

Original Article - Year 2017 - Volume 32 -
Innervation of the nipple-areolar complex after reduction mammaplasty: a histological study
Inervação do complexo areolopapilar após mamoplastia redutora: estudo histológico
ABSTRACT
INTRODUCTION: The periareolar dermal release maneuver in mammoplasty promotes better mobility of the nipple-areola complex. However, there are doubts on possible nerve damages in this kind of topography. This quantitative analysis compared the nerve branches density from the medial, lateral and caudal side-flow of the nipple-areola complex (NAC).
METHODS: This was a prospective study. The study included 26 women who have undergone a mammaplasty reduction using the Pitanguy's classic technique. The dermis fragments collected from the medial, lateral and caudal sides were properly prepared and subjected to a histological study in order to determine the nerve branches density in each studied sides.
RESULTS: Of 26 studied patients, 42.3% had a higher nerve branches density in the lateral side; 38.5%, on the medial side and 19.2% on the caudal side. The statistical analysis used to evaluate whether there was a predominance of one side where the dermis has been sectioned showed that the proportion comparison test was not significant (p = 0.304).
CONCLUSION: The comparative analysis has shown that there is no preponderance of nerve density in any periareolar dermis side.
Keywords: Mammaplasty; Histology; Anatomy.
RESUMO
INTRODUÇÃO: A manobra de liberação dérmica periareolar na mamoplastia promove uma melhor mobilidade do complexo mamilo-aréola (NAC). No entanto, existem dúvidas sobre possíveis danos nos nervos neste tipo de topografia. Este estudo objetiva uma análise quantitativa comparando a densidade dos nervos do fluxo lateral medial, lateral e caudal do NAC.
MÉTODOS: Trata-se de um estudo prospectivo. O estudo incluiu 26 pacientes do sexo feminino que foram submetidas à mamoplastia redutora pela técnica clássica de Pitanguy. Os fragmentos da derme coletados dos lados medial, lateral e caudal foram devidamente preparados e submetidos a um estudo histológico para determinar a densidade dos nervos em cada um dos lados estudados.
RESULTADOS: Dos 26 pacientes estudados, 42,3% apresentaram maior densidade de nervos no lado lateral; 38,5%, do lado medial e 19,2% do lado caudal. A análise estatística utilizada para avaliar se houve predominância de um lado onde a derme foi seccionada demonstrou que o teste de comparação de proporções não foi significativo (p = 0,304).
CONCLUSÃO: A análise comparativa mostrou que não há preponderância de densidade de nervos em qualquer lado da derme periareolar.
Palavras-chave: Mamoplastia; Histologia; Anatomia.
Surgical procedures in the thorax are subject to important skin nerves damage in the breast area, areola and nipple1. The nipple is a sensitive unit with an erectile function and it is important part of the woman intimacy with significant impact in their psychological and sexual health2.
A number of studies have been proposed to identify the safe zone for breast resection and maximal preservation of breast innervation1-5.
However, existing studies are controversial on distribution and pathway that these nerves take up to the nipple-papillary complex (NAC)2.
In the plastic surgery department of the Federal University of Pernambuco a project is under analysis in order to evaluate dermal release maneuver in patients undergoing breast reduction. The main advantage observed is: greater mobility of the NAC. However, there are doubts about possible nerve damage in this topography4,6-10.
OBJECTIVE
This study proposes a quantitative and comparative histological analysis about the nerve density in the medial, lateral and caudal side of the periareolar dermis.
METHODS
The survey was conducted in the Hospital das Clínicas of the Federal University of Pernambuco (HC-UFPE) in Recife, PE, Brazil. The study was previous approved by Ethical and Research Committee, number ACEE: 05351312.3.0000.5208. This is a prospective study conducted from 2013-2015 in which 26 women were selected, patients aged ranged from 21 to 50 years who were admitted to the plastic surgery clinic with complaints of ptosis or breast hypertrophy. We excluded those with comorbidities, body mass index (BMI) above 30, menopausal or psychiatric disorders (assessed with the mini-mental state examination).
All patients underwent Pitanguy breast reduction11,12 under general anesthesia, and they were operated on by the same surgeon.
The finished periareolar decortication, in which area was previously marked according to each case, initiated the release of periareolar dermis. The procedure was performed with a scalpel blade 15, approximately 0.5 cm of normal skin around the decorticated area, most of the dermis was kept in contact with NAC. After the dermal release, dermal fragments were harvested with approximately 5 cm in length, from the medial, lateral and caudal periareolar dermal area and forwarded to histological analysis (Figure 1).
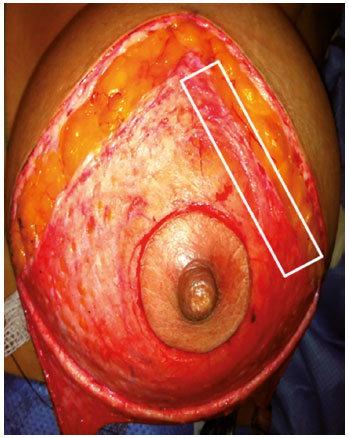
Figure 1. Sectioned dermis on the lateral and medial sides (dermal release maneuver) after decortication. The marked area shows lateral segment of dermal sample that was collected.
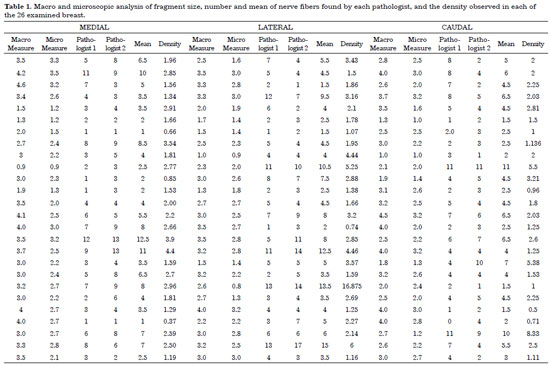
Samples forwarded to histopathological analysis were technical processed with histological sections of 5 µms and stained with hematoxylin and eosin. Samples were analyzed by two pathologists at different times. The nerve fillets amount was obtained by counting by optic microscopy at 100 times magnification. The macroscopic measurement of the specimen and histological processing (microscopic measurement) were considered.
Based on data obtained, we calculated nerve density was calculated by dividing the average number of threads found by the two pathologists on the micro sample measurement (after histological processing) and thus found the number of nerve fillets per square centimeters (cm2) . A comparison of the nerve thickness was done among medial, lateral and caudal side.
Data were typed into a Microsoft Excel spreadsheet exported to SPSS software, version 18, for analysis. In the evaluation of prevalence of side with highest density we calculated the percentage frequency, and constructed the frequency distribution. The comparison of prevalence was performed using the chi-squared test to compare proportions, and to calculate the confidence interval to prevalence found. The conclusion of the analysis considered a significance level of 5%.
RESULTS
Results of histological analysis of 26 breast are shown in table 1.
Figure 2 shows quantity of patients related with density of nervous fillets found in each analyzed side.
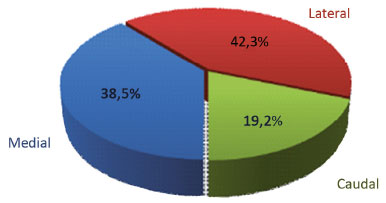
Figure 2. Number of patients related to density of nerve branches found in each analyzed side.
Statistical data analysis used the Chi-squared test with confidence intervals to analyze each side, which is observed in table 2. We used a significance level of 5% (p < 0.05).
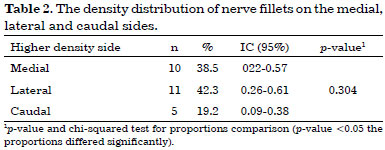
Even when higher prevalence in lateral side was seen, confidence intervals from three evaluated parts submitted to present intersections indicating similarity among prevalence of women with higher density on the medial, lateral and caudal side. Still, we observed that proportion comparison test was not significant (p = 0.304).
No cases of partial or total areola necrosis were seen among studied patients.
DISCUSSION
Maintaining the nerve fibers integrity that gives sensitivity to the NAC that is a reason for plastic surgeon who are active work in this area.
Since 1840, with Cooper, apud Munhoz13, several authors have tried to describe what kind of nerves were these and what its pathway until it reaches the nipple-papillary complex. However, the various studies written so far present some controversies, particularly concerning to the path that these nerves travel to reach the NAC.
Main anatomical studies seem to agree that innervation of the NAC comes from 3rd, 4th and 5th intercostal nerves, in which the 4th, is the most important of them. This nerve is divided into two major branches, the anterior cutaneous branch, which emerges from the upper-side region of the sternum and follows a shallow downward pathway toward super and medial edge of the areola; and the lateral cutaneous branch.
This latter emits a surface segment, making a subcutaneous path toward lower medial edge of the NAC, and a deep branch, which emerges in the mid-axillary line height and passes adjacent to the fascia of the pectoralis major muscle to the midclavicular line, in which makes an angle of almost 90 degrees, ascending through the breast tissue and ending at the back of the NAC3-5.
Schlenz et al.3 after anatomical dissection of 28 female cadavers and found a frequency of the lateral cutaneous branch in 93% of breasts, as well as a large-caliber nerves. Therefore, they considered it the most important nerve to the sensitivity of the nipple-papillary complex.
Riccio et al.2 recommended a careful resection of the lower side quadrant of the breast, considered as an unsafety area, because this region would own the most reliable innervation of the breast, through the lateral cutaneous branch.
Based on these studies, which is assigned to the lateral cutaneous branch of greater relevance, explain the fact that our study found a higher density of nerve branches in the dermis side periareolar. This finding, however, is not accompanied by a statistically significant difference (p = 0.304).
Sarhadi et al.4 held tangential and transverse histological sections on the areola and they observed that even deep lateral cutaneous branch fibers ascending through the breast perpendicularly on the breast tissue does not culminate immediately on the posterior face of the areola, but in its adjacent dermis, contributing to the formation of subdermal plexus and thus for the random distribution of the input fibers to the NAC pathway.
This study great part of the dermis surrounding the areola was preserved, since the incisions were performed to release dermal already closed to the skin surrounding the decorticated area. According to Sarhadi et al.4, therefore, the area that received innervation from this important nerve branch was preserved.
Our results lead to consider innervation of periareolar dermis, unlike studies reported in the literature that describe the pathway of nerves in subcutaneous plane. This fact, if on one hand it reveals the originality of the research, on the other hand it makes difficult the literature comparison.
Since it was described in 1930, the Schartzman maneuver14 that demands decortication with preservation of periareolar dermis that has been considered as fundamental to vascularization of NAC in the different choices of techniques used for breast reduction.
In Brazil, breast reduction technique developed by Arie and modified by Pitanguy11,12 is probably the most widely used and taught to plastic surgery residents.
In cases where there is a need for extensive mobilization of NAC, or when the breast presents a firm parenchyma, with little slippage of the overlying and adjacent skin, periareolar dermis imposes limitations on mobilization of the NAC during breast reduction surgery, the technique described above. Another difficulty observed in patients with these characteristics is to maintain the circular shape of the NAC, aesthetically influencing the result. The dermal release maneuver was designed as an alternative to overcome such difficulties. However, when the maneuver is performed to periareolar dermal release, a fear exist on compromising vascularization and, therefore, innervation of NAC.
Results of this study showed that there is no side with a preponderance of nerve branches (p = 0.304), thus, the dermal release does not compromise the section of a side which is predominant in relation to the density of nerve endings to NAC.
Another fact to consider is that the section is limited to the dermis. There is no way to ensure that the sectioned nerve branches at this level are sensory or motor. The studies found describe the main nerves responsible for the sensitivity of NAC in the subcutaneous level and not in the dermis where the maneuver releasing is done.
Counting of nerve fillets was performed by two pathologists, and ultimate result was the average of these values. Such care is justified to reduce the possibility of the same nervous fillets have been considered more than once.
Although not objective of this study, it is important to report that no case observed the appearance of areola necrosis, whether partial or total, among 26 patients who underwent surgery. The analysis of this result, as well as the objective measurement of sensitivity done with Semmes-Weinstein monofilaments, which are part of the study under final phas, and conducted by the same group of researchers.
CONCLUSION
The comparative analysis has shown that there is no preponderance density of nerve fillets in any side of periareolar dermis.
COLLABORATIONS
JZS Analysis and/or interpretation of data; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
OMLP Completion of surgeries and/or experiments.
FAMBA Completion of surgeries and/or experiments.
DMT Completion of surgeries and/or experiments.
JMP Completion of surgeries and/or experiments.
ATC Writing the manuscript or critical review of its contents.
RA Completion of surgeries and/or experiments.
JLAA Analysis and/or interpretation of data.
AEOR Final approval of the manuscript; conception and design of the study.
REFERENCES
1. Jaspars JJ, Posma AN, van Immerseel AA, Gittenberger-de Groot AC. The cutaneous innervation of the female breast and nipple-areola complex: implications for surgery. Br J Plast Surg. 1997;50(4):249-59. DOI: http://dx.doi.org/10.1016/S0007-1226(97)91155-3
2. Riccio CA, Zeiderman MR, Chowdhry S, Brooks RM, Kelishadi SS, Tutela JP, et al. Plastic Surgery of the Breast: Keeping the Nipple Sensitive. Eplasty. 2015;15:e28.
3. Schlenz I, Kuzbari R, Gruber H, Holle J. The sensitivity of the nipple-areola complex: an anatomic study. Plast Reconstr Surg. 2000;105(3):905-9. PMID: 10724249 DOI: http://dx.doi.org/10.1097/00006534-200003000-00012
4. Sarhadi NS, Shaw Dunn J, Lee FD, Soutar DS. An anatomical study of the nerve supply of the breast, including the nipple and areola. Br J Plast Surg. 1996;49(3):156-64. PMID: 8785595 DOI: http://dx.doi.org/10.1016/S0007-1226(96)90218-0
5. Sarhadi NS, Shaw-Dunn J, Soutar DS. Nerve supply of the breast with special reference to the nipple and areola: Sir Astley Cooper revisited. Clin Anat. 1997;10(4):283-8. DOI: http://dx.doi.org/10.1002/(SICI)1098-2353(1997)10:4<283::AID-CA12>3.0.CO;2-G
6. Craig RD, Sykes PA. Nipple sensitivity following reduction mammaplasty. Br J Plast Surg. 1970;23(2):165-72. PMID: 5464107 DOI: http://dx.doi.org/10.1016/S0007-1226(70)80034-0
7. Farina MA, Newby BG, Alani HM. Innervation of the nipple-areola complex. Plast Reconstr Surg. 1980;66(4):497-501. PMID: 7208664 DOI: http://dx.doi.org/10.1097/00006534-198010000-00001
8. Gonzalez F, Brown FE, Gold ME, Walton RL, Shafer B. Preoperative and postoperative nipple-areola sensibility in patients undergoing reduction mammaplasty. Plast Reconstr Surg. 1993;92(5):809-14. DOI: http://dx.doi.org/10.1097/00006534-199392050-00005
9. Aboudib JH, Roxo ACW. Avaliação dos resultados tardios de mamoplastia redutora pela técnica periareolar. Rev Bras Cir Plást. 2011;26(1):74-80. DOI: http://dx.doi.org/10.1590/S1983-51752011000100016
10. Souza AA, Faiwichow L, Ferreira AA, Simão TS, Pitol DN, Máximo FR. Avaliação das técnicas de mamoplastia quanto a sua influência tardia na distância do complexo areolopapilar ao sulco inframamário. Rev Bras Cir Plást. 2011;26(4):664-9. DOI: http://dx.doi.org/10.1590/S1983-51752011000400022
11. Ronconi RC, Vieira FA, Boechat CEJ, Nunes PSMR, Aboudib JHC, Castro CC. Estudo Retrospectivo de 730 Pacientes Submetidas a Mamaplastia Redutora. Rev Bras Cir Plást. 2004;19(2):58-62.
12. Kaluf R, Azevêdo FN, Rodrigues LO. Sistemática Cirúrgica em Pacientes Ex-Obesos. Rev Bras Cir Plást. 2006;21(3):166-74.
13. Munhoz AM. Viabilidade anátomo-clínica da utilização dos vasos perfurantes do músculo peitoral maior como pedículo receptor na reconstrução mamária imediata e tardia com microcirurgia [Tese de doutorado]. São Paulo: Universidade de São Paulo; 2006.
14. Miró AL. Tratamento das Ptoses Mamárias com Retalhos Cruzados sem Prévia Ressecção de Pele. Rev Bras Cir Plást. 2000;15(1):32-4.
1. Universidade Federal de Pernambuco, Recife, PE, Brazil
2. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
3. Hospital das Clínicas, Universidade Federal de Pernambuco, Recife, PE, Brazil
Institution: Hospital das Clínicas, Universidade Federal de Pernambuco, Recife, PE, Brazil.
Corresponding author:
Jairo Zacche de Sá
Av República do Libano, 251, Bloco A, sala 903 - Pina
Recife, PE, Brazil Zip Code 51110-160
E-mail: jairozacche@gmail.com
Article received: March 9, 2017.
Article accepted: April 23, 2017.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter