of data; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
MCAG Analysis and/or interpretation of data; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
RQL Analysis and/or interpretation of data; completion of surgeries and/or experiments.
CMA Analysis and/or interpretation of data; completion of surgeries and/or experiments.
IRJ Analysis and/or interpretation of data; completion of surgeries and/or experiments.
LGM Analysis and/or interpretation of data; completion of surgeries and/or experiments.
LMCD Analysis and/or interpretation of data; completion of surgeries and/or experiments.
DASS Analysis and/or interpretation of data; completion of surgeries and/or experiments.
FTM Statistical analyses.
JCD Analysis and/or interpretation of data; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments.
REFERENCES
1. Meyer Ganz O, Tobalem M, Perneger T, Lam T, Modarressi A, Elias B, Pittet B. Risks and benefits of using an absorbable mesh in one-stage immediate breast reconstruction: a comparative study. Plast Reconstr Surg. 2015;135(3):498e-507e. PMID: 25719714 DOI: http://dx.doi.org/10.1097/PRS.0000000000001027
2. World Health Organization. Breast cancer: prevention and control [acesso 2014 Feb 12]. Disponível em: http://www.who.int/cancer/detection/breastcancer/en/
3. Al-Ghazal SK, Fallowfield L, Blamey RW. Comparison of psychological aspects and patient satisfaction following breast conserving surgery, simple mastectomy and breast reconstruction. Eur J Cancer. 2000;36(15):1938-43. DOI: http://dx.doi.org/10.1016/S0959-8049(00)00197-0
4. Rozen WM, Ashton MW, Taylor GI. Defining the role for autologous breast reconstruction after mastectomy: social and oncologic implications. Clin Breast Cancer. 2008;8(2):134-42.
5. Wilkins EG, Cederna PS, Lowery JC, Davis JA, Kim HM, Roth RS, et al. Prospective analysis of psychosocial outcomes in breast reconstruction: one-year postoperative results from the Michigan Breast Reconstruction Outcome Study. Plast Reconstr Surg. 2000;106(5):1014-25; discussion 1026.
6. Halstead WS. The results of operations for the cure of cancer of the breast performed at the Johns Hopkins Hospital from June, 1889, to January, 1894. Ann Surg. 1894;20(5):497-555.
7. Smith ML, Clarke-Pearson EM, Vornovitsky M, Dayan JH, Samson W, Sultan MR. The efficacy of simultaneous breast reconstruction and contralateral balancing procedures in reducing the need for second stage operations. Arch Plast Surg. 2014;41(5):535-41. PMID: 25276646
8. Losken A, Carlson GW, Bostwick J 3rd, Jones GE, Culbertson JH, Schoemann M. Trends in unilateral breast reconstruction and management of the contralateral breast: the Emory experience. Plast Reconstr Surg. 2002;110(1):89-97. PMID: 12087236
9. Jahkola T, Asko-Seljavaara S, von Smitten K. Immediate breast reconstruction. Scand J Surg. 2003;92(4):249-56. PMID: 14758913
10. Cunnick GH, Mokbel K. Skin-sparing mastectomy. Am J Surg. 2004;188(1):78-84. PMID: 15219490
11. NahabedianMY. Managing the opposite breast: contralateral symmetry procedures. Cancer J. 2008;14(4):258-63.
12. Enajat M, Smit JM, Rozen WM, Hartman EH, Liss A, Kildal M, et al. Aesthetic refinements and reoperative procedures following 370 consecutive DIEP and SIEA flap breast reconstructions: important considerations for patient consent. Aesthetic Plast Surg. 2010;34(3):306-12. PMID: 20424838
13. Hudson DA, Skoll PJ. Complete one-stage, immediate breast reconstruction with prosthetic material in patients with large or ptotic breasts. Plast Reconstr Surg. 2002;110(2):487-93; discussion 494-6.
14. Tzilinis A, Lofman AM, Tzarnas CD. Transfusion requirements for TRAM flap postmastectomy breast reconstruction. Ann Plast Surg. 2003;50(6):623-7.
15. Lennox PA, Clugston PA, Beasley ME, Bostwick J 3rd. Autologous blood transfusion in TRAM breast reconstruction: is it necessary? Ann Plast Surg. 2004;53(6):532-5.
16. Cohen J. Is blood transfusion necessary in reduction mammaplasty patients? Ann Plast Surg. 1996;37(1):116-8. DOI: http://dx.doi.org/10.1097/00000637-199809000-00002
17. Clugston PA, Fitzpatrick DG, Kester DA, Foley B, Germann E. Autologous blood use in reduction mammaplasty: is it justified? Plast Reconstr Surg. 1995;95(5):824-8.
18. Buenaventura S, Severinac R, Mullis W, Beasley M, Jacobs W, Wood D. Outpatient reduction mammaplasty: a review of 338 consecutive cases. Ann Plast Surg. 1996;36(2):162-6.
19. Panettiere P, Marchetti L, Accorsi D, Del Gaudio GA. Aesthetic breast reconstruction. Aesthetic Plast Surg. 2002;26(9):429-35.
20. Tran NV, Evans GR, Kroll SS, Baldwin BJ, Miller MJ, Reece GP, et al. Postoperative adjuvant irradiation: effects on tranverse rectus abdominis muscle flap breast reconstruction. Plast Reconstr Surg. 2000;106(2):313-7.
21. Smith ML, Evans GR, Gürlek A, Bouvet M, Singletary SE, Ames FC, et al. Reduction mammaplasty: its role in breast conservation surgery for early-stage breast cancer. Ann Plast Surg. 1998;41(3):234-9. PMID: 9746077
22. Petit J, Rietjens M, Garusi C. Breast reconstructive techniques in cancer patients: which ones, when to apply, which immediate and long term risks? Crit Rev Oncol Hematol. 2001;38(3):231-9. PMID: 11369256
23. Venus MR, Prinsloo DJ. Immediate breast reconstruction with latissimus dorsi flap and implant: audit of outcomes and patient satisfaction survey. J Plast Reconstr Aesthet Surg. 2010;63(1):101-5.
24. Song HM, Styblo TM, Carlson GW, Losken A. The use of oncoplastic reduction techniques to reconstruct partial mastectomy defects in women with ductal carcinoma in situ. Breast J. 2010;16(2):141-6.
25. Losken A, Pinell XA, Eskenazi B. The benefits of partial versus total breast reconstruction for women with macromastia. Plast Reconstr Surg 2010;125(4):1051-6. PMID: 20072088
26. Stevenson TR, Goldstein JA. TRAM flap breast reconstruction and contralateral reduction or mastopexy. Plast Reconstr Surg. 1993;92(2):228-33. PMID: 8337271
27. Huang JJ, Wu CW, Leon Lam W, Lin CY, Nguyen DH, Cheng MH. Simultaneous contralateral breast reduction/mastopexy with unilateral breast reconstruction using free abdominal flaps. Ann Plast Surg. 2011;67(4):336-42.
28. Chang EI, Selber JC, Chang EI, Nosrati N, Zhang H, Robb GL, et al. Choosing the optimal timing for contralateral symmetry procedures after unilateral free flap breast reconstruction. Ann Plast Surg. 2015;74(1):12-6.
29. Nahabedian MY. Symmetrical breast reconstruction: analysis of secondary procedures after reconstruction with implants and autologous tissue. Plast Reconstr Surg. 2005;115(1):257-60. PMID: 15622260
30. Nahabedian MY. Managing the opposite breast: contralateral symmetry procedures. Cancer J. 2008;14(4):258-63.
31. Asplund O, Svane G. Adjustment of the contralateral breast following breast reconstruction. Scand J Plast Reconstr Surg. 1983;17(3):225-32. PMID: 6673089 DOI: http://dx.doi.org/10.3109/02844318309013122
1. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
2. Hospital Daher Lago Sul, Brasília, DF, Brazil
3. Sociedade Brasileira de Anestesiologia, Rio de Janeiro, RJ, Brazil
Institution: Hospital Daher Lago Sul, Brasília, DF, Brazil.
Corresponding author:
Milena Carvalho Almeida Galdino
SHIS QI15, Chácara 68, Casa A - Lago Sul
Brasília, DF, Brazil Zip Code 71600-810
E-mail: almeida_mila12@yahoo.com.br
Article received: December 2, 2015.
Article accepted: February 21, 2017.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter