

Original Article - Year 2017 - Volume 32 -
Treatment of orbital floor fracture with conchal cartilage
Tratamento de fratura de assoalho orbital com cartilagem conchal
ABSTRACT
INTRODUCTION: The reconstruction of defects in the orbital floor after fractures poses a challenge to the plastic surgeon because besides the patient's aesthetic and reconstructive expectations, possible functional complications such as diplopia and facial paresthesia must be treated. This study aimed at reporting a series of cases in which conchal auricular cartilage was used for volumetric orbital and structural replacement of the floor.
METHODS: Twenty-four patients, with surgery performed by the author, between 2013 and 2016, for pure (blow-out) or impure (conjugated to orbital margin injuries, such as zygoma and maxilla) orbital floor fractures, were evaluated. The repair technique involved autologous conchal cartilage graft in all cases. Patients were classified for the presence of preoperative complaints, including paresthesia and diplopia, and symptoms such as enophthalmia, as well as postoperative outcomes.
RESULTS: The existence of concomitant lesions, such as zygomatic complex and maxillary fracture, as well as fractures with greater discontinuity in the orbital floor, may influence the success of reconstruction. Few patients exhibited postoperative complaints and only two (9.2%) required a new surgical approach.
CONCLUSION: Autologous conchal auricular cartilage is a suitable material for reconstruction of defects in the post-fracture orbital floor, possessing various advantages, including ease of attainment, low morbidity, inconspicuous scar, and excellent adaptation to the shape of the orbital floor and consequent volumetric replacement.
Keywords: Orbit; Orbital fractures; Orbital implants.
RESUMO
INTRODUÇÃO: A reconstrução dos defeitos no assoalho orbital após fraturas constitui um desafio ao cirurgião plástico, pois além da expectativa estética e reconstrutora do paciente, cabe o tratamento de possíveis complicações funcionais, como diplopia e parestesias faciais. O objetivo é demonstrar uma série de casos utilizando cartilagem auricular conchal para reposição volumétrica orbital e estrutural do assoalho.
MÉTODOS: Foram avaliados 24 pacientes, operados pelo autor deste trabalho no período de 2013 a 2016, por motivo de fraturas de assoalho orbital pura (blow-out) ou impura (conjugadas a lesões de margem orbital, como zigoma e maxila). A técnica de estruturação do assoalho utilizou enxerto cartilaginoso autólogo conchal em todos os casos. Os pacientes foram catalogados quanto à presença de queixas pré-operatórias, como parestesia e diplopia, e sintomas, como enoftalmia, assim como resultados pós-operatórios.
RESULTADOS: A presença de lesões concomitantes como fratura de complexo zigomático e fratura maxilar pode influenciar no sucesso da reconstrução, assim como as fraturas com maior área de descontinuidade no assoalho orbital. Poucos pacientes apresentaram queixas pós-operatórias e somente dois casos (9,2%) necessitaram de nova abordagem cirúrgica.
CONCLUSÃO: A cartilagem conchal auricular autóloga é um material adequado à reconstrução de defeitos no assoalho orbital pós-fratura, apresentando como vantagens a fácil obtenção, baixa morbidade, cicatriz inconspícua, excelente adaptação ao formato do assoalho da órbita e consequente reposição volumétrica.
Palavras-chave: Órbita; Fraturas orbitárias; Implantes orbitários.
Orbital floor fractures are frequent after face trauma, usually with diplopia, hypo and enophthalmia1. Early recognition and diagnosis are important in treating this condition2.
The change of the content/continent ratio, i.e., the relationship between the eyeball, musculature, and orbital fat, and the volume of the orbit, is considered the main originating mechanism of the enophthalmia and diplopia. Although a minor cause, the atrophy of orbital contents has also been reported as an etiology of these alterations3-6.
Surgical repair aims to restore this content/continent ratio through an anatomical and functional sustainability, avoiding the recurrence of herniation of orbital contents, restoring ocular movement and orbital volume, and returning the aesthetic appearance of the face.
Following Gart & Gosain6, fractures of the orbital region should be correctly treated with reduction of the hernia tissue, release of possible entrapments of orbital fat or extraocular musculature, repositioning of bone fragments, and reconstruction of the orbital floor.
Deficient treatment may lead to complications such as restriction of ocular movement by entrapment of intraorbital fat, or extraocular muscles in fragments of fracture, or reconstruction material, diplopia, orbital dystopia, unsightly appearance, and enophthalmia, as demonstrated by Gart & Gosain6.
Reconstruction of the orbital floor can be performed using various types of materials, namely, autologous, such as septal cartilage used by Kraus et al.7,8, or conchal, used by Ozyazgan et al.9 and Castellani et al.10, and homologs and alloplastics such as the Silastic screen used in the work of Aboh et al.11. There is no definite consensus with respect to the most suitable material for the reconstruction of these fractures.
The adopted surgical access route also varies among surgeons, with the most commonly used options, being the subpalpebral, subciliary, and transconjunctival pathways12,13.
The author used the technique of conchal auricular cartilage for volumetric and structural replacement of the orbital floor, as recommended by Castellani et al.10.
This study reports an analysis of 24 patients with surgical correction of orbital floor fractures that were associated or not associated with other lesions and were treated with autologous conchal cartilage grafts.
OBJECTIVE
To report a series of cases of orbital floor fracture treated with conchal auricular cartilage for volumetric orbital replacement and restructuring of the orbital floor.
METHODS
Twenty-four patients with surgical correction of orbital floor fractures that were associated or not associated with other lesions were evaluated between March 2013 and April 2016 at Hospital Felício Rocho, Belo Horizonte, MG.
Preoperative complaints of paresthesia of the ipsilateral infraorbital territory, diplopia, and impossibility of ocular movement due to muscular incarceration were assessed. The preoperative signs evaluated were blepharohematoma, enophthalmia or hypophthalmia, loss of zygomatic eminence projection, and disocclusion.
The causes and types of fractures were evaluated.
Data were obtained from the medical records to determine sex, age, time between fracture and surgical correction, and access route of the surgical approach. The principles of Helsinki were respected.
Patients were submitted to anamnesis and physical examination during the preoperative consultation and were informed about the surgical technique, location, size and evolution of the scar, most common complications, and also the importance and necessity of postoperative care. All patients signed the Term of Free and Informed Consent.
The photographic record was completed before and after the surgical procedure. Antisepsis, antibiotic prophylaxis, hemostasis, asepsis, and minimal manipulation of the graft were rigidly observed and accomplished.
In patients with lesions exclusively in the orbital floor, a palpebral (subpalpebral or subciliar) incision was made; in patients with fractures additional to the orbital floor this was performed last.
In patients with simultaneous lesions such as naso-orbito-ethmoid (NOE) fractures, concomitant incisions, namely, cranial coronal and oral upper vestibular of Caldwell Luc incisions were made. In the treatment of zygomatic arch fractures, Gilles' temporal incisions or direct access through exposition of the coronal incision were performed. Since these fractures are outside the scope of this study, they were not extensively addressed.
The patients first returned after 7 and 14 days, and later, 1, 3, and 6 months following the procedure. All patients had a minimum follow-up period of 6 months. During this period, patients were reassessed and a postoperative photographic record was collected.
After placing the patient on the surgical table and performing appropriate asepsis and antisepsis, marking was performed, taking into consideration the size of the graft to be used and the area where it was to be inserted. All patients received general anesthesia with orotracheal intubation.
Demarcation was established with methylene blue at the limits of the auricular concha, followed by incision, and posterior and anterior subperichondrial detachment of the concha (Figure 1). All anatomical auricular units of the helix, scapula, and anti-helix were preserved during the subperichondrial detachment and resection of this cartilage.

Figure 1. Demarcation of the auricular conchal limits.
After antisepsis and placement of surgical drapes, patients received the respective incisions needed to treat their fractures.
In the cases of anterior access, the incision was made 1 mm below the transition between the concha and the ipsilateral anti-helix (Figure 2).

Figure 2. Resected concha with preservation of the perichondrium.
The graft was carefully removed to preserve the integrity of the concha.
Cartilage for the graft was always harvested from the ear on the same side of the orbital defect.
Conchal cartilage graft of the ear, obtained through anterior or posterior incision, was used in all patients.
Next, the eyelid cutaneous incision was performed. In the case of the subciliary incision, about 4 mm of orbicularis muscle corresponding to the tarsal portion was preserved, with the muscle being incised just below this portion (Figure 3). In the case of the subpalpebral incision located immediately above the inferior margin of the orbit, in the transition from the palpebral skin to the malar skin, the orbicularis muscle was sectioned in its orbital portion.

Figure 3. Orbit accessed by subciliary incision, preserving the tarsal portion of the orbicularis muscle and performing the incision of the septal portion of this muscle.
In both cases, the medial and posterior orbital lamellae were preserved, and only the anterior lamella (skin and orbicularis muscle) was incised.
After incision, the anterior lamella was succeeded by the orbital septum, which was preserved. The periosteal incision was then made on the inferior orbital margin and the subperiosteal detachment of the orbit, with complete exposure of the foci of the fracture floor.
The orbital content eventually herniated to the maxillary sinus was recovered and cephaladly rebounded by the retractors. The orbital detachment was ample for posterior positioning of the conchal cartilage.
The next step consisted of the grafting of conchal cartilage in the orbital floor, as shown in figure 4. All the foci of concomitant fractures, if any, were anatomically reduced. The reduction of any herniated orbital contents, such as orbital fat, extraocular musculature, and papyraceous bones of the floor, was performed. The fracture focus of the orbital floor was obliterated by the auricular concha after adequately adapted to the curvature of the orbit. After the grafting, the closure was completed by planes of access to the orbit, carefully closing the periosteum to avoid extrusion of the concha.

Figure 4. Filling of orbital floor with auricular conchal cartilage.
RESULTS
Twenty-four patients received surgical correction of orbital floor fractures, associated or not with other lesions. Patients included 6 women and 18 men, with ages ranging between 6 and 87 years. The average age was 40.05 years.
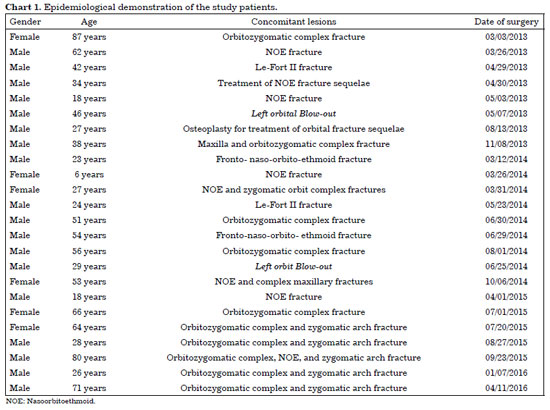
Two patients exhibited pure blow-out fractures without lesion at the orbital margins. Multiple fractures were identified in the other 22 patients, varying between simple NOE fractures, complex NOE fractures, Le Fort II fractures or orbitozygomatic complex fractures (Chart 1).
Paresthesia of the ipsilateral infraorbital territory (67%) and diplopia (21%) were the most common preoperative complaints. The impossibility of ocular movement due to muscular incarceration occurred in a single patient.
The most common preoperative signs were blepharohematoma (79%), enophthalmia or hypophthalmia (55%), loss of zygomatic eminence projection (38%), and dislocation (16%). The latter two were observed in patients with concomitant fractures in the orbitozygomatic complex or in the facial abutments.
The main causes of fracture resulted from automobile accidents (16 cases), intentional physical aggression or sports' injuries (5 cases) and ordinary falls (3 cases).
The following fractures were identified: 2 cases of pure blow-out of the orbital floor, 11 cases of floor fracture and fracture of the lateral wall of the orbit, and the other 11 cases corresponded to floor and medial orbital wall fractures.
The time between the trauma and the surgical approach to the fracture ranged between 4 and 18 days.
The access to the cartilage graft removal was retroauricular in 19 patients and anterior in 5 patients.
The access to the fracture site was transcutaneous in all cases and favored incision in 20 patients was the subciliary incision, which was made 1-2 mm below the ciliary border of the inferior palpebral, preserving the orbicularis muscle in its tarsal portion. A subpalpebral incision, located in the palpebral skin transition to the malar skin, directly above the orbital margin, was performed in 4 patients. A transconjunctival incision was not made in any patient.
The following (common) postoperative complications were observed: 11 patients exhibited blepharohematoma; 9 patients showed residual paresthesia of the infraorbital territory (with complete resolution after 6 months in all cases), and 1 patient with residual diplopia, required a new surgical approach and contralateral conchal cartilage grafting to restore the orbital content/continent ratio.
One patient showed retro-orbital hematoma with orbital compartment syndrome in the immediate postoperative period, being identified before anesthetic awakening and promptly treated with hematoma evacuation, hemostasis, and orbital decompression, without the need for a canthotomy.
There were no other postoperative or transoperative complications.
The period of hospitalization ranged between 1 and 18 days.
Two patients exhibited a palpable graft at the orbital margin and a new approach was required to improve the graft insertion in the orbit and closure of the margin periosteum, thus avoiding new extrusion. The patients evolved without intercurrences afterwards.
There was no significant complaint about the conchal graft donor sites and no case of surgical site infection.
Patients indicated high levels of satisfaction in the postoperative period, with a return to normal activities after an average period of 21 days.
The aesthetic results of the treatment of orbital floor fractures with auricular conchal cartilage were well received by the patients, with no specific complaints regarding facial scars, auricular (pre or retroauricular) or facial (hypo/enophthalmia and telecanthus) (Figures 5-10).

Figure 5. A 23-year-old patient with nasoorbitoethmoid fracture, traumatic telecanthus, and bilateral orbital floor fracture, after automobile accident.
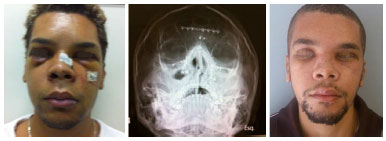
Figure 6. Previous patient . Radiography with reconstruction of facial abutments and symmetrical orbital structures, and with similar volumes in the initial and late postoperative period.

Figure 7. A 53-year-old patient with complex facial NOE associated with Le Fort II, destruction of orbital floor and floating palate, submitted to oral treatment by degloving to treat facial abutments, followed by bilateral subciliary incisions for treatment of orbital margins and floors.

Figure 8. Late postoperative patient showing excellent facial volumetric replacement with bilateral orbits, absence of telecanthus, no visual complaints, and absence of complaints with respect to bilateral subciliary scars; Panoramic radiography; anatomical reconstruction of the face with symmetrical and normal positions of the orbits and occlusion in class I in the midline, denoting correct reconstruction of the facial abutments.

Figure 9. A 27-year-old patient with nasoorbitoethmoid and right orbitozygomatic complex fracture after automobile accident. Patient received a subciliary incision and removal of auricular concha and grafting of conchal cartilage on the floor orbital, after treatment of orbital margin fracture.

Figure 10. Previous patient . Immediate and late postoperative, exhibiting inconspicuous scars, good ocular alignment, normal intercanthal distance, and absence of complaints or symptoms, such as paresthesia and diplopia.
Pre- and Post-Operative (Figures 5 to 10)
The patients first returned after 7 and 14 days and later 1, 3, and 6 months, after the procedure. All patients had a minimum follow-up period of 6 months. During this period, patients were reassessed and a postoperative photographic record was collected.
DISCUSSION
The treatment of orbital floor fractures is an evolving field14. It is known that, regardless of the material adopted, the reconstruction must be anatomical, avoiding extreme rigidity of the orbital floor, as achieved in reconstructions with metallic screens or thick bone. This is well documented in cases of recurrence of lesions in the same eye, in which increased pressure associated with trauma caused by rigidity of the reconstructed orbital floor, resulted in an ocular lesion and amaurosis; this is described by Costa, one of the pioneers of craniomaxillofacial surgery in Brazil, in the book by Melega et al.15.
Autologous materials such as bone, cartilage, fascia, and periosteum have the advantage of reduced infection rates and low cost. By contrast, these materials have the disadvantage of increasing the surgical time and the morbidity associated with complications in the donor site6,14. Among the autologous materials, the most commonly used in the orbital floor are cartilage and bone.
Homologous materials have advantages similar to the autologous. However, despite being easily obtained without morbidity in the donor area, they show higher rates of infection, absorption, and loss6,14.
Alloplastic materials in turn, reduce the surgical time but increase the probability of infection, rejection, fistulas, cysts, and treatment costs. Most studies have shown fewer complications with autologous grafts than with synthetic ones6,14.
The choice of the material used in the reconstruction of the floor of the orbit was motivated by the low morbidity in the donor area and its biocompatibility. Furthermore, because of the greater morbidity, surgical time, potential non-anatomical reduction due to excess orbital floor stiffness, and absorption rates in bone grafting, reconstruction with cartilaginous graft, rather than the other possible reconstruction choices, was the preferred procedure in this study.
Among the various sources of autologous cartilage, the nasal septum, auricular concha, and costal arches were chosen in this study. The cartilage is more viable, as nutrition does not require direct contact, in opposition to the bones. The septal and conchal cartilages have similar absorption indexes11,16.
Despite its proven viability and efficiency septal cartilage is less used. Greater morbidity of the donor area and possibility of complications such as septal perforation and contaminated airway discouraged its use here, as compared with conchal cartilage.
According to Talesh et al.17 and Özyazgan et al.9, auricular cartilage is highly recommended for reconstruction of defects in the orbital floor; this is because of its shape equivalence, ideal flexibility, satisfactory resistance to support the orbital content, decompression and agility with which it can be withdrawn, small morbidity in the donor region, and no aesthetic deformity of the donor area.
Removal of the graft should be carefully done to preserve the integrity of the concha, as this should be fully used in monoblock for better occlusion of the floor defect.
The conchal cartilage graft from the ear was used in all patients and its extraction was performed by anterior or posterior incision. Anterior incision was used only in 5 patients. This was abandoned due to the poorer esthetic effect, since although inconspicuous, it is more visible than the posterior incision.
The results obtained here with conchal cartilage graft demonstrated the reliability of the method as well as a low index of complications in the donor area and good restoration of the orbital content/continent ratio.
The absence of cases of residual enophthalmia also demonstrated the reliability of the conchal graft in maintaining the orbital content of herniations to the ipsilateral maxillary sinus. The concave shape of conchal cartilages presents better adaptability to the orbit, relative to septal cartilages, and helps the anatomical reconstruction of the orbital cavity, which exhibits a conical shape with postero-superior apex10,18,19.
The proximity of the surgical sites, between the donor and recipient sites, allows the simultaneous access by two surgical teams, reducing surgical time and operative morbidity.
In addition, because the subpalpebral incision is performed directly on the orbital margin, it allows rapid and direct access to the fracture focus, although with worse aesthetic results. The subciliary incision is a transcutaneous access option, which is technically more complicated than the subpalpebral one, although, with better esthetic results than the latter.
The transconjunctival pathway has the advantage of not involving cutaneous incision; however, it is technically more complex than the previous two. Moreover, it often requires adjuvant lateral cannulation for better access and exposure, especially in fractures of orbitozygomatic complex and inferolateral orbital wall, as popularized by Tessier12 and previously introduced by Bourguet13.
The transcutaneous, subciliary or subpalpebral access20,21 shows good aesthetic results and seems to be one of the reasons for the absence of significant postoperative complaints in any of the cases.
It is essential for the grafting of conchal cartilage on the orbital floor that all the foci of concomitant fractures, if existent, are anatomically reduced. Equally important is the reduction of any orbital contents eventually herniated such as orbital fat, extraocular musculature, and papyraceous bones of the floor.
The fracture focus of the orbital floor should be obliterated by the auricular concha, which adapts well to the orbital curvature, due to its natural curvature, preventing the recurrence of herniation of the contents to the maxillary sinus.
As in any surgical procedure, this technique requires adequate anatomical knowledge, fundamental to reduce postoperative complications and to achieve effective results, in addition to providing a better recovery.
This work aimed at demonstrating the results of the orbital floor reconstruction technique, with the goal of achieving a more adequate result in the use of conchal auricular cartilage for volumetric orbital and structural replacement of the floor.
This technique involved minimal complications in the donor area, good restoration of the orbital content/continent ratio, and excellent correction of the reconstruction of the orbit floor.
CONCLUSIONS
Conchal cartilages are an excellent choice in the reconstruction of the orbit floor, presenting minimal morbidity in the donor site and anatomical reconstruction of the orbital contents/continent ratio, with excellent adaptation of the concha graft to the orbital wall, allowing anatomical reduction.
This procedure involving the use of eyelid cutaneous incisions and reconstruction with auricular concha graft represents an adequate treatment12,13,24.
The method demonstrated good reproducibility without great grafting technical difficulty and little or no morbidity of the donor area.
The method is safe, reproducible, with low complication rates and high satisfaction rates, thus being a good option for the reconstruction of the post-fracture orbital floor22.
COLLABORATIONS
WCNBP Analysis and interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; performance of experiments; writing the manuscript or critical review of its contents.
ICO Analysis and interpretation of data; statistical analyses; performance of experiments; writing the manuscript and critical review of its contents.
DSOA Analysis and interpretation of data; completion of surgeries.
MTRPF Analysis and interpretation of data; completion of surgeries.
MHLR Analysis and interpretation of data; completion of surgeries.
GMCS Completion of surgeries; writing the manuscript and critical review of its contents.
SMC Final approval of the manuscript; conception and design of the study; completion of surgeries; critical review of its contents.
KRO Analysis and interpretation of data; performance of experiments.
REFERENCES
1. Beigi B, Khandwala M, Gupta D. Management of pure orbital floor fractures: a proposed protocol to prevent unnecessary or early surgery. Orbit. 2014;33(5):336-42. PMID: 24987818 DOI: http://dx.doi.org/10.3109/01676830.2014.902475
2. Harris GJ. Avoiding complications in the repair of orbital floor fractures. JAMA Facial Plast Surg. 2014;16(4):290-5. DOI: http://dx.doi.org/10.1001/jamafacial.2014.56
3. Chua DY, Lo S. Orbital fracture in a professional diver: issues and management. J Maxillofac Oral Surg. 2015;14(Suppl 1):81-3. DOI: http://dx.doi.org/10.1007/s12663-011-0315-9
4. Bartoli D, Fadda MT, Battisti A, Cassoni A, Pagnoni M, Riccardi E, et al. Retrospective analysis of 301 patients with orbital floor fracture. J Craniomaxillofac Surg. 2015;43(2):244-7. PMID: 25547215 DOI: http://dx.doi.org/10.1016/j.jcms.2014.11.015
5. Gunarajah DR, Samman N. Biomaterials for repair of orbital floor blowout fractures: a systematic review. J Oral Maxillofac Surg. 2013;71(3):550-70. DOI: http://dx.doi.org/10.1016/j.joms.2012.10.029
6. Gart MS, Gosain AK. Evidence-based medicine: Orbital floor fractures. Plast Reconstr Surg. 2014;134(6):1345-55. PMID: 25415098 DOI: http://dx.doi.org/10.1097/PRS.0000000000000719
7. Kraus M, Gatot A, Kaplan DM, Fliss DM. Post-traumatic orbital floor reconstruction with nasoseptal cartilage in children. Int J Pediatr Otorhinolaryngol. 2002;64(3):187-92. PMID: 12090946 DOI: http://dx.doi.org/10.1016/S0165-5876(02)00013-7
8. Kraus M, Gatot A, Fliss DM. Repair of traumatic inferior orbital wall defects with nasoseptal cartilage. J Oral Maxillofac Surg. 2001;59(12):1397-400. DOI: http://dx.doi.org/10.1053/joms.2001.28265
9. Ozyazgan I, Eskitaşçioğlu T, Baykan H, Coruh A. Repair of traumatic orbital wall defects using conchal cartilage. Plast Reconstr Surg. 2006;117(4):1269-76. PMID: 16582799 DOI: http://dx.doi.org/10.1097/01.prs.0000208301.69547.8b
10. Castellani A, Negrini S, Zanetti U. Treatment of orbital floor blowout fractures with conchal auricular cartilage graft: a report on 14 cases. J Oral Maxillofac Surg. 2002;60(12):1413-7. DOI: http://dx.doi.org/10.1053/joms.2002.36094
11. Aboh IV, Chisci G, Gennaro P, Giovannetti F, Bartoli D, Priore P, et al. Complications of orbital floor repair with silastic sheet: the skin fistula. J Craniofac Surg. 2013;24(4):1288-91. DOI: http://dx.doi.org/10.1097/SCS.0b013e318293f921
12. Tessier P. The conjunctival approach to the orbital floor and maxilla in congenital malformation and trauma. J Maxillofac Surg. 1973;1(1):3-8. DOI: http://dx.doi.org/10.1016/S0301-0503(73)80005-0
13. Bourguet J. Les lernies graissenses de l'orbite: Notre traitement chirurgical. Bull Acad Med (Paris). 1924;92:1270-2.
14. Aldekhayel S, Aljaaly H, Fouda-Neel O, Shararah AW, Zaid WS, Gilardino M. Evolving trends in the management of orbital floor fractures. J Craniofac Surg. 2014;25(1):258-61. DOI: http://dx.doi.org/10.1097/SCS.0000000000000441
15. Melega JM, Viterbo F, Mendes FH. Cirurgia plástica: os princípios e a atualidade. Rio de Janeiro: Guanabara Koogan; 2011.
16. Bayat M, Momen-Heravi F, Khalilzadeh O, Mirhosseni Z, Sadeghi-Tari A. Comparison of conchal cartilage graft with nasal septal cartilage graft for reconstruction of orbital floor blowout fractures. Br J Oral Maxillofac Surg. 2010;48(8):617-20. DOI: http://dx.doi.org/10.1016/j.bjoms.2009.10.019
17. Talesh KT, Babaee S, Vahdati SA, Tabeshfar S. Effectiveness of a nasoseptal cartilaginous graft for repairing traumatic fractures of the inferior orbital wall. Br J Oral Maxillofac Surg. 2009;47(1):10-3. DOI: http://dx.doi.org/10.1016/j.bjoms.2008.04.017
18. Tong L, Bauer RJ, Buchman SR. A current 10-year retrospective survey of 199 surgically treated orbital floor fractures in a nonurban tertiary care center. Plast Reconstr Surg. 2001;108(3):612-21. DOI: http://dx.doi.org/10.1097/00006534-200109010-00003
19. Rinna C, Ungari C, Saltarel A, Cassoni A, Reale G. Orbital floor restoration. J Craniofac Surg. 2005;16(6):968-72. DOI: http://dx.doi.org/10.1097/01.scs.0000186308.16795.8b
20. Manganello-Souza LC, Rodrigues de Freitas R. Transconjunctival approach to zygomatic and orbital floor fractures. Int J Oral Maxillofac Surg. 1997;26(1):31-4. DOI: http://dx.doi.org/10.1016/S0901-5027(97)80843-0
21. Kothari NA, Avashia YJ, Lemelman BT, Mir HS, Thaller SR. Incisions for orbital floor exploration. J Craniofac Surg. 2012;23(7 Suppl 1):1985-9. DOI: http://dx.doi.org/10.1097/SCS.0b013e31825aaa03
22. Jaquiéry C, Aeppli C, Cornelius P, Palmowsky A, Kunz C, Hammer B. Reconstruction of orbital wall defects: critical review of 72 patients. Int J Oral Maxillofac Surg. 2007;36(3):193-9. DOI: http://dx.doi.org/10.1016/j.ijom.2006.11.002
1. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
2. Associação Brasileira de Cirurgia Crânio-Maxilo-Facial, São Paulo, SP, Brazil
3. Hospital Felício Rocho, Belo Horizonte, MG, Brazil
Institution: Hospital Felício Rocho, Belo Horizonte, MG, Brazil.
Corresponding author:
Waldemar Chaves Nascimento Brandao Penna
Av. do Contorno, 9530 - Santa Efigênia
Belo Horizonte, MG, Brazil Zip Code 30110-017
E-mail: waldemarpenna@gmail.com
Article received: September 13, 2016.
Article accepted: October 10, 2016.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter