

Case Report - Year 2017 - Volume 32 -
Primary umbilical endometriosis: excision and neo-omphaloplasty
Endometriose umbilical primária: excisão e neo-onfaloplastia
ABSTRACT
INTRODUCTION: Umbilical primary endometriosis is a rare condition that affects women of childbearing age. Spontaneous umbilical endometriosis presents lump in the navel, cyclic pain, discreet local bleeding during menstruation, with no history of previous surgery. The treatment is block excision of the lesion and umbilical cord with edges margin to avoid recurrence and immediate umbilical reconstruction.
METHODS: We describe the surgical technique for circle excision of the umbilical endometrioma and neo-omphaloplasty in one stage.
CONCLUSION: The possibility of umbilical endometriosis should be considered when the presence of nodules and umbilical bleeding, even without previous surgery. The surgical technique provides total remission of the lesion and an umbilical natural scar.
Keywords: Endometriosis; Umbilicus; Rare diseases; Reconstructive surgical procedures.
RESUMO
INTRODUÇÃO: Endometriose primária de umbigo é uma afecção rara que acomete mulheres em idade fértil. A endometriose umbilical espontânea apresenta-se com nódulo em umbigo, dor cíclica, sangramento local discreto durante o período menstrual, sem história de cirurgia prévia. O tratamento consiste na excisão em bloco da lesão e cordão umbilical, com margens para evitar recorrência e a reconstrução umbilical imediata.
MÉTODOS: Apresentamos a técnica cirúrgica para excisão circular do endometrioma umbilical e a neo-onfaloplastia em um só estágio.
CONCLUSÃO: A possibilidade de endometriose umbilical deve ser considerada quando da presença de nodulações e hemorragias umbilicais, mesmo sem cirurgia prévia. A técnica cirúrgica proporciona remissão total da lesão e uma cicatriz umbilical de aspecto natural.
Palavras-chave: Endometrioma; Umbigo; Doenças raras; Procedimentos cirúrgicos reconstrutivos.
Endometriosis is a condition characterized by the presence of endometrial tissue outside the uterine cavity, which affects about 10% to 15% of women in childbearing age and often involves the ovaries, the fallopian tubes, the peritoneum, the uterine ligaments and the septum retovaginal1.
The cutaneous endometriosis is one of extra pelvic local where endometriosis is found and the majority of abdominal wall endometriomas described so far was observed in or near the cesarean section scars. The malignant transformation of the abdominal wall endometriosis is a rare complication and it occurs in less than 1% of cases2,3. Most authors believe in a multifactorial origin for endometriosis. The etiology of spontaneous umbilical form is not well established.
The umbilical primary endometriosis was first reported by Villar in 18862-4. It is considered a rare disease and affects 0.4 - 4% of all patients with endometriosis and accounts for 30 - 40% of cases of cutaneous endometriosis5,6. The clinical appearance of endometriosis in the navel can be of a brown or red wine-like injury, hard, nodular, rounded, with a history of changes in volume from 0.5 to 5 cm in diameter and it can cause local pain and bleeding during the menstrual cycle.
The umbilicus is described as a depressed scar, located in the midline of the abdominal wall at the level of the iliac crests with top diameter about 1.5 to 2 cm and a vertical orientation7. The umbilical scar is essential to the contour of the abdomen and its absence gives an unnatural appearance, causing embarrassment and discontent to the patient, which justifies its immediate reconstruction. Surgical treatment is through a full circular excision of the endometrioma with secure borders and the neo-omphaloplasty enables umbilicus with permanent depression and natural aspect.
OBJECTIVE
To emphasize surgical technique used for umbilicus reconstruction in the case of primary umbilical endometriosis.
METHODS
The study was approved by the Research Ethics Committee of the Hospital Maternidade Leonor Mendes de Barros on 04.07.2015 protocol nº. 1,032.262. The consent form was signed and the patient authorized publication of the image of the umbilical region. The authors declare no conflict of interest.
Surgical technique
The patient was placed in the supine position under spinal anesthesia and sedation. A circular excision in the entire lesion was carried out and safe margins were established to prevent local recurrence (Figure 1A). A block resection of umbilical cord until aponeurosis (Figure 1B) was done and the parietal peritoneum was visualized in order to exclude presence of endometriosis (Figure 1C), the wound was closured using nylon 2.0.
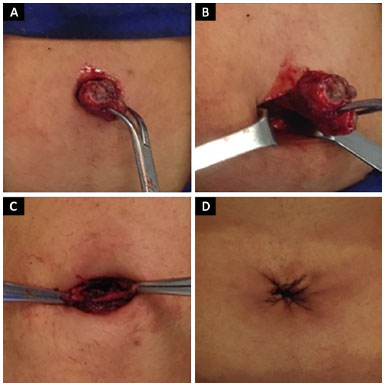
Figure 1. A: Circular excision of endometrioma with surgical margin; B: Block exeresis and umbilical cord; C: Viewing of subjacent aponeurosis; D: Synthesis of skin aponeurosis in the skin with small central bloody area.
The neo-omphaloplasty consists of removal of the subcutaneous tissue at the margin of the circular area and subsequent synthesis of the underlying dermis aponeurosis using a 4.0 nylon cord, while maintaining a small open area of approximately 1 cm in diameter (Figure 1D). The surgical procedure lasted 90 minutes and the patient was discharged on the first day after the surgery with prescription for antimicrobial medication and analgesic.
CASE REPORT
A 33-years-old woman without obstetric or surgical history. She had clinical history of nodule in the umbilicus scar in the last two years, presenting pain and minor bleeding during menstrual periods. The umbilical lesion was brown and red wine-like nodules, bleeding on palpation, measuring about 1.5 cm in diameter (Figure 2A).
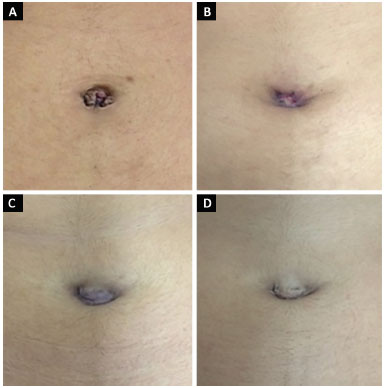
Figure 2. A: Umbilical endometriosis; B: 14 days after surgery; C: 3 months after surgery; D: 10 months after surgery.
A biopsy confirmed the suspected diagnosis of umbilical endometriosis. The abdominal ultrasound showed nodules measuring 6 x 5 x 5 mm at the umbilicus. The dosage of CA-125 revealed serum level of 16.0 U/ml, within normal range. The CA-125 (cancer antigen 125) is a serum marker for ovarian cancer that can be elevated in other malignancies and benign conditions such as endometriosis.
The complete epithelialization occurred in the umbilicus period of approximately 14 days (Figure 2B) when the suture wires were removal. The postoperative follow-up occurred in the clinic and the patient had a favorable clinical evolution and healing were normal 3 months after surgery (Figure 2C). After 10 months from the surgery, the patient reported no pain or swelling in the umbilicus, and no local recurrence was observed. The new navel presented natural and aesthetic appearance (Figure 2D).
Magnetic resonance imaging of the pelvis was normal. The pathological study identified the presence of endometrial tissue and confirmed the diagnosis of umbilical endometrioma (Figure 3).
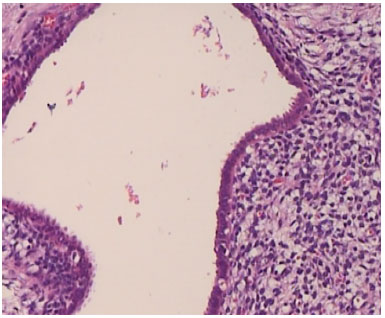
Figure 3. Histological imaging: presence of endometrial gland, epithelium and adjacent stroma, typical endometriosis.
DISCUSSION
The primary umbilical endometriosis is a rare entity and it is not related to the surgery. Incidence is about 0.5 to 1% of all cases of endometriosis extragenital. The typical clinical presentation of umbilical endometriosis is a purple lump in the umbilicus, which becomes swollen, painful and bleeding during menstruation.
Endometriosis is a disease of unknown etiology, probably multifactorial, whose pathophysiological mechanism is not fully understood. Many studies have investigate this disease that needs estrogen action to exist, but a clear knowledge of its origin was not reached. Endometriosis occurring in surgical scar is usually because of transplantation of endometrial tissue during surgery and ongoing ovarian action that at any time can lead to symptoms.
A number of theories attempt to explain the emergence of umbilical endometriosis, the most plausible is the implantation of endometrial cells from menstrual reflux through the fallopian tubes proposed by Sampson in 1925. However, this theory explains the appearance of pelvic peritoneal implants. The cell transplantation in surgical path may explain the occurrence in surgical scars, but it does not indicate endometriomas locations in distant organs.
Halban developed the theory of vascular or lymphatic migration of endometrial cells to ectopic sites. The theory of coelomic metaplasia is based on embryological studies and involves the transformation of cells of the peritoneal mesothelium endometrial tissue under the effect of inflammatory, traumatic, toxic or hormonal factors8,9.
Recent studies investigate environmental changes that may lead to the development of endometriosis and exposure to tetraclorodibenzopdioxina, commonly called dioxin. This is a lipophilic pollutant derived from waste incineration and processing of metals that contaminates food for human consumption and interacts little known endocrine and immunological mechanisms, but potentially involved in the pathogenesis of endometriosis, by dioxin action, which accounts for changes of encoding genes of estradiol synthesis and progestagenic receptors.
Despite the strong evidence of vascular dissemination or lymph of endometrial cells in the setting of primary umbilical endometriosis, we could not disregard data relating the disease to environmental factors, such as food contamination by dioxin10.
The differential diagnosis includes benign processes such as umbilical hernia, granulomas, nevi, cysts, seborrheic keratosis and keloid, in addition to malignant injuries such as melanoma, gastrointestinal tumor metastasis11.
Surgery is the treatment for endometrioma (Villar nodule) and this procedure entails complete excision of the lesion with a safety margin to avoid recurrence12-14. The patient should be advice on the possible local recurrence. The histopathological exam should always be requested.
CONCLUSION
The primary umbilical endometriosis is rare and it considered in the differential diagnosis in women with node, cyclic pain and bleeding associated with menstrual period. The diagnosis is clinical and histological. Surgery consists of total excision of endometrioma and umbilical cord with immediate umbilical reconstruction using the circle technique providing an adequate treatment resulting in minimal scarring and well located in the umbilical region.
ACKNOWLEDGMENT
We thank Dr. Maria Aparecida de Moraes Rebello Pinho for providing digital images of anatomopathological study.
COLLABORATIONS
RLS Final approval of the manuscript; cconception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
STY Analysis and/or interpretation of data.
LGS Analysis and/or interpretation of data; writing the manuscript or critical review of its contents.
TAO Writing the manuscript or critical review of its contents.
CMN Analysis and/or interpretation of data.
REFERENCES
1. Fancellu A, Pinna A, Manca A, Capobianco G, Porcu A. Primary umbilical endometriosis. Case report and discussion on management options. Int J Surg Case Rep. 2013;4(12):1145-8. DOI: http://dx.doi.org/10.1016/j.ijscr.2013.11.001
2. Efremidou EI, Kouklakis G, Mitrakas A, Liratzopoulos N, Polychronidis ACh. Primary umbilical endometrioma: a rare case of spontaneous abdominal wall endometriosis. Int J Gen Med. 2012;5:999-1002. DOI: http://dx.doi.org/10.2147/IJGM.S37302
3. Pramanik SR, Mondal S, Paul S, Joycerani D. Primary umbilical endometriosis: A rarity. J Hum Reprod Sci. 2014;7(4):269-71. DOI: http://dx.doi.org/10.4103/0974-1208.147495
4. Pariza G, Mavrodin CI. Primary umbilical endometriosis (Villar's nodule) - case study, literature revision. Chirurgia (Bucur). 2014;109(4):546-9.
5. Kaya B, Aslan E, Cerkez C, Kaygusuz G, Serel S. Endometriose cutânea. Rev Bras Cir Plást. 2012;27(3):493-5. DOI: http://dx.doi.org/10.1590/S1983-51752012000300031
6. Ghosh A, Das S. Primary umbilical endometriosis: a case report and review of literature. Arch Gynecol Obstet. 2014;290(4):807-9. PMID: 24930115 DOI: http://dx.doi.org/10.1007/s00404-014-3291-8
7. Kokuba EM, Sabino NM, Sato H, Aihara AY, Schor E, Ferreira LM. Reconstruction technique for umbilical endometriosis. Int J Gynaecol Obstet. 2006;94(1):37-40. PMID: 16781715 DOI: http://dx.doi.org/10.1016/j.ijgo.2006.04.034
8. Abramowicz S, Pura I, Vassilieff M, Auber M, Ness J, Denis MH, et al. Umbilical endometriosis in women free of abdominal surgical antecedents. J Gynecol Obstet Biol Reprod (Paris). 2011;40(6):572-6. DOI: http://dx.doi.org/10.1016/j.jgyn.2011.05.002
9. Schor E et al. Endometriose. In: Girão MJBC, Lima GR, Baracat EC, eds. Ginecologia. Barueri: Manole; 2009. p.189-197.
10. Carvalho BR, Silva JCR, Silva CJSR, Barbosa HF, Poli Neto OB, Reis FJC, et al. Endometriose umbilical sem cirurgia pélvica prévia. Rev Bras Ginecol Obstet. 2008;30(4):167-70. DOI: http://dx.doi.org/10.1590/S0100-72032008000400002
11. Malebranche AD, Bush K. Umbilical endometriosis: A rare diagnosis in plastic and reconstructive surgery. Can J Plast Surg. 2010;18(4):147-8.
12. Vilas Sueiro A, Monteagudo B, Suárez Amor Ó, Rodríguez Pazos L, González Vilas D, Pérez Valcárcel J, et al. Primary endometriosis: a differential diagnosis with the umbilical nodular lesions. Dermatol Online J. 2014;20(9):pii:13030/qt4kq933jq.
13. Arkoulis N, Chew BK. An unusual case of asymptomatic spontaneous umbilical endometriosis treated with skin-sparing excision. J Surg Case Rep. 2015;2015(3). pii: rjv017. DOI: http://dx.doi.org/10.1093/jscr/rjv017
14. Theunissen CI, IJpma FF. Primary umbilical endometriosis: a cause of a painful umbilical nodule. J Surg Case Rep. 2015;2015(3). pii:rjv025. DOI: http://dx.doi.org/10.1093/jscr/rjv025
1. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
2. Hospital e Maternidade Leonor Mendes de Barros, São Paulo, SP, Brazil
3. Federação Brasileira das Associações de Ginecologia e Obstetrícia, Rio de Janeiro, RJ, Brazil
Institution: Hospital Maternidade Leonor Mendes de Barros, São Paulo, SP, Brazil.
Corresponding author:
Roberto Luiz Sodré
Rua Antonio Alves Barril, 355/191 - Jardim Anália Franco
São Paulo, SP, Brazil Zip Code 03338-000
E-mail: roberto.sodre@uol.com.br
Article received: September 10, 2015.
Article accepted: February 3, 2017.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter