

Original Article - Year 2017 - Volume 32 -
Total nasal reconstruction: use of the "sandwich technique" during residency
Reconstrução nasal total: uso da "técnica em sanduíche" durante a residência
ABSTRACT
INTRODUCTION: One of the most common sites of skin cancer is the nose, and because of its distinct three-dimensional structure, reconstruction of the nasal tip support is challenging for plastic surgeons.
METHODS: This article presents an alternative option for total nasal reconstruction using the bilateral frontal flap and the block bilateral auricular cartilage graft. We present an account of the use of the "sandwich technique", consisting of two frontal flaps interspersed by auricular cartilage. While the first flap gives rise to the new roof of the nasal fossa, the cartilage configures the three-dimensional shape and provides support for the new nasal structure. The second flap is then responsible for the outer coverage.
RESULTS: In this case, both the minimal morbidity of the donor area and excellent perfusion of the autonomized flaps were verified, leading to a largely satisfactory result.
CONCLUSIONS: Although total nasal reconstruction is an infrequent procedure in the career of a plastic surgeon, the technique described here is a viable option for these cases.
Keywords: Surgical flaps; Nose/surgery; Nasal tumors; Reconstructive surgical procedures.
RESUMO
INTRODUÇÃO: Um dos locais mais comuns para o surgimento de câncer de pele é o nariz e, devido à sua distinta estruturação em três dimensões, a reconstrução do suporte da ponta nasal apresenta-se como um desafio para os cirurgiões plásticos.
MÉTODOS: Este artigo apresenta uma das opções de reconstrução nasal total utilizando como recursos o retalho frontal bilateral e o enxerto de cartilagem auricular bilateral em bloco. Apresentamos um relato do uso da "técnica em sanduíche", constituída por dois retalhos frontais intercalados pelas cartilagens auriculares. Enquanto o primeiro retalho origina o novo teto das fossas nasais, a cartilagem configura o formato tridimensional e garante o suporte da nova estrutura nasal. O segundo retalho fica, então, responsável pela cobertura exterior.
RESULTADOS: Neste caso comprovou-se tanto a mínima morbidade da área doadora quanto a excelente perfusão dos retalhos autonomizados, o que se considerou um resultado amplamente satisfatório.
CONCLUSÕES: Embora a reconstrução nasal total seja um procedimento infrequente na vida do cirurgião plástico, a técnica aqui descrita mostra-se como uma opção atraente para estes casos.
Palavras-chave: Retalhos cirúrgicos; Nariz/cirurgia; Neoplasias nasais; Procedimentos cirúrgicos reconstrutivos.
One of the most common sites of skin cancer is the nose, and because of its distinct three-dimensional structure, reconstruction of the nasal tip poses a challenge for plastic surgeons1,2. In this context, the alar and quadrangular cartilages are critical structures responsible for the projection and maintenance of the shape and function of the lower third of the nose3,4. Although several techniques exist for the partial reconstruction of these cartilages, only a few authors have described total reconstruction techniques3.
Basic principles for the successful reconstruction of the nasal skin cover should include confirmation of free surgical margins, precise determination of the size and location of the defect to be treated, and evaluation of other pre-existing defects5. Other important factors include achieving a color and texture that conforms to the original, with a thick tissue structure capable of maintaining its shape and support in spite of gravity, tension and scarring, and a thin, flexible coverage that does not affect the passage of air6.
In situations of partial and total alar reconstruction, two graft fragments are usually used to simulate the original form of the pre-existing cartilage4. The graft materials can be classified as autogenous, allogeneic, and homogenous, according to their origin1. Autogenous grafts are preferred for the support of both the dorsum and the nasal tip2, and some of their advantages include: greater durability, immediate availability, flexibility within the nose, and absence of an immune response1. However, they are associated with the risk of donor area morbidity and potential graft resorption1.
With regard to tissue coverage, full thickness skin grafts are historically used to replace the nasal cover. The most common donor sites include the pre- and post-auricular, supraclavicular, and nasolabial regions5. When flaps are indicated, the most common donor site is the frontal region due to its excellent vascularization7.
The frontal flap is recommended in situations of defect reconstruction involving the alar and columella areas, or for defects of the nasal tip8. The safety of this type of flap has been well established through anatomical studies9,10, and its advantages include: the ability to promote stable structuring, good coloration, adequate texture, and easy reproducibility8,11.
It is essential for the flap to cover the cartilages accurately. A small flap can make the cartilaginous structure collapse, while a large flap can promote excessive scar retraction12. In situations involving nasal coverage with large grafts, it is important to keep in mind that a high esthetic standard is less likely to be achieved, given the variability of the properties in the region to be reconstructed11. However, patients seem to be less critical of the esthetic results than are professionals, with reported satisfaction rates of around 79%7.
The innovative technique developed in 1995 by Max Pereira uses conchal and tragal auricular cartilage for the reconstruction of the alar cartilages. Sufficient restoration of the size, shape, and thickness of the original cartilage was cited as a major advantage. In this technique, an auricular graft is used on each side, removed en bloc by an anterior or posterior approach, one for each alar cartilage. Moreover, sutures are not required to model the shape of the new cartilage2.
The use of this technique is practiced in adults, although there are reported cases of its applicability in the treatment of fetal malformations. While some authors strive to perform reconstructive nasal surgery only in children aged 8 years and older, an exo-rhinoplasty approach with good esthetic and functional outcomes has already been successfully applied in a 23-day-old child13.
The most important postoperative complication includes nasal tip necrosis, the reported rates of which vary between 0 and 12%7. Although cartilage tends to appear excessively projected in the immediate or short-term postoperative context, a layer of scars is gradually formed between the new cartilages and the flap, ultimately conferring a natural look to the final result12.
Finally, as a general guideline, it is suggested that the surgeon should exercise restraint in repairing only the defect in question, and not the entire facial subunit, thereby enabling the maximum preservation of inherent tissue14.
OBJECTIVE
The objective of this article is to present one of the options for total nasal reconstruction using an auricular cartilage graft, according to the technique described by Max Pereira: the double-sided bilateral frontal flap.
METHODS
Clinical case
A 79-year-old male patient, with a history of basal cell carcinoma (BCC) excision in the nasal dorsum and reconstruction with primary suture 4 years ago, was received at our plastic surgery service (Hospital São Lucas, Pontifical Catholic University of Rio Grande do Sul - Porto Alegre, RS), with a recurrence after 1 year of undergoing new excision of the lesion and rotation of the interpolated nasogenic bilateral flap, which was not autonomized.
This patient was attended in our plastic surgery service in 2015, due to a recurrent lesion on the dorsum and nasal tip with 1 year of evolution. Upon physical examination, a scaly ulcerated lesion on the dorsum and nasal tip compromising the nasal alae and columella was observed. According to the tomographic report, there was deep invasion up to the nasal septum, but without bone invasion. Functionally, he presented with retraction of the nasal orifices and bilateral internal valve dysfunction associated with respiratory distress (Figure 1).
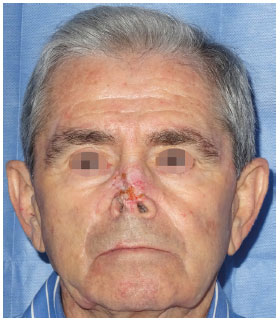
Figure 1. Neoplastic lesion affecting the dorsum and nasal tip with extension to the nasal ala bilaterally and the columella. The non-autonomous interpolated flap of the second reconstruction (performed by another surgeon) and the narrowing of the nostrils are observed.
Surgical technique
A total block excision of the neoplasia was conducted, with 0.5-cm surgical margins, followed by partial excision of the septal cartilage next to the mucosa and excision of the alar cartilages maintaining its proximal third (Figure 2). Due to the previous history of recurrence, a freezing biopsy was requested during the surgical procedure, which demonstrated tumor-free surgical margins.

Figure 2. Result after total excision of the neoplasia. Note the excision of part of the nasal septum and nasal ala. The nasal bone is free of neoplasia. Marking of the bilateral frontal flap is seen.
The use of two frontal flaps associated with auricular cartilage grafting for three-stage alar reconstruction was planned. The patient agreed to the procedure proposed by the team and signed an informed consent form for the scientific use of his photographs. The operative phases were as follows:
- Preparation of the first flap (left) according to the usual technique: rotation was performed on itself, bifurcating the flap and keeping the distal third skin. Later, this distal portion will cover the roof of the nasal passages bilaterally. Suture was performed between the medial skin portion of the bipartite flap and the mucosa on either side of the septum, as well as between the lateral skin portion of the bipartite flap and the inner part of the remaining nasal alae. The central part of the pedicle of the flap was de-epidermized (dotted area) in order to have contact with the exposed dorsum bone and cartilage. The proximal part of the flap retained the skin to constitute the free bridge of the frontal flap (Figures 2 and 3).
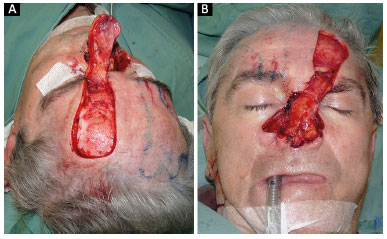
Figure 3. A: Preparation of the left frontal flap and its detachment; B: Rotation of the flap over itself and the creation of the nostrils.
- Grafting of the auricular cartilage according to the Max Pereira technique: In order to maintain the support of the new nose, a block excision of the auricular cartilage was used. First, skin marking on the anterolateral region of the concha and posterior part of the tragus was carried out, followed by transfixing the cartilages with a needle and methylene blue for labeling, incision of the skin from the outer edge of the marking, and detachment until exposure of the required cartilage was achieved. Then, incision and block excision of cartilage and skin suture plus Brown curative were performed. After this, the auricular cartilage on each side was rotated and placed close to the contralateral side and joined by non-absorbable sutures in the region corresponding to the new medial cross and new dome (Figure 4).
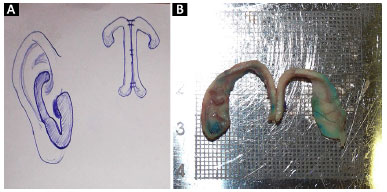
Figure 4. A: Preoperative design of the technique; B: Part of the rotated and sutured cartilage. The resemblance to normal alar cartilages is striking.
The new cartilaginous support structure was positioned and fixed with non-absorbable sutures to the nasal septum and each remaining nasal ala (Figure 5).
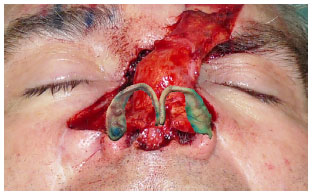
Figure 5. Figure representing the positioning of the new alar cartilage.
Preparation of the second frontal flap (right): This flap had the shape of the tip, dorsum, columella, and nasal ala in the distal part and was rotated to maintain the skin on the exterior of the cover. It was then placed on the cartilaginous structure, constituting a "sandwich" format. When closing, and to avoid creating tension in the skin of the forehead, it was decided to leave the most distal part of the periosteum exposed (Figure 6).
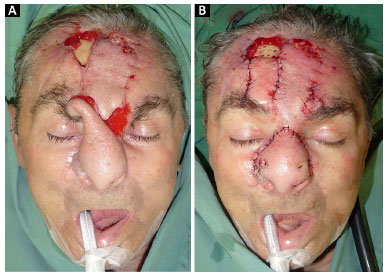
Figure 6. A: At 1 month postoperatively and prior to the autonomization of the frontal flaps; B: After releasing the vascular pedicles. Note the perforation of the outer table of the frontal bone up to the spongy bone.
RESULTS
One month after surgery, the frontal flaps were autonomized. The patient suffered periosteal necrosis of the frontal bone exposed at the beginning of surgery. This complication was managed with perforation of the outer table of the frontal bone with a circular drill to stimulate bleeding and granulation tissue growth (Figure 6). Two days later, the first dressing was performed, showing good perfusion of the autonomic flap, permeable nostrils, good projection of the nasal tip, and formation of granulation tissue in the bone perforations (Figure 7).

Figure 7. A: Two days after surgery for autonomization and treatment of exposed bone, frontal view; B: Right oblique view.
We call attention to the lack of sequelae in the cartilage donor area (Figure 8) and the pleasant esthetic result after 6 months (Figure 9).
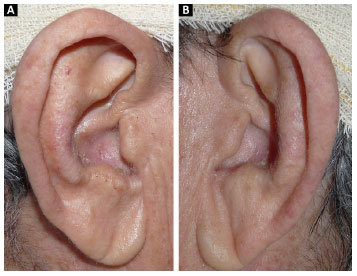
Figure 8. A: Right ear; B: Left ear. Donor area of cartilage without sequelae at 1 month after graft removal.
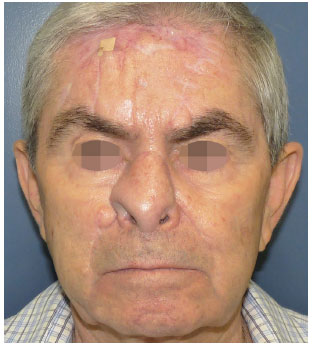
Figure 9. Final result at 8 months after autonomization surgery. Note the proper growth of granulation tissue in the region of the frontal bone. The patient awaits another surgical procedure to defat the flap.
DISCUSSION
Skin cancer is a prevalent condition in Brazil, and the nasal area is very commonly affected because of its direct exposure to the sun's action. The nose has vast esthetic and functional relevance; due to its location in the central area of the face, it is a noble structure that plays a critical role in the evaluation of the overall beauty of the face. The nose is a frequent site of destructive carcinomas with stigmatizing results15. For these reasons, the development of the plastic surgeon's expertise requires great knowledge and training in reconstructive nasal surgery.
Several nasal reconstruction techniques have been described16-20, with records dating from 2000 BC showing interest in the anatomical peculiarities of the area21. The restoration of the nose is based on the understanding that it is a three-dimensional structure21,22 composed of multiple layers. The relevant methods aim to diligently and meticulously repair all internal lining deficiencies, by not only filling the irregularities but also reshaping the nose, functionally (maintaining the airway) and esthetically21-24.
The use of grafts and local flaps is well known and taught in the first year of specialist training; however, total nasal reconstruction techniques are performed with low frequency by residents due to the high degree of tactical complexity. Planning becomes difficult when it is necessary to provide indoor and outdoor coverage, as well as support the structures.
For internal nasal coverage, flaps of the nasal mucosa, buccal mucosa flaps, or skin grafts that will undergo tissue metaplasia to mimic the normal nasal mucosa may be used. For the external cover, the frontal flap is one of the most indicated. A second surgical procedure is necessary for the autonomization of the flaps, resection of the interpolated pedicles, repositioning of the altered facial units, and refinements21. For this reason, the surgeon should also check with the patients regarding their commitment to a complex multi-stage procedure25.
The patient's own cartilage tissue is the ideal material for the support of structures. This tissue may be from the septum, conchal auricular cartilages, or costal cartilages. The cartilage graft is intended to support the nasal wing, as well as to shape it, attaining projection, and maintaining airway permeability22, 26. Sometimes, it is also used to recreate the septum, resulting in a better nasal structure. This eliminates the need to suture and sculpt the graft, making the procedure simpler and more likely to yield a good outcome21.
In the clinical case described, an initial frontal flap was used to cover the nose, taking advantage of the distal skin of the flap to constitute the roof of the new nasal cavities. The structural support of the nose was achieved with bilateral auricular cartilage grafting according to the technique described by Max Pereira. The outer covering of the nose was addressed by a second frontal flap designed according to the shape of the skin defect. This technique, which the authors call the "sandwich technique", is an attractive option for total nasal reconstruction and is optimally performed during the plastic surgeon's training during residency.
CONCLUSIONS
Total nasal reconstruction is an infrequent procedure during the professional career of the plastic surgeon, especially during residency. This article elucidates the process of a relevant surgical option in complex cases that require detailed planning and superior anatomical knowledge. The authors present the "sandwich technique" as an attractive alternative for total nasal reconstruction.
COLLABORATIONS
RFMR Analysis and/or interpretation of data; final approval of the manuscript; conception and design of the study; ompletion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
LS Final approval of the manuscript; completion of surgeries and/or experiments.
PG Analysis and/or interpretation of data; statistical analyses; writing the manuscript or critical review of its contents.
KM Analysis and/or interpretation of data; writing the manuscript or critical review of its contents.
AM Completion of surgeries and/or experiments.
COU Final approval of the manuscript; conception and design of the study.
REFERENCES
1. Immerman S, White WM, Constantinides M. Cartilage grafting in nasal reconstruction. Facial Plast Surg Clin North Am. 2011;19(1):175-82. DOI: http://dx.doi.org/10.1016/j.fsc.2010.10.006
2. Pereira MD, Andrews JM, Martins DM, Marques AF, Ishida LC. Total en bloc reconstruction of the alar cartilage using autogenous ear cartilage. Plast Reconstr Surg. 1995;95(1):168-72. DOI: http://dx.doi.org/10.1097/00006534-199501000-00030
3. Pereira MD, Marques AF, Ishida LC, Smialowski EB, Andrews JM. Total reconstruction of the alar cartilage en bloc using the ear cartilage: a study in cadavers. Plast Reconstr Surg. 1995;96(5):1045-52. DOI: http://dx.doi.org/10.1097/00006534-199510000-00006
4. Oliveira MF, Pereira MD, Ferreira LM. Reconstrução total da cartilagem alar utilizando enxerto de cartilagem auricular em bloco após ressecção tumoral. Rev Bras Cir Plast. 2010;25(3 Suppl 1):26.
5. Weber SM, Wang TD. Options for internal lining in nasal reconstruction. Facial Plast Surg Clin North Am. 2011;19(1):163-73. DOI: http://dx.doi.org/10.1016/j.fsc.2010.10.005
6. Menick F. Practical details of nasal reconstruction. Plast Reconstr Surg. 2013;131(4):613e-30e. PMID: 23542280 DOI: http://dx.doi.org/10.1097/PRS.0b013e3182827bb3
7. Mureau MA, Moolenburgh SE, Levendag PC, Hofer SO. Aesthetic and functional outcome following nasal reconstruction. Plast Reconstr Surg. 2007;120(5):1217-27. DOI: http://dx.doi.org/10.1097/01.prs.0000279145.95073.ed
8. Kumar S, Jacob MM. Simultaneous resection and reconstruction of the nose using frontal flap. J Maxilofac Oral Surg. 2010;9(1):108. DOI: http://dx.doi.org/10.1007/s12663-010-0005-z
9. Boyd CM, Baker SR, Fader DJ, Wang TS, Johnson TM. The forehead flap for nasal reconstruction. Arch Dermatol. 2000;136(11):1365-70. PMID: 11074699 DOI: http://dx.doi.org/10.1001/archderm.136.11.1365
10. Reece EM, Schaverien M, Rohrich RJ. The paramedian forehead flap: a dynamic anatomical vascular study verifying safety and clinical implications. Plast Reconstr Surg. 2008;121(6):1956-63. PMID: 18520881 DOI: http://dx.doi.org/10.1097/PRS.0b013e3181707109
11. Choi JW, Hong JP, Lee My, Suh DC. Total nose reconstruction using superselective embolisation and a forehead flap: overlooked in recurrent massive vascular malformations of the nose. J Plast Reconstr Aesthet Surg. 2010;63(3):423-30. DOI: http://dx.doi.org/10.1016/j.bjps.2008.11.048
12. Burget GC. Reconstruction of the alar cartilage arches. Operach Tech Plast Reconstr Surg. 1995;2(1):55-66. DOI: http://dx.doi.org/10.1016/S1071-0949(05)80017-4
13. Collares MVM, Faller GJ, Castro ACB, Portinho CP. Reconstrução nasal neonatal na síndrome do Warfarin fetal. Rev AMRIGS (Porto Alegre). 2009;53(2):184-7.
14. Rohrich RJ, Griffin JR, Ansari M, Beran SJ, Potter JK Nasal reconstruction--beyond aesthetic subunits: a 15-year review of 1334 cases. Plast Reconstr Surg. 2004;114(6):1405-16.
15. Linares MA, Zakaria A, Nizran P. Skin Cancer. Prim Care. 2015;42(4):645-59. PMID: 26612377 DOI: http://dx.doi.org/10.1016/j.pop.2015.07.006
16. Oseni A, Crowley C, Lowdell M, Birchall M, Butler PE, Seifalian AM. Advancing nasal reconstructive surgery: the application of tissue engineering technology. J Tissue Eng Regen Med. 2012;6(10):757-68. DOI: http://dx.doi.org/10.1002/term.487
17. Parrett BM, Pribaz JJ. An algorithm for treatment of nasal defects. Clin Plast Surg. 2009;36(3):407-20. PMID: 19505611 DOI: http://dx.doi.org/10.1016/j.cps.2009.02.004
18. Fischer H, Gubisch W. Nasal reconstruction: a challenge for plastic surgery. Dtsch Arztebl Int. 2008;105(43):741-6. PMID: 19623298
19. Salgarelli AC, Bellini P, Multinu A, Magnoni C, Francomano M, Fantini F, et al. Reconstruction of nasal skin cancer defects with local flaps. J Skin Cancer. 2011;2011:181093. PMID: 21773033 DOI: http://dx.doi.org/10.1155/2011/181093
20. Antunes MB, Chalian AA. Microvascular reconstruction of nasal defects. Facial Plast Surg Clin North Am. 2011;19(1):157-62. DOI: http://dx.doi.org/10.1016/j.fsc.2010.10.014
21. Senandes LS, Vizzotto MD, Fischer A, Zanol F, Lima VS. Complex nasal reconstruction: series of 10 cases. XXX Jornada Sul-brasileira de Cirurgia Plástica-Gramado-RS. Arq Catarin Med. 2014;43(supl. 1):150-4.
22. Choe YS, Kim MW, Jo SJ. A Novel Approach for Full-Thickness Defect of the Nasal Alar Rim: Primary Closure of the Defect and Reduction of the Contralateral Normal Ala for Symmetry. Ann Dermatol. 2015;27(6):748-50. DOI: http://dx.doi.org/10.5021/ad.2015.27.6.748
23. Han DH, Mangoba DC, Lee DY, Jin HR. Reconstruction of nasal alar defects in asian patients. Arch Facial Plast Surg. 2012;14(5):312-7. DOI: http://dx.doi.org/10.1001/archfacial.2012.520
24. Park SS. Nasal reconstruction in the 21st century--a contemporary review. Clin Exp Otorhinolaryngol. 2008;1(1):1-9. DOI: http://dx.doi.org/10.3342/ceo.2008.1.1.1
25. Thornton JF, Griffin JR, Constantine FC. Nasal reconstruction: an overview and nuances. Semin Plast Surg. 2008;22(4):257-68. DOI: http://dx.doi.org/10.1055/s-0028-1095885
26. McCluskey PD, Constantine FC, Thornton JF. Lower third nasal reconstruction: when is skin grafting an appropriate option? Plast Reconstr Surg. 2009;124(3):826-35. PMID: 19730301
1. Pontifícia Universidade Católica do Rio Grande do Sul, Porto Alegre, RS, Brazil
2. Hospital São Lucas, Pontifícia Universidade Católica do Rio Grande do Sul, Porto Alegre, RS, Brazil
3. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
Institution: Hospital São Lucas, Pontifícia Universidade Católica do Rio Grande do Sul, Porto Alegre, RS, Brazil.
Corresponding author:
Renato Franz Matta Ramos
Av. Ipiranga, 6690 - Jardim Botânico
Porto Alegre, RS, Brazil Zip Code 90610-000
E-mail: renatomatta82@hotmail.com
Article received: February 4, 2016.
Article accepted: February 3, 2017.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter